Getting a diagnosis of uveitis can be scary. You might wonder if it will get better by itself. Uveitis is a serious eye problem. It causes inflammation within the eye, affecting the uvea, the eye’s middle layer. Wondering ‘can uveitis go away on its own?’ Discover the hard truth about this serious condition and why waiting can be a dangerous mistake.
This layer includes the iris, ciliary body, and choroid. While some cases of acute uveitis might get better without help, it’s important to see a doctor. This is to avoid serious problems and losing your vision.
Key Takeaways
- Uveitis is a serious eye condition that requires medical attention.
- Some acute cases may resolve without treatment, but professional care is recommended.
- Untreated uveitis can lead to permanent vision loss.
- The condition involves inflammation of the uvea, the eye’s middle layer.
- Understanding the types, symptoms, and treatment options is key for managing it well.
Understanding Uveitis: An Overview
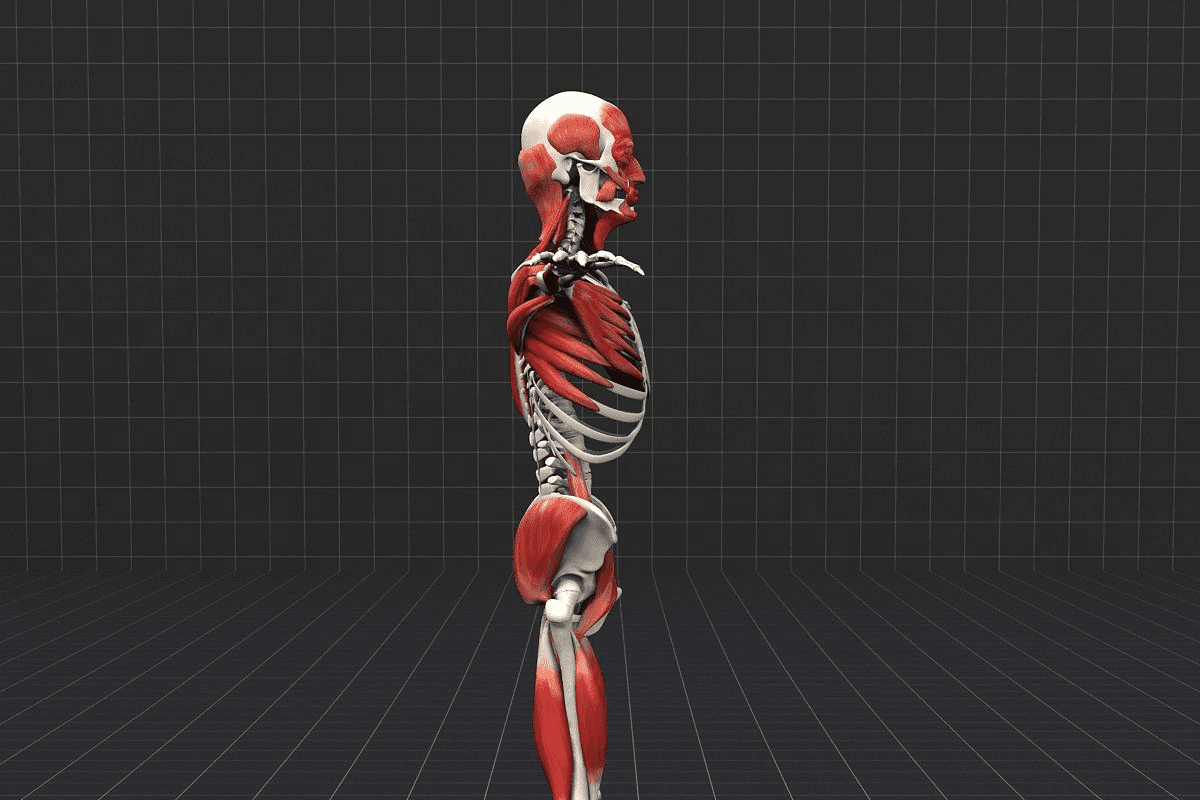
To understand uveitis, knowing about the uvea is key. The uvea is a middle layer in the eye. It’s vital for the eye’s health. Uveitis is when this layer gets inflamed, which can cause serious problems if not treated right.
What Is the Uvea and Its Function in the Eye?
The uvea is the middle layer of the eye. It’s between the sclera (the white outer layer) and the retina (the innermost layer). It has three main parts: the iris, the ciliary body, and the choroid.
