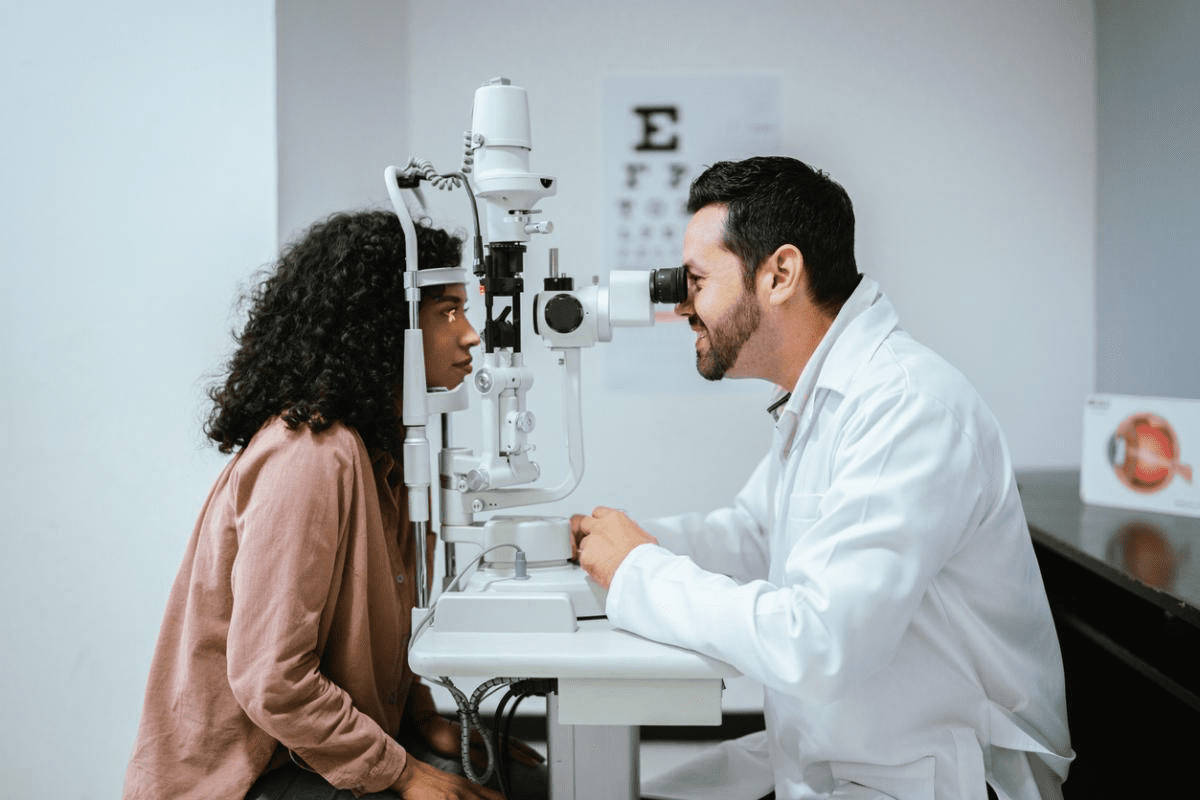
Autoimmune eye diseases are a big problem worldwide, affecting millions. When an autoimmune disease strikes, the immune system attacks healthy cells. This can harm any part of the body, including the eyes.Are your red eyes autoimmune related? Discover 7 alarming causes, symptoms, and the essential treatments that bring relief.
Studies show that autoimmune disorders can affect every part of the eye. This includes the retina inside and the muscles on the outside. Knowing about these conditions is key to managing and treating them.
We will look at seven main autoimmune eye disorders. We’ll cover their symptoms, causes, and treatments. This will give you a clear picture of these conditions and how they affect your vision.
Key Takeaways
- Autoimmune eye diseases are a significant concern worldwide, affecting millions.
- These conditions occur when the immune system mistakenly attacks healthy eye tissues.
- Every part of the eye can be impacted by autoimmune disorders.
- Understanding autoimmune eye diseases is critical for effective management.
- Early detection and treatment can make a big difference in saving your sight.
Understanding Autoimmune Eye Diseases

Autoimmune eye conditions happen when the body’s immune system attacks healthy eye tissues. This can harm vision and eye health. These diseases can greatly affect a person’s life quality.
What Are Autoimmune Eye Diseases?
