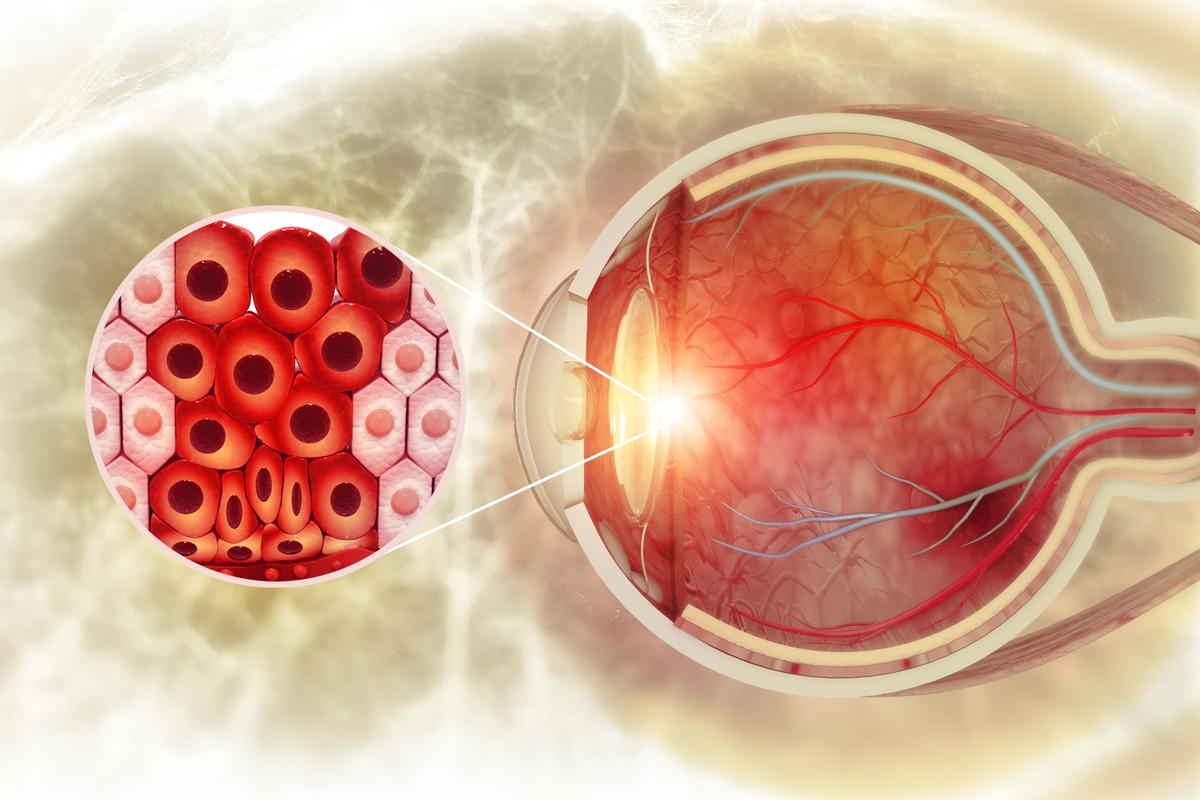
When the body’s defense system goes wrong, it might attack healthy cells in the eyes. This can lead to inflammation and serious vision problems.Explore the link between autoimmune and eyes. Discover how this shocking attack happens and what you can do to protect your vision.
We’re here to explain how autoimmune diseases can harm your eyes. These diseases happen when the immune system mistakenly attacks the eyes’ own tissues. This can cause damage and even permanent vision loss.
At Liv Hospital, we use the latest in care. We mix expert eye doctors with rheumatologists. This way, we offer full support for patients with autoimmune eye diseases.
Key Takeaways
- Autoimmune eye diseases occur when the immune system malfunctions and targets the eyes.
- The immune system’s attack on the eyes can cause inflammation and vision complications.
- Liv Hospital offers multidisciplinary care for patients with autoimmune eye diseases.
- Expert ophthalmology and rheumatology are combined to provide complete support.
- Timely treatment is key to avoid permanent vision loss.
Understanding the Immune System and Ocular Health

Our eyes have a special way of working with our immune system. They need a careful balance to stay healthy and keep our vision clear. The immune system fights off bad germs, but it must do so gently to avoid harming our eyes.
Normal Immune Function in the Eye
The eye has its own defense system to fight off infections. It uses physical barriers like the cornea and sclera to start the defense. It also has a suppressive environment that keeps inflammation in check, preventing damage to the eye.