The iris controls how much light gets in. The ciliary body makes fluid for the lens and cornea. The choroid supplies the retina with oxygen and nutrients.
Types of Uveitis and Their Characteristics
Uveitis is divided by where in the uvea it happens. The main types are:
- Anterior Uveitis: This is when the front part of the uvea gets inflamed, often the iris.
- Intermediate Uveitis: This affects the vitreous humor, the gel inside the eye.
- Posterior Uveitis: This is when the back part of the uvea, including the choroid, gets inflamed.
- Panuveitis: This is when all parts of the uvea get inflamed.
Each type of uveitis needs a different treatment. Knowing the exact type is important for the right care.
The Prevalence and Impact of Uveitis
Uveitis is not very common but has a big impact on those who get it. It can cause serious problems, like vision loss, if not treated.
Uveitis can happen to anyone, but it’s more common in adults between 20 and 60. Knowing this helps us understand who is at higher risk.
Who Is Most Commonly Affected?
Uveitis can affect anyone, but it’s more common in adults aged 20 to 60. This age group is more likely to get it because of their immune system and what they’re exposed to.
- Adults aged 20-60 are the most common demographic affected by uveitis.
- Children and older adults can also be affected, though less frequently.
Statistics on Vision Loss from Untreated Uveitis
Uveitis has a big impact on vision health. About 30,000 new cases of blindness happen in the U.S. each year because of untreated uveitis. This shows how important it is to treat it quickly to avoid vision loss.
Key statistics include:
- 30,000 new cases of blindness each year in the U.S. due to untreated uveitis.
- Uveitis is responsible for a significant proportion of visual impairment worldwide.
Knowing about uveitis and its effects is key. It helps us understand the need for awareness and quick medical help. By recognizing the risks and acting fast, we can lower the chance of serious problems.
Recognizing the Symptoms of Uveitis
It’s important to know the signs of uveitis to avoid serious problems. Uveitis causes inflammation in the eye. This can lead to different symptoms, some mild, others severe.
Common Warning Signs
The symptoms of uveitis can start quickly or slowly. You might notice eye redness, sensitivity to light (photophobia), blurred vision, and eye pain. Some people see floaters, which are dark spots in their vision.
These signs mean your eye is inflamed. It’s key to know them to get help fast.
When to Seek Medical Attention
If you see signs like an inflamed eye, see an eye doctor right away. Quick action can make a big difference. It helps prevent serious problems.
Waiting too long can make things worse. It could even cause permanent vision loss. So, it’s vital to act fast if you notice these symptoms.
What Causes Uveitis?
Uveitis happens when the immune system mistakenly attacks the eye’s tissues. This can lead to a serious condition that threatens sight. The inflammation occurs in the uvea, the eye’s middle layer. It can be caused by infections, injuries, or other health issues.
Immune System Attacks on Eye Tissues
The immune system is meant to protect us from harm. But in uveitis, it malfunctions and attacks the eye’s tissues. This can cause inflammation and damage. Several things can trigger this autoimmune response, including:
- Infections: Some viral infections can start an immune response that leads to uveitis.
- Eye Injury: Trauma to the eye can cause inflammation and lead to uveitis.
- Surgical Procedures: In some cases, eye surgery can trigger an immune response, resulting in uveitis.
Associated Conditions and Risk Factors
Some health conditions and risk factors can make you more likely to get uveitis. These include:
- Autoimmune Diseases: Conditions like lupus and rheumatoid arthritis can increase the risk of uveitis.
- Viral Infections: Viruses like herpes simplex can cause uveitis.
- Previous Eye Injury or Surgery: People who have had eye trauma or surgery are at higher risk.
Knowing about these conditions and risks is key to catching uveitis early. Healthcare providers can then create effective treatment plans. This helps reduce inflammation and prevent further problems.
Can Uveitis Go Away on Its Own?
Whether uveitis can go away by itself depends on many things. Uveitis is an eye inflammation that can be either acute or chronic.
Acute vs. Chronic Uveitis
Acute uveitis comes on quickly and might get better in a few weeks or months. Chronic uveitis, on the other hand, lasts longer and needs ongoing care to control inflammation and avoid problems.
Key differences between acute and chronic uveitis include:
- Duration: Acute uveitis is shorter, while chronic uveitis can last for years.
- Symptom Onset: Acute uveitis starts suddenly, and chronic uveitis starts more slowly.
- Treatment Approach: Acute cases might not need treatment, but chronic cases need ongoing treatment to prevent vision loss.