Autoimmune eye diseases happen when the immune system mistakenly attacks healthy eye tissues. This can cause inflammation and damage to important parts like the retina and optic nerve.
People with these diseases may see blind spots, blurred vision, or double vision. How these symptoms show up can differ from person to person.
How Autoimmune Conditions Affect the Eyes
Autoimmune conditions can harm the eyes in many ways. For example, Graves’ disease can cause thyroid eye disease in up to 50% of patients. Sjögren’s syndrome can lead to severe dry eye in 94% of those with primary SS.
Uveitis is another condition that can cause blurred vision and eye pain. Knowing how these conditions affect the eyes is key to finding good treatments.
Autoimmune Condition | Ocular Manifestation | Prevalence |
Graves’ Disease | Thyroid Eye Disease | Up to 50% |
Sjögren’s Syndrome | Severe Dry Eye | 94% in primary SS patients |
Uveitis | Blurred Vision, Eye Pain | Varies |
Understanding how autoimmune conditions affect the eyes helps doctors give better treatments. This can lead to better results for patients.
The Rising Prevalence of Autoimmune Eye Disorders

Autoimmune eye disorders are becoming more common worldwide. They affect millions of people, leading to serious vision problems if not treated. This is a big concern for public health.
In recent decades, we’ve seen a big increase in autoimmune eye issues. Research shows that autoimmune diseases have grown from 3.2% in the 1960s to 19.1% in 2018. This rise is alarming and needs more study.
Global Statistics and Trends
The market for autoimmune disease treatments is expected to hit $6.3 billion by 2026. This shows the growing problem of these diseases. Eye-related issues are a big part of this, with conditions like uveitis and thyroid eye disease becoming more common.
Autoimmune eye conditions vary by region. Some groups are more likely to get them. For example, genetic factors are key in developing these diseases. People with a genetic risk are more likely to face eye problems.
Risk Factors for Developing Autoimmune Eye Conditions
Several things can increase your risk of getting autoimmune eye conditions. These include genetic predisposition, environmental triggers, and other autoimmune diseases. Knowing these risks helps with early detection and prevention.
People with a family history of autoimmune diseases are at higher risk. Environmental factors like toxins or infections can also trigger these diseases in some.
To lower your risk of autoimmune eye problems, it’s important to be aware of risk factors. Regular eye exams, a healthy lifestyle, and managing other autoimmune conditions are key steps.
Graves’ Disease and Thyroid Eye Disease
Graves’ disease is a complex autoimmune disorder that affects the thyroid gland. It often impacts the eyes significantly. This condition is closely linked to thyroid eye disease, a serious eye problem.
Symptoms and Ocular Manifestations
Thyroid eye disease, a common issue in Graves’ disease, affects up to 50% of patients. It causes a variety of eye symptoms. These include bulging eyes (exophthalmos), double vision (diplopia), redness, swelling, and sensitivity to light.
The symptoms can range from mild discomfort and dryness to severe inflammation and vision loss. It’s important to understand these symptoms for early diagnosis and effective treatment.
Causes and Risk Factors
Graves’ disease is caused by an abnormal immune response. This response makes the thyroid gland produce too much thyroid hormone. The exact triggers are not fully understood, but genetic predisposition and environmental factors, such as smoking, play a big role.
Risk factors for thyroid eye disease include being female, smoking, and having a history of Graves’ disease. Identifying these risk factors early can help in preventive care and monitoring.
Treatment Options and Management
Managing Graves’ disease and thyroid eye disease requires a multi-faceted approach. Treatment options include medications to reduce thyroid hormone production or alleviate eye symptoms. In severe cases, surgery may be needed.
We stress the importance of a complete treatment plan. This includes lifestyle adjustments and regular monitoring. It helps manage symptoms effectively and prevent long-term complications.
Sjögren’s Syndrome and Severe Dry Eye
Sjögren’s syndrome is a chronic autoimmune disorder that severely affects the eyes. It causes dry eye in many patients. This happens because the exocrine glands, like the lacrimal gland, don’t work right.
Recognizing Sjögren’s Eye Symptoms
The main symptoms of Sjögren’s in the eyes are dryness. Severe dry eye is seen in almost 94% of those with primary Sjögren’s. It makes eyes feel uncomfortable, blurry, and like there’s something in them.
People often say their eyes feel dry or gritty. They might see blurry or have trouble focusing. They might also feel light hurts their eyes or get tired easily.