The eye also uses chemical barriers like tears with enzymes like lysozyme to fight bacteria. It can control the adaptive immune response to avoid too much inflammation that could harm our vision.
Ocular Immune Privilege
The eye has a special protection called ocular immune privilege. This means it can avoid too much of an immune response that could harm it. This privilege is kept up by things like the blood-ocular barrier, which keeps immune cells out.
The eye also has an immune suppressive microenvironment. This includes anti-inflammatory cytokines and regulatory T cells that help keep the immune response in check. This environment is key to protecting the eye from damage during infections and autoimmune reactions.
Understanding ocular immune privilege is key to seeing how autoimmune diseases can affect the eyes. When this balance is broken, the immune system can attack the eye’s tissues. This can lead to autoimmune eye diseases.
When Protection Becomes the Problem: Autoimmune and Eyes
When the immune system goes wrong, the eyes can get hurt. Autoimmune diseases happen when the body’s immune system attacks its own tissues. This can cause inflammation and damage to the delicate parts of the eyes.
Mechanisms of Autoimmunity in Ocular Tissues
The eye is a complex organ with many parts. Each part can be attacked by the immune system. Autoimmune diseases in the eyes can start through molecular mimicry, where the immune system mistakes its own cells for foreign ones.
Key mechanisms include:
- Molecular mimicry between self-antigens and foreign antigens
- Loss of tolerance to self-antigens due to genetic predisposition or environmental triggers
- Activation of autoreactive T cells and B cells
The Role of Inflammation in Eye Damage
Inflammation is a big problem in autoimmune eye diseases. It can cause lasting damage to the eyes, leading to vision loss. Inflammation in the eyes involves many cell types and cytokines.
Inflammatory processes can cause:
- Damage to the cornea, leading to vision distortion
- Uveitis, or inflammation of the uvea, causing pain and vision loss
- Scleritis, or inflammation of the sclera, resulting in severe eye pain
Autoimmune responses in the eyes can lead to serious vision problems. It’s important to understand how autoimmunity and inflammation work. This knowledge is key to finding effective treatments.
Autoimmune Condition | Ocular Manifestation | Potential Complications |
Rheumatoid Arthritis | Scleritis, Keratoconjunctivitis Sicca | Vision loss, Chronic eye pain |
Lupus | Retinal vasculitis, Optic neuritis | Blindness, Visual disturbances |
Sjogren’s Syndrome | Dry Eye Disease | Chronic dryness, Corneal ulcers |
Common Autoimmune Diseases Affecting the Eyes
Many autoimmune conditions can harm the eyes, causing vision problems and discomfort. These diseases happen when the body’s immune system attacks its own tissues. When the eyes are affected, the results can be serious.
Systemic Conditions with Ocular Manifestations
Some autoimmune diseases affect the whole body, including the eyes. Systemic lupus erythematosus (SLE) can cause eye symptoms like dry eyes and retinal vasculitis. Rheumatoid arthritis (RA) is known for joint inflammation but can also cause eye problems like scleritis and episcleritis.
Sjogren’s syndrome mainly affects the tear glands, causing dry eyes. Graves’ disease can lead to thyroid eye disease, causing bulging eyes, double vision, and light sensitivity.
- SLE: Can cause retinal damage and vision loss if not properly managed.
- RA: May lead to scleritis, a painful condition that can result in scleromalacia if left untreated.
- Sjogren’s syndrome: Primarily affects tear production, leading to chronic dry eyes.
- Graves’ disease: Can cause proptosis, or bulging of the eyes, due to inflammation behind the eyeball.
Primary Ocular Autoimmune Disorders
Some autoimmune conditions mainly affect the eyes. Uveitis is an inflammation of the uvea, the middle layer of the eye, which can lead to vision loss if not treated promptly. Optic neuritis involves inflammation of the optic nerve and can cause pain and temporary vision loss in one eye.
These primary ocular autoimmune disorders highlight the importance of early diagnosis and treatment to prevent long-term damage. We will discuss these conditions in more detail, exploring their symptoms, diagnosis, and treatment options.
- Uveitis: Requires immediate treatment to prevent complications like glaucoma and cataracts.
- Optic neuritis: Often associated with multiple sclerosis, it can be a presenting symptom.
Recognizing the Warning Signs
It’s important to spot the early signs of autoimmune eye disorders. This is because these conditions can show up in different ways in the eyes. Knowing these signs can help you get the right care quickly.
Common Symptoms of Autoimmune Eye Disorders
Autoimmune eye disorders can cause a variety of symptoms. These include eye pain, light sensitivity, blurred vision, floaters, redness, and a foreign body sensation. These symptoms can be mild or severe and may come and go.