Factors Influencing Natural Resolution
Several factors affect whether uveitis can resolve naturally:
- Underlying Cause: The cause of uveitis, like infection or autoimmune disorders, is key.
- Immune Response: How the body reacts to inflammation matters.
- Presence of Underlying Conditions: People with other health issues might have different outcomes.
Even though some acute uveitis might get better by itself, it’s important to see a doctor. Untreated uveitis, whether acute or chronic, can cause serious problems and vision loss.
We suggest that patients stay in close touch with their doctors. This way, they can monitor their condition and get the right treatment. Knowing the type of uveitis and its causes helps patients manage their condition better and avoid complications.
The Dangers of Leaving Uveitis Untreated
Untreated uveitis is a serious threat to eye health. It can cause permanent damage. If not treated, it can lead to severe complications that harm vision and eye health.
Potential Complications
Untreated uveitis can cause several severe problems, including:
- Glaucoma: Increased eye pressure that can harm the optic nerve.
- Cataracts: Clouding of the lens that makes vision blurry.
- Cystoid Macular Edema (CME): Fluid buildup in the macula, causing swelling and vision distortion.
- Retinal Detachment: The retina separates from the eye, leading to severe vision loss.
These issues not only harm vision but also lower the quality of life. It’s vital to see a doctor if you think you have uveitis.
Timeline of Progression Without Treatment
The time it takes for complications to develop can vary. It depends on the uveitis’s severity, any underlying health issues, and how well the immune system responds.
Usually, complications can happen quickly, within weeks or months without treatment. Getting medical help early is key to avoiding these problems and keeping your vision.
Knowing the risks of untreated uveitis shows why early treatment is so important. Treating uveitis quickly can greatly lower the chance of serious complications.
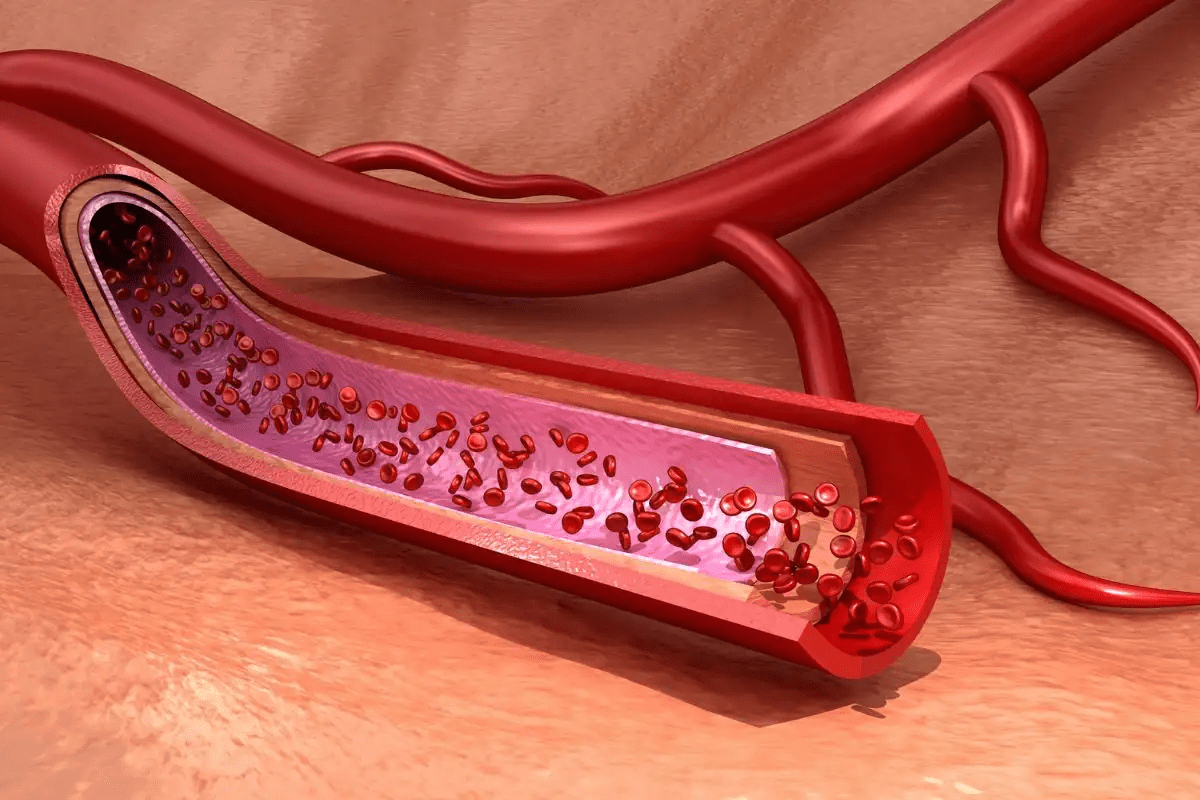
Inflammation Within the Eye: Mechanisms and Effects
It’s important to know how inflammation within the eye works to treat uveitis well. Inflammation is a complex process that can harm the eye’s delicate parts.