Underlying Causes
The main reason for dry eye in Sjögren’s is the damage to the lacrimal gland. This gland makes tears. When it’s damaged, not enough tears are made, or the tears aren’t good for the eyes.
Inflammation is a big part of Sjögren’s. It causes the gland damage and leads to dry eye symptoms.
Treatment Approaches
Dealing with severe dry eye in Sjögren’s needs a few steps. Treatment options include:
- Artificial tears and eye drops to help with natural tears
- Punctal plugs to keep tears in the eyes
- Anti-inflammatory meds to fight inflammation
- Restasis or other meds to make more tears
We stress the need for a full treatment plan. It should tackle symptoms and the autoimmune issue. This helps improve life for those with Sjögren’s syndrome.
Uveitis: Inflammation of the Eye’s Middle Layer
Uveitis is a serious eye condition that affects the middle layer of the eye. It’s a type of inflammation that can happen for many reasons, including autoimmune diseases. We’ll look at the different types, symptoms, causes, and treatments for uveitis.
Types and Symptoms
Uveitis can affect different parts of the uvea. The main types are:
- Anterior Uveitis: This affects the front part of the uvea and is often linked to autoimmune diseases.
- Intermediate Uveitis: It affects the middle part of the uvea and is common in young adults.
- Posterior Uveitis: This affects the back part of the uvea and can cause serious vision loss if not treated quickly.
- Panuveitis: It affects all layers of the uvea and is a more severe form of the condition.
The symptoms of uveitis vary by type and severity. They often include:
- Blurred vision
- Eye pain
- Redness
- Sensitivity to light
- Floaters
A leading ophthalmologist says, “Uveitis can greatly affect a patient’s life, making early diagnosis and treatment key.”
“The key to managing uveitis lies in understanding its underlying causes and tailoring treatment according.”
Causes and Associated Conditions
Uveitis can be caused by many things, including:
- Autoimmune disorders, such as rheumatoid arthritis or lupus
- Infections, like toxoplasmosis or tuberculosis
- Injury to the eye
- Certain medications
The table below shows some common causes and related conditions of uveitis:
Cause | Associated Condition | Characteristics |
Autoimmune | Rheumatoid Arthritis | Chronic inflammation, joint pain |
Infectious | Toxoplasmosis | Parasitic infection, vision loss |
Trauma | Eye Injury | Blunt or penetrating trauma |
Treatment and Prognosis
Treatment for uveitis aims to reduce inflammation and improve symptoms. It may include:
- Corticosteroids to reduce inflammation
- Immunosuppressive drugs for autoimmune-related uveitis
- Antibiotics or antivirals for infectious uveitis
- Surgery in severe cases
The outcome for uveitis depends on the cause, severity, and treatment response. Early treatment is key to avoiding long-term vision loss.
We stress the need for a detailed treatment plan for each patient. This ensures the best possible outcome.
Rheumatoid Arthritis and Its Ocular Manifestations
Rheumatoid arthritis (RA) can harm the eyes in many ways. It’s a chronic disease that can affect the cornea, conjunctiva, and sclera. This makes eye health a big concern for those with RA.
Ocular Impact of RA
RA can cause serious eye problems. These include dry eye syndrome, scleritis, and episcleritis. Dry eye syndrome is the most common issue, affecting about 25% of RA patients.
Ocular manifestations of RA can significantly impact a patient’s quality of life. It’s important to understand these issues to manage them well.
Keratoconjunctivitis Sicca and Other Complications
Keratoconjunctivitis sicca is when the eyes don’t make enough tears or have poor quality tears. Other problems include:
- Scleritis: This is inflammation of the sclera that can cause severe pain and vision loss if not treated.
- Episcleritis: It’s inflammation of the episclera, leading to eye redness and irritation.
- Uveitis: This is inflammation of the uvea, which can cause vision problems.
Ocular Condition | Symptoms | Complications |
Keratoconjunctivitis Sicca | Dryness, irritation, blurred vision | Corneal damage, vision loss |
Scleritis | Severe pain, redness, sensitivity to light | Vision loss, scleral thinning |
Episcleritis | Redness, irritation, discomfort | Rarely, vision problems |
Managing Eye Health with RA
It’s key to manage eye health for RA patients. Regular eye exams can catch problems early. Treatment might include:
- Lubricating eye drops for dry eye.
- Anti-inflammatory meds for scleritis and episcleritis.
- Immunosuppressive therapy in severe cases.