It’s key to watch for these signs and any changes in your eye health. If you notice any, it’s important to understand what they might mean for your health.
When to Seek Medical Attention
If you see any of these symptoms, it’s important to know when to get help. If your symptoms keep getting worse or don’t go away, you should see an eye doctor.
Getting a diagnosis and treatment early can really help with autoimmune eye disorders. We suggest seeing a doctor if you notice:
- Sudden changes in vision
- Increased sensitivity to light
- Severe eye pain
- New or increasing floaters
- Redness or swelling that doesn’t improve
Looking after your eye health can make a big difference in managing these disorders. If you’re worried about your symptoms, don’t wait to contact a healthcare provider.
Lupus and Vision: How SLE Attacks the Eyes
The link between lupus and vision is complex. Systemic lupus erythematosus (SLE) can harm many parts of the body, including the eyes.
Ocular Manifestations of Lupus
Lupus can lead to various eye issues. These include dry eyes, retinal vasculitis, and optic neuritis. These problems can greatly affect a patient’s quality of life.
Dry Eyes: Dry eye syndrome is common in lupus patients. It happens when the eyes don’t make enough tears. This causes discomfort and vision issues.
Retinal Vasculitis: Inflammation of the retina’s blood vessels can damage it. If not treated, it can lead to vision loss.
Optic Neuritis: This is inflammation of the optic nerve. It can cause pain and temporary vision loss.
Risk Factors for Eye Involvement in SLE
Some factors can make eye problems more likely in SLE patients. Knowing these risk factors is key for early detection and treatment.
Risk Factor | Description |
Disease Duration | Longer disease duration is associated with a higher risk of ocular manifestations. |
Antiphospholipid Antibodies | Presence of these antibodies can increase the risk of retinal vascular events. |
Systemic Disease Activity | Higher systemic disease activity is linked to a greater risk of eye involvement. |
Knowing these risk factors helps doctors watch patients closely. They can act early to stop serious eye problems.
Rheumatoid Arthritis: Beyond Joints to Eyes
Rheumatoid arthritis (RA) is a chronic autoimmune disorder that affects more than just the joints. It also impacts ocular health significantly. The joint symptoms of RA are well-known, but its effects on the eyes are just as important. They often need quick attention to avoid serious problems.
Scleritis and Episcleritis in RA
Scleritis and episcleritis are two inflammatory eye conditions common in RA patients. Scleritis is a serious inflammation of the sclera, the white outer eye wall. It can cause pain, redness, and vision loss if not treated right. Episcleritis affects the thin layer on top of the sclera and is generally less severe but uncomfortable.
Both conditions are linked to RA and show the systemic inflammation of this autoimmune disease. Treating them often requires teamwork between rheumatologists and ophthalmologists. This ensures both joint and eye symptoms are well-managed.
Keratoconjunctivitis Sicca and RA
Keratoconjunctivitis sicca, or dry eye syndrome, is a common eye problem in RA patients. It happens when the lacrimal gland gets inflamed, reducing tear production. This leads to dryness, irritation, and blurred vision.
Treatment includes artificial tears, anti-inflammatory meds, and sometimes punctal plugs to save tears. Managing keratoconjunctivitis sicca well is key to avoiding eye damage. It helps keep the quality of life for those with RA.
Sjogren’s Syndrome and Dry Eye Disease
Sjogren’s syndrome is an autoimmune disease that damages tear glands, causing dry eye. It’s a chronic condition where the immune system attacks the glands that make tears and saliva. This leads to dryness in the eyes and mouth.
Destruction of Tear Glands
The immune system’s response in Sjogren’s syndrome is complex. Autoantibodies attack the lacrimal glands, causing inflammation and damage. This reduces tear production and leads to dry eye symptoms.
It’s important to understand how the immune system works in Sjogren’s syndrome. This knowledge helps in finding effective treatments. It shows how the immune system can both protect and harm when it’s not working right.
Managing Chronic Dry Eyes
Managing dry eyes in Sjogren’s syndrome needs a mix of treatments. We suggest using a combination of treatments to help symptoms and prevent problems.
- Artificial tears to lubricate the eyes
- Anti-inflammatory medications to reduce glandular inflammation
- Punctal plugs to conserve tears
- Restasis or other prescription medications to increase tear production
Treatment Options | Benefits | Considerations |
Artificial Tears | Immediate relief, easy to use | Frequent application needed |
Anti-inflammatory Medications | Reduces inflammation, improves symptoms | Potential side effects, monitor usage |
Punctal Plugs | Conserves tears, long-term relief | Minor surgical procedure |
Understanding Sjogren’s syndrome and its effects on tear glands helps manage dry eye disease. This improves the lives of those affected.