How Inflammation Damages Eye Structures
Inflammation in uveitis can harm different parts of the eye, like the uvea, retina, and more. The process involves chemicals that can damage tissues and even cause vision loss.
- Damage to the Uvea: The uvea, made up of the iris, ciliary body, and choroid, has many blood vessels. Inflammation here can mess up its normal function.
- Retinal Involvement: The retina is key for seeing. Inflammation can cause swelling, detachment, or damage to light-sensitive cells.
- Other Structures: Inflammation can also harm the lens, vitreous, and optic nerve. This can lead to problems like cataracts, bleeding in the vitreous, or optic neuritis.
The Inflammatory Cascade in Uveitis
The inflammatory cascade in uveitis is a complex series of interactions. It involves immune cells, cytokines, and other molecules. This cascade can make inflammation worse and cause tissue damage.
Key parts of the inflammatory cascade include:
- Immune cells like T-cells and macrophages get activated.
- Pro-inflammatory cytokines, such as TNF-alpha and IL-1, are released.
- Vascular permeability increases, letting inflammatory cells in.
Knowing these mechanisms is key to creating effective treatments for uveitis. It helps prevent long-term vision loss.
Diagnosing Uveitis: What to Expect
If you think you might have uveitis, getting a thorough check-up is key. This helps figure out how bad it is and what treatment you need. A detailed eye exam is used to see how much inflammation there is and if the eye is damaged.
Common Diagnostic Procedures
To accurately diagnose uveitis, several tests are used. These include:
- Visual Acuity Tests: These check how clear your vision is, which can be affected by uveitis.
- Fundoscopic Exams: These let doctors look at the retina and other parts of the eye for signs of inflammation or damage.
- Slit-Lamp Exams: These exams look at the front part of the eye, like the iris and lens, for signs of uveitis.
These tests help doctors understand how serious the condition is. They then create a treatment plan that’s right for you.
Diagnostic Test | Purpose |
Visual Acuity Test | Measures the sharpness of vision |
Fundoscopic Exam | Examines the retina and internal eye structures |
Slit-Lamp Exam | Inspects the anterior segment of the eye |
Questions Your Doctor May Ask
During your check-up, your doctor will ask you some questions. They want to understand your situation better. They might ask:
- What are your symptoms, and when did they start?
- Do you have a history of eye diseases or surgeries?
- Have you recently experienced any injuries or infections?
Answering these questions clearly helps your doctor make a correct diagnosis. They can then create a treatment plan that works for you.
Getting a correct diagnosis is the first step in managing uveitis well. Knowing about the tests and what to expect makes your eye exam easier.
Treatment Options for Uveitis
Understanding how to treat uveitis is key. The main goal is to lower inflammation, ease pain, and prevent damage. We’ll look at the different ways to manage this condition.
Medication-Based Approaches
Medicine is often the first step in treating uveitis. Corticosteroids are used to fight inflammation. They can be eye drops, injections, or pills, based on the inflammation’s location and severity.
Immunosuppressants or biologic drugs might be needed for chronic or severe cases. These drugs help control the immune system’s attack on the eye. This reduces inflammation and prevents further damage.
Other Therapeutic Interventions
Other treatments are needed for complications or severe uveitis. Surgical procedures might be needed for cataracts, glaucoma, or retinal detachment caused by inflammation.
Vitreoretinal surgery is considered for serious damage to the vitreous or retina. Surgery decisions depend on the condition’s severity and the benefits and risks.
We create a treatment plan tailored to each patient. This ensures the best care for uveitis.
Recurrent Uveitis: Why It Comes Back
Recurrent uveitis can really affect someone’s life, even more so for those with autoimmune diseases. It’s tough to deal with uveitis coming back. Understanding why it happens is key to managing it well.