Managing RA and its eye problems needs a team effort. Rheumatologists and ophthalmologists must work together.
By knowing about RA’s eye risks and using the right treatments, we can help RA patients live better lives.
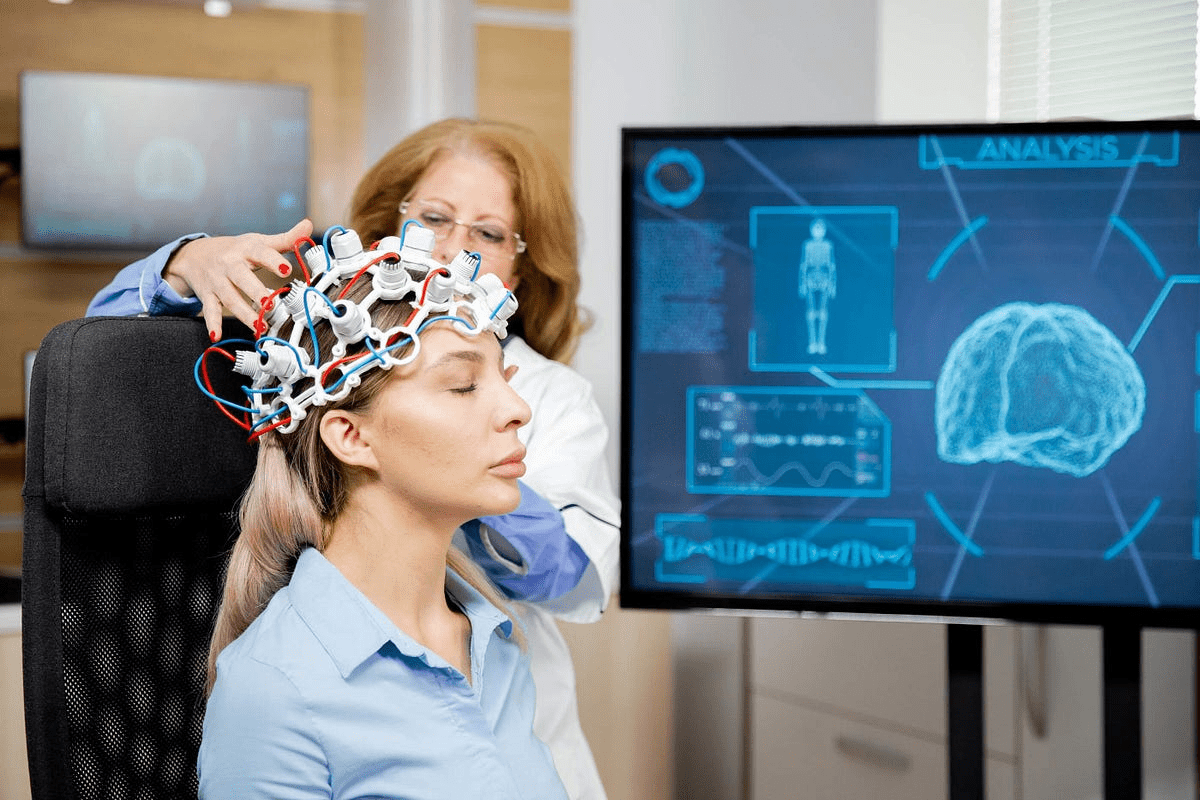
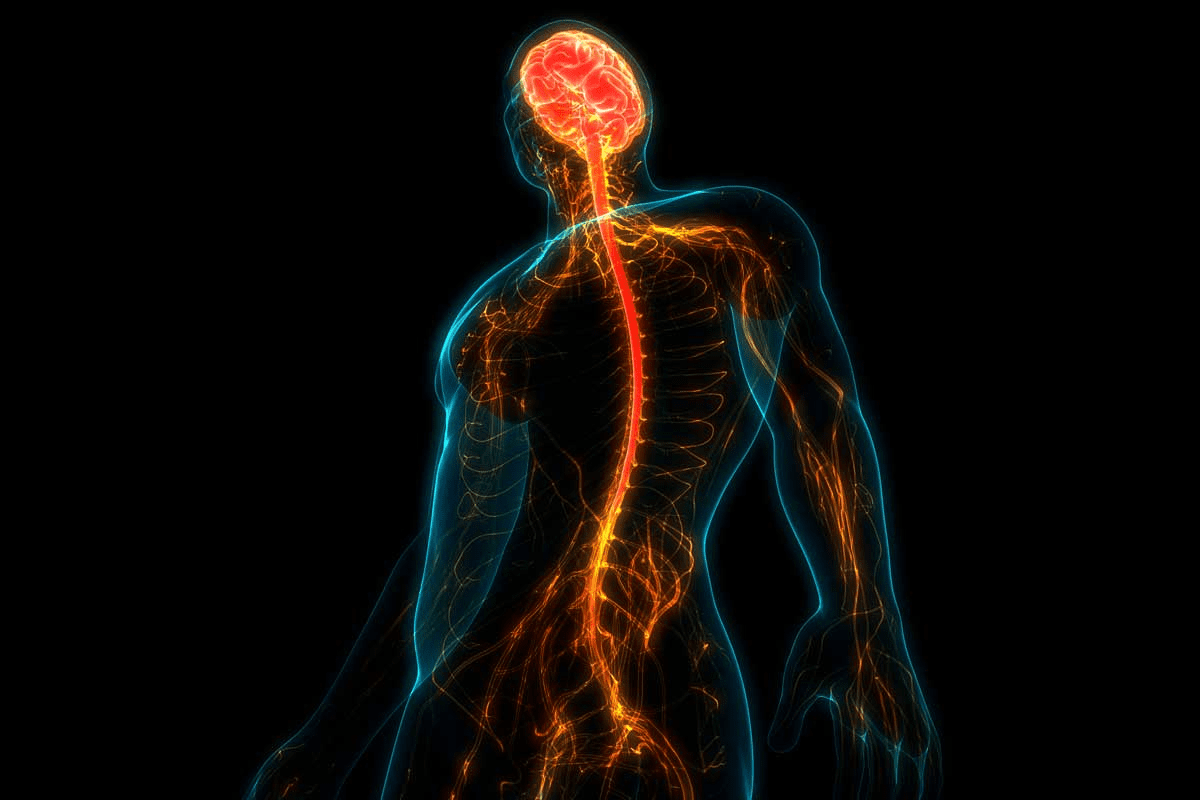
Multiple Sclerosis and Vision Problems
Multiple sclerosis is a chronic autoimmune disease that often affects vision. It can cause many eye-related issues. This condition impacts the central nervous system, leading to various visual disturbances. These problems can significantly affect a person’s quality of life.
Optic Neuritis and MS
Optic neuritis is a common vision problem linked to MS. It’s an inflammation of the optic nerve that can cause pain and temporary vision loss in one eye. About 50% of people with MS will experience optic neuritis at some point.
Optic neuritis is often one of the first signs of MS. It happens when the immune system attacks the myelin sheath around the optic nerve. This disrupts normal nerve function.
Other Visual Disturbances
People with MS may also face other visual issues. These include:
- Double vision or blurred vision
- Difficulty with color vision
- Loss of vision in one eye
- Visual field loss
These problems can arise from lesions in different parts of the visual pathway. This includes the optic nerve and the brain’s visual centers.
Treatment Strategies
Managing vision problems in MS requires a multi-faceted approach. This includes:
Treatment | Description |
Corticosteroids | To reduce inflammation and hasten recovery from optic neuritis |
Disease-Modifying Therapies (DMTs) | To reduce the frequency of MS relapses, potentially decreasing the occurrence of vision problems |
Rehabilitation Therapy | To help patients adapt to persistent visual disturbances |
The National Multiple Sclerosis Society notes, “Early treatment with corticosteroids can help speed up recovery from optic neuritis.”
“The management of MS-related vision problems requires a complete approach. This includes medical treatment, rehabilitation, and lifestyle adjustments.”
Living with MS and its vision problems can be tough. But, with the right treatment and support, many people manage their symptoms well. They can also maintain a good quality of life.
Red Eyes Autoimmune Connection: Scleritis and Episcleritis
Scleritis and episcleritis are linked to autoimmune disorders. They cause red, irritated eyes. These conditions can greatly affect a person’s life, so quick diagnosis and treatment are key.
Distinguishing Features and Symptoms
Scleritis and episcleritis involve inflammation of the sclera, the eye’s white outer layer. Scleritis is more serious, causing pain, vision issues, and possible permanent damage if untreated. Episcleritis is less severe, leading to redness and discomfort but rarely affects vision.