Graves’ Disease and Thyroid Eye Disease
Thyroid eye disease often comes with Graves’ disease. It causes inflammation in the orbit and can lead to vision problems. Graves’ disease is an autoimmune disorder that affects the thyroid gland. It can also impact the eyes significantly.
Orbital Inflammation and Proptosis
Orbital inflammation is a key symptom of thyroid eye disease. It can cause the eyes to bulge out, known as proptosis. This happens when tissues behind the eyeball swell, pushing it forward.
Key factors contributing to orbital inflammation include:
- Autoimmune response
- Inflammation of orbital tissues
- Swelling of extraocular muscles
Proptosis can make the eyes uncomfortable, dry, and irritated. In severe cases, it can cause serious problems like exposure keratopathy or optic neuropathy.
Visual Complications of Thyroid Eye Disease
Thyroid eye disease can cause various vision problems. These include double vision, blurred vision, and vision loss in severe cases. The inflammation and swelling can harm the extraocular muscles and the optic nerve.
Visual Complication | Description |
Diplopia (Double Vision) | Caused by inflammation and swelling of extraocular muscles, leading to impaired eye movement. |
Blurred Vision | Resulting from corneal irregularity or exposure keratopathy due to proptosis. |
Vision Loss | Severe cases can lead to optic neuropathy, potentially causing irreversible vision loss. |
It’s important to understand these complications to manage thyroid eye disease well. Early diagnosis and treatment can reduce the condition’s severity and prevent long-term damage.
Multiple Sclerosis and Neuromyelitis Optica
Optic neuritis is a common problem in multiple sclerosis. It shows how autoimmune diseases can lead to vision loss. Multiple sclerosis (MS) affects the central nervous system, including the optic nerve. We will look at how MS and neuromyelitis optica spectrum disorders (NMOSD) affect the eyes and what it means for patients.
Optic Neuritis in MS
Optic neuritis is inflammation of the optic nerve that can cause pain and vision loss. In MS, it’s a common symptom, often one of the first signs. The severity of optic neuritis can vary, ranging from mild visual disturbances to severe vision loss. Early diagnosis and treatment are key to managing this condition and preventing long-term damage.
The damage in optic neuritis in MS is due to demyelination. This is when the protective myelin sheath around the optic nerve is damaged. This damage disrupts the transmission of visual signals, leading to symptoms. Understanding the mechanisms behind optic neuritis is essential for developing targeted therapies.
Neuromyelitis Optica Spectrum Disorders
Neuromyelitis optica spectrum disorders (NMOSD) are autoimmune conditions that cause severe inflammation of the optic nerve and spinal cord. NMOSD can lead to significant visual impairment and has a poor prognosis if not treated promptly. It’s important to distinguish NMOSD from MS, as their treatments differ.
NMOSD is typically associated with specific autoantibodies, such as aquaporin-4 (AQP4) IgG. Finding these antibodies is key for diagnosing NMOSD and starting the right treatment. We stress that early treatment can greatly improve outcomes for patients with NMOSD.
Uveitis: A Leading Cause of Preventable Blindness
Uveitis is a big problem worldwide, causing many people to lose their sight. It happens when the middle layer of the eye gets inflamed. If not treated quickly, it can cause serious vision problems.
Types and Classification of Uveitis
Uveitis is divided into different types based on where the inflammation is and why it happens. The main types are:
- Anterior Uveitis: This affects the front part of the uvea and is often linked to autoimmune diseases.
- Intermediate Uveitis: It involves the vitreous and the outer part of the retina.
- Posterior Uveitis: This type affects the back part of the uvea and can cause a lot of vision loss.
- Panuveitis: It involves all layers of the uvea.
Associated Systemic Conditions
Uveitis is linked to many systemic conditions, including autoimmune diseases. Some of these include:
- Ankylosing Spondylitis: A form of arthritis that can cause uveitis.
- Rheumatoid Arthritis: An autoimmune disease that can lead to uveitis.
- Sarcoidosis: A condition where granulomas form in the body, including the eyes.
- Inflammatory Bowel Disease: Conditions like Crohn’s disease and ulcerative colitis can be linked to uveitis.
Knowing these connections is key to diagnosing and treating uveitis. Treating the underlying condition is often essential to control eye inflammation.
Diagnosis and Treatment Approaches
Diagnosing autoimmune eye diseases involves both clinical checks and advanced tests. Getting the right diagnosis is key. It lets doctors create a treatment plan that fits each patient’s needs.