Underlying Causes of Repeated Episodes
Uveitis often comes back because of inflammation or autoimmune diseases. “The presence of an underlying systemic disease is a significant risk factor for recurrent uveitis,” doctors say. Conditions like rheumatoid arthritis, lupus, or ankylosing spondylitis can make it more likely to happen again.
Genetics, environmental factors, and other eye or body diseases can also play a part. Knowing these can help in making a good plan to manage it.
Managing Chronic and Recurring Cases
Handling chronic and recurring uveitis needs a full plan. We suggest ongoing treatment, regular checks, and changing the plan if needed. “A tailored treatment strategy is essential for controlling inflammation and preventing complications in recurrent uveitis,” guidelines say.
- Regular follow-up appointments with an eye care professional to monitor the condition.
- Adherence to prescribed medication regimens to control inflammation.
- Lifestyle adjustments to minimize risk factors and manage symptoms.
By being proactive and making a plan just for you, you can manage uveitis better. We’re here to support and care for those facing this tough condition.
Living with Uveitis: Lifestyle Considerations
Uveitis can change daily life, but the right steps can help manage it. It’s about medical care, lifestyle changes, and emotional support.
Coping Strategies for Daily Life
Managing uveitis means using several strategies to keep life good. Protecting the eyes from harm is key. Wear sunglasses with UV protection and avoid chemicals that can hurt your eyes.
Managing stress is also important. Stress can make uveitis worse. Try stress-reducing activities like meditation, yoga, or deep breathing.
“The key to managing uveitis is not just treating the condition but also adopting a healthy lifestyle that includes a balanced diet, regular exercise, and sufficient rest.”
Following your treatment plans is critical. This means taking your medicine as told, going to follow-up visits, and knowing about side effects.
Support Resources for Patients
Living with uveitis can be tough, but you’re not alone. There are many support resources to help.
- Patient organizations for uveitis and eye conditions offer support and info.
- Online forums and communities connect you with others facing similar issues.
- Healthcare providers give personalized advice and treatment options.
By using these resources and coping strategies, people with uveitis can live full and active lives.
Conclusion: Taking Control of Your Eye Health
Managing uveitis well means using medicine and changing your lifestyle. Knowing about the condition and following treatment plans helps you take care of your eyes. This way, you can lower the chance of serious problems.
Handling uveitis is complex. We aim to help you with the support and tools you need. This includes top-notch medical care and advice on lifestyle changes for the best vision.
Being proactive in your eye care is key. We’re here to help you at every step. Our goal is to make sure you get the best results in fighting uveitis and keeping your vision safe.
FAQ
Does uveitis go away on its own?
Some cases of acute uveitis might clear up without treatment. But, it’s important to see a doctor to avoid complications and vision loss. Chronic uveitis often needs ongoing care.
What is uveitis and how does it affect the eye?
Uveitis is a serious eye condition. It causes inflammation in the middle layer of the eye. This can lead to vision loss if not treated.
What are the symptoms of uveitis?
Symptoms include eye redness, light sensitivity, blurred vision, and eye pain. These can start suddenly or slowly and vary in severity.
What causes uveitis?
Uveitis happens when the immune system attacks the eye. This can be due to injuries, surgeries, viral infections, or diseases like rheumatoid arthritis.
Can uveitis lead to vision loss?
Yes, if not treated, uveitis can cause serious problems like vision loss. It’s a major cause of blindness each year.
How is uveitis diagnosed?
Doctors use eye exams, including visual tests and slit-lamp exams, to diagnose uveitis. They also ask about your medical history and symptoms.
What are the treatment options for uveitis?
Treatment often includes medications like corticosteroids to reduce inflammation. In some cases, other drugs may be used to control the immune system.
Can recurrent uveitis be managed?
Yes, managing recurrent uveitis involves treating the underlying causes. This includes ongoing medication, regular check-ups, and adjusting treatment as needed.
How can I cope with uveitis in daily life?
To cope, protect your eyes, manage stress, and follow your treatment plan. Support groups and online communities offer help and advice.
What are the possible complications of untreated uveitis?
Untreated uveitis can lead to glaucoma, cataracts, macular edema, and retinal detachment. These can severely affect your vision.
Is uveitis a common condition?
Uveitis is rare but serious. It can affect anyone, but it’s most common in adults aged 20 to 60.
References
National Center for Biotechnology Information. Uveitis: Spontaneous Resolution and Diagnostic Considerations. Retrieved from https://pubmed.ncbi.nlm.nih.gov/24342020/