The symptoms can differ but often include:
- Redness of the eye
- Pain or discomfort
- Sensitivity to light
- Vision disturbances (more common in scleritis)
A medical expert notes, “Red eyes, pain, or vision changes need a detailed check for autoimmune conditions.”
Associated Autoimmune Conditions
Scleritis and episcleritis are tied to various autoimmune diseases. Rheumatoid arthritis is a common cause, but they can also be linked to lupus or granulomatosis with polyangiitis.
It’s vital to understand the underlying autoimmune condition to manage these eye issues well. Autoimmune diseases happen when the body attacks its own tissues. In scleritis and episcleritis, this leads to inflammation of the sclera.
Treatment Options
Treatment for scleritis and episcleritis varies based on the condition’s severity and the autoimmune disease. Options include:
- Anti-inflammatory medications to reduce swelling and pain
- Immunosuppressive drugs to manage the autoimmune response
- Biologic agents for targeted therapy in severe cases
Early diagnosis and treatment are critical to avoid complications and manage symptoms well. A complete treatment plan is needed, addressing both the eye condition and the autoimmune disease.
Behçet’s Disease and Ocular Inflammation
Behçet’s disease is a complex autoimmune disorder. It can cause significant inflammation in the eyes. This condition affects many parts of the eye and is known for its wide range of symptoms.
Recognizing Eye Symptoms
The eye symptoms of Behçet’s disease are a big concern. They can lead to chronic inflammation and vision loss. Common symptoms include:
- Uveitis, which is inflammation of the uvea, the middle layer of the eye.
- Retinal vasculitis, indicating inflammation of the blood vessels in the retina.
- Optic neuritis, which is inflammation of the optic nerve.
Medical Expert, a renowned ophthalmologist, says, “Early recognition of these symptoms is key. It helps prevent long-term vision damage.”
Causes and Diagnosis
The exact cause of Behçet’s disease is not known. It’s thought to be a mix of genetics and environment. Doctors diagnose it by looking for specific symptoms like oral and genital ulcers, skin lesions, and eye inflammation.
A study in the Journal of Ophthalmology says, “Diagnosing Behçet’s disease is hard. This is because its symptoms are not specific and can vary a lot.”
Managing Ocular Behçet’s
Managing ocular Behçet’s needs a team effort. Ophthalmologists and rheumatologists work together. Treatment includes:
- Corticosteroids to reduce inflammation.
- Immunosuppressive agents to control the immune system’s abnormal response.
- Biologic agents, such as TNF-alpha inhibitors, for severe cases.
As highlighted by
“The goal of treatment is to reduce inflammation, prevent tissue damage, and preserve vision.”
Regular monitoring and adjusting treatment plans are key to managing the disease well.
We stress the importance of teamwork between healthcare providers and patients. This is essential for managing Behçet’s disease and its eye symptoms effectively.
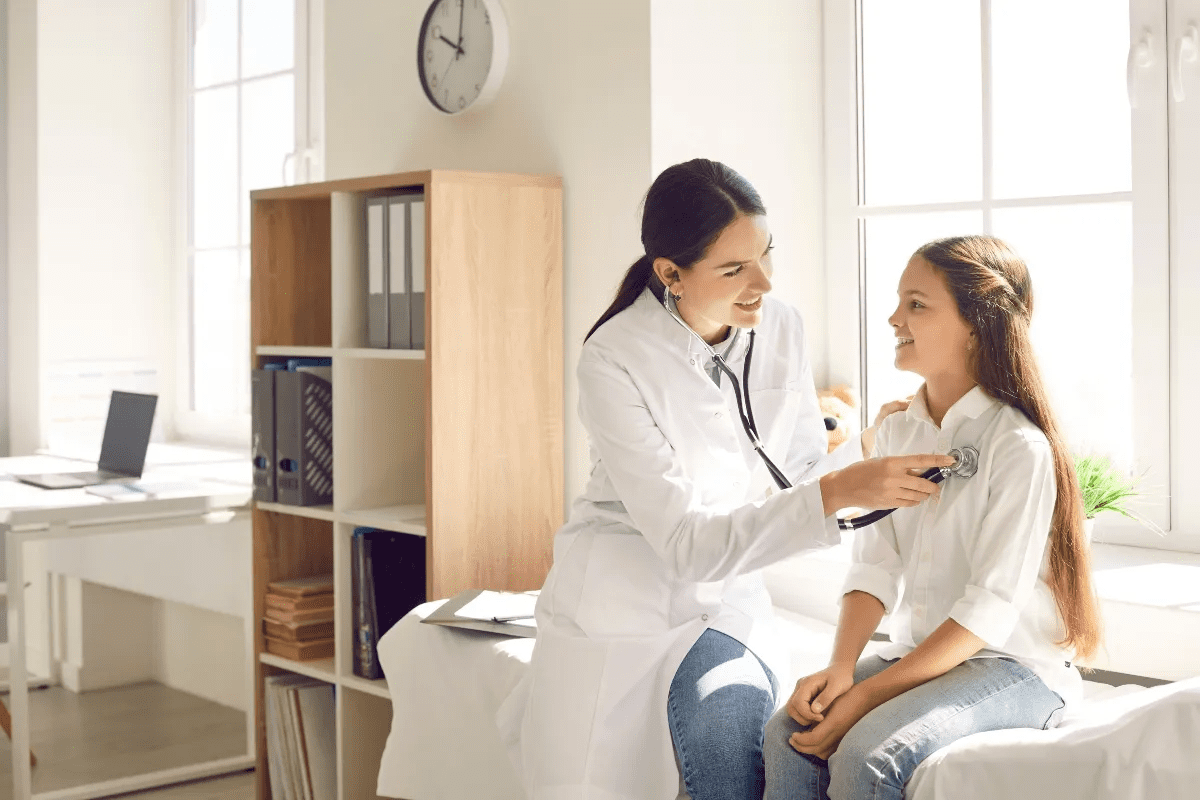
Conclusion: Living with Autoimmune Eye Conditions