Clinical Evaluation and Diagnostic Tests
Doctors start by looking at your medical history and doing a physical check-up. They use special tests to see how your eyes are doing.
Diagnostic Test | Purpose |
Visual Acuity Test | Checks how clear your vision is |
Slit-Lamp Examination | Looks at the front part of your eye |
Fundoscopy | Examines the back of your eye |
Optical Coherence Tomography (OCT) | Shows detailed pictures of your retina |
Immunosuppressive Therapies
Immunosuppressive treatments are key in fighting autoimmune eye diseases. They help lower inflammation and protect your eye tissues.
“Immunosuppressive therapy has revolutionized the treatment of autoimmune eye diseases, giving patients with severe or hard-to-treat disease new hope.”
— Expert Opinion
Biologics and Targeted Treatments
Biologics and targeted treatments are big steps forward in treating autoimmune eye diseases.
- Tumor necrosis factor-alpha (TNF-alpha) inhibitors
- Interleukin inhibitors
- Janus kinase (JAK) inhibitors
Local vs. Systemic Treatment Considerations
Choosing between local and systemic treatments depends on how bad the disease is.
Conclusion: Living with Autoimmune Eye Conditions
Living with autoimmune eye conditions needs a full approach to management and support. We’ve looked at various autoimmune diseases that hit the eyes, like lupus, rheumatoid arthritis, Sjogren’s syndrome, Graves’ disease, and multiple sclerosis.
Autoimmune eye diseases can be tough, but the right care and support can really help. Managing these diseases means using medicine, making lifestyle changes, and keeping a close eye on things.
Good management helps people lessen symptoms, avoid problems, and keep their eyesight. It’s key to work together with doctors and patients to create plans that fit each person’s needs.
Understanding and tackling autoimmune eye conditions head-on can lead to a fulfilling life. We’re dedicated to top-notch healthcare and support for patients worldwide. We aim to help them deal with the ups and downs of living with these conditions.
FAQ
What are autoimmune diseases of the eye?
Autoimmune diseases of the eye happen when the immune system attacks the eyes by mistake. This leads to inflammation and damage. It can cause conditions like uveitis, scleritis, and dry eye disease.
How does the immune system affect the eyes?
The immune system protects the eyes from harm. But in autoimmune diseases, it can overreact. This causes inflammation and damage to the eyes.
What is ocular immune privilege?
Ocular immune privilege is a way the eyes are protected from too much immune response. This includes physical and chemical barriers. It also includes a suppressive environment in the eye.
Can lupus affect the eyes?
Yes, lupus can affect the eyes. It can cause conditions like retinal vasculitis, optic neuritis, and dry eye disease.
How does rheumatoid arthritis affect the eyes?
Rheumatoid arthritis can cause eye problems. It can lead to conditions like scleritis, episcleritis, and dry eye disease.
What is the relationship between Sjogren’s syndrome and dry eye disease?
Sjogren’s syndrome often causes dry eye disease. This is because it destroys the tear glands. It can lead to chronic dry eyes, discomfort, and vision problems.
How does Graves’ disease affect the eyes?
Graves’ disease can cause thyroid eye disease. This involves orbital inflammation, proptosis, and visual complications. These can include double vision and vision loss.
What is the impact of multiple sclerosis on the eyes?
Multiple sclerosis can cause optic neuritis. This is inflammation of the optic nerve. It can lead to vision problems, including blurred vision, pain, and loss of vision.
What is uveitis, and how is it related to autoimmune diseases?
Uveitis is a form of eye inflammation. It can be caused by autoimmune diseases like rheumatoid arthritis, lupus, and multiple sclerosis. It can lead to vision problems and, if left untreated, blindness.
How are autoimmune eye diseases diagnosed and treated?
Autoimmune eye diseases are diagnosed through clinical evaluation, diagnostic tests, and medical history. Treatment includes immunosuppressive therapies, biologics, and targeted treatments. Local and systemic treatment approaches are also used.
What are the common symptoms of autoimmune eye disorders?
Common symptoms include redness, pain, blurred vision, dryness, sensitivity to light, and vision loss. If you experience these symptoms, seek medical attention promptly.
Can autoimmune eye diseases be managed effectively?
Yes, with proper diagnosis and treatment, autoimmune eye diseases can be managed. A good management plan includes medication, lifestyle changes, and regular monitoring. This helps control symptoms and prevent complications.
References
National Center for Biotechnology Information. Autoimmune Eye Conditions: Symptoms and Management. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC8593335/