Autoimmune diseases of the eyes can really change a person’s life. They need a lot of care and management. We’ve looked at many eye conditions caused by these diseases, like Graves’ disease and Sjögren’s syndrome.
Managing these conditions requires a team effort. It’s important to get a quick diagnosis and effective treatment. People with these diseases need regular check-ups and treatment changes to keep symptoms under control.
Eye care for autoimmune diseases is a team job. Ophthalmologists, rheumatologists, and primary care doctors all play a part. Together, they help keep the eyes healthy and the person well.
Understanding autoimmune eye diseases and the need for full care can make a big difference. It helps improve the lives of those dealing with these conditions.
FAQ
What are autoimmune eye diseases?
Autoimmune eye diseases happen when the immune system attacks healthy eye tissues. This leads to various eye conditions and vision problems.
What are the common symptoms of autoimmune eye diseases?
Symptoms vary by condition but often include dry eye, redness, and inflammation. Vision loss and light sensitivity are also common.
What is Graves’ disease and how does it affect the eyes?
Graves’ disease is an autoimmune disorder affecting the thyroid gland. It can cause thyroid eye disease. Symptoms include bulging eyes, double vision, and light sensitivity.
How does Sjögren’s syndrome affect the eyes?
Sjögren’s syndrome is a chronic autoimmune disorder. It can cause dry eye, leading to dryness, irritation, and vision problems.
What is uveitis and how is it treated?
Uveitis is inflammation of the eye’s middle layer. It can cause vision loss. Treatment includes corticosteroids, immunosuppressive medications, and biologic agents.
How does rheumatoid arthritis affect the eyes?
Rheumatoid arthritis can cause dry eye, scleritis, and uveitis. These can lead to vision problems if not treated.
What is the connection between multiple sclerosis and vision problems?
Multiple sclerosis is a chronic autoimmune disorder. It can cause vision problems like optic neuritis, double vision, and vision loss.
What are scleritis and episcleritis, and how are they treated?
Scleritis and episcleritis are inflammatory conditions causing red eyes. They are often linked to autoimmune disorders. Treatment includes anti-inflammatory medications and immunosuppressive therapy.
What is Behçet’s disease, and how does it affect the eyes?
Behçet’s disease is a rare autoimmune disorder. It can cause significant ocular inflammation. Symptoms include uveitis, retinitis, and vision loss.
How can autoimmune eye diseases be managed?
Management includes prompt diagnosis and effective treatment. Ongoing care helps alleviate symptoms, prevent vision loss, and improve quality of life.
What are the risk factors for developing autoimmune eye conditions?
Risk factors include genetic predisposition and environmental triggers. Underlying autoimmune disorders also increase the risk.
Can autoimmune eye diseases be cured?
While some can be managed well, a cure is not always possible. Treatment focuses on alleviating symptoms, preventing complications, and improving quality of life.
References
No suitable reference found.