Our eyes are not just windows to the world; they’re also vulnerable to the body’s immune responses. When the immune system mistakenly attacks the tissues around the eyes, it can lead to a range of conditions that potentially threaten our vision.
Autoimmune diseases that affect the eyes can manifest in various forms, from mild dryness to severe inflammation that could lead to blindness. Understanding these conditions is key for timely diagnosis and effective management.
We will explore seven significant conditions where the body’s immune response impacts the eyes. We’ll discuss their symptoms, causes, and treatment options.
Key Takeaways
- Autoimmune responses can target the eyes, leading to various conditions.
- These conditions range from mild to severe and can impact vision significantly.
- Understanding the symptoms and causes is key for effective management.
- Modern treatment advances offer hope for managing these conditions.
- Specialized centers provide complete care for patients with these conditions.
What Happens When Your Immune System Attacks Your Eyes
When the immune system goes wrong, it might attack the eyes. This can lead to different eye disorders. The eyes are delicate and have many blood vessels, making them a common target.
More than 80 autoimmune diseases can harm the eyes. This shows how closely the immune system and eye health are linked.
The Immune System and Ocular Health
The immune system helps keep us safe from infections. But, if it fails, it might attack the eyes. This can cause inflammation and damage.
The eyes are at risk because of their complex structure and immune cells.
Autoimmune eye diseases can affect different parts of the eye. Knowing how the immune system affects the eyes is key to treating these diseases.
Prevalence and Impact of Eye Autoimmunity
Autoimmune eye diseases can cause vision loss and eye problems worldwide. These conditions can affect anyone, at any age. Some diseases are more common in certain groups.
Autoimmune Disease | Ocular Manifestations | Prevalence |
Rheumatoid Arthritis | Scleritis, Episcleritis | Common |
Sjögren’s Syndrome | Dry Eye Disease | High |
Multiple Sclerosis | Optic Neuritis | Moderate |
Common Warning Signs
It’s important to know the symptoms of autoimmune eye diseases. Look out for redness, pain, blurred vision, and sensitivity to light. If you notice these signs, see an eye doctor right away.
Understanding how the immune system affects the eyes and knowing the symptoms can help. This way, we can protect vision and improve life for those with these conditions.
How Autoimmune Eye Disorders Are Diagnosed
Diagnosing autoimmune eye disorders is a complex task. It requires a detailed approach. These conditions can be hard to spot because their symptoms are varied and can look like other eye diseases.
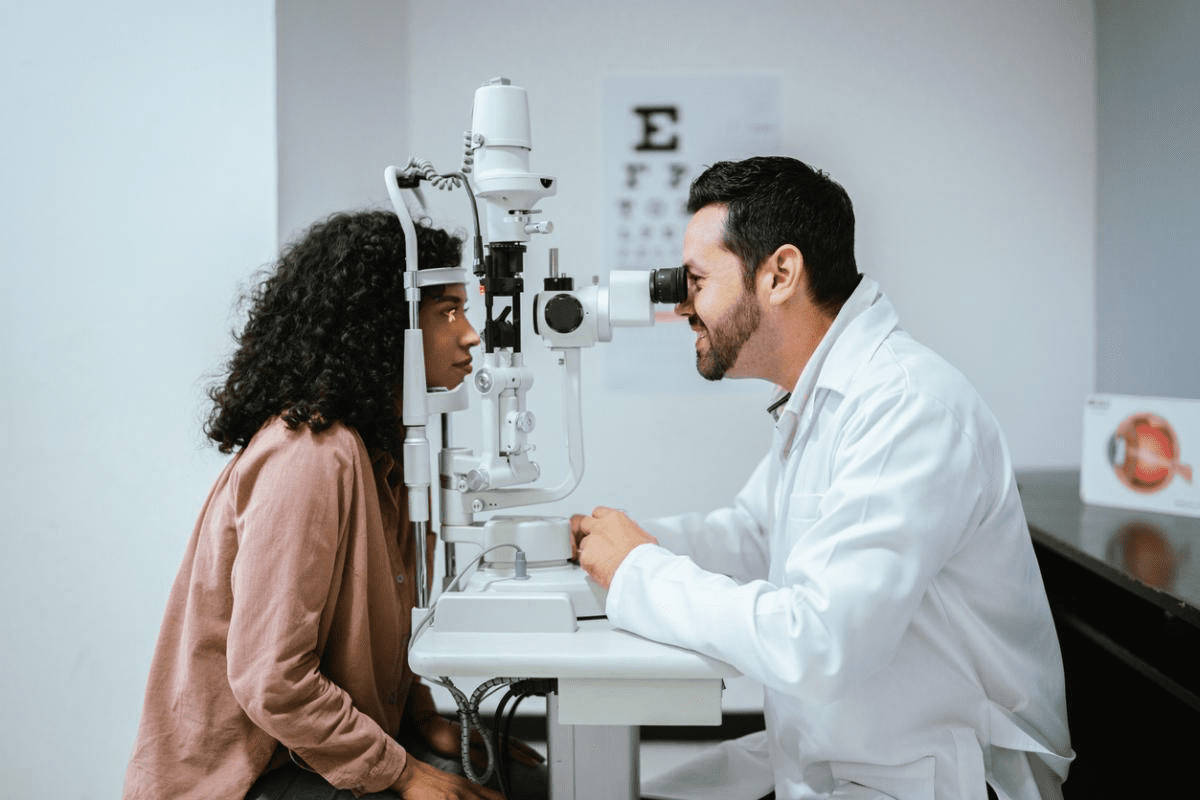
Initial Eye Examination
The first step is a thorough eye check-up. We check how well you can see and look at the eye’s parts. We also check the eye’s health to find any signs of autoimmune issues.
Blood Tests and Biomarkers
After the eye check, we do blood tests. These tests look for biomarkers linked to autoimmune diseases. Finding certain antibodies can show if you have conditions like rheumatoid arthritis or lupus, which can harm the eyes.
Imaging and Specialized Testing
We use advanced imaging and tests to get a better look at the eye disorder. Tools like OCT, fluorescein angiography, and ultrasound imaging help us see the retina and optic nerve clearly. This gives us important details about the eye’s health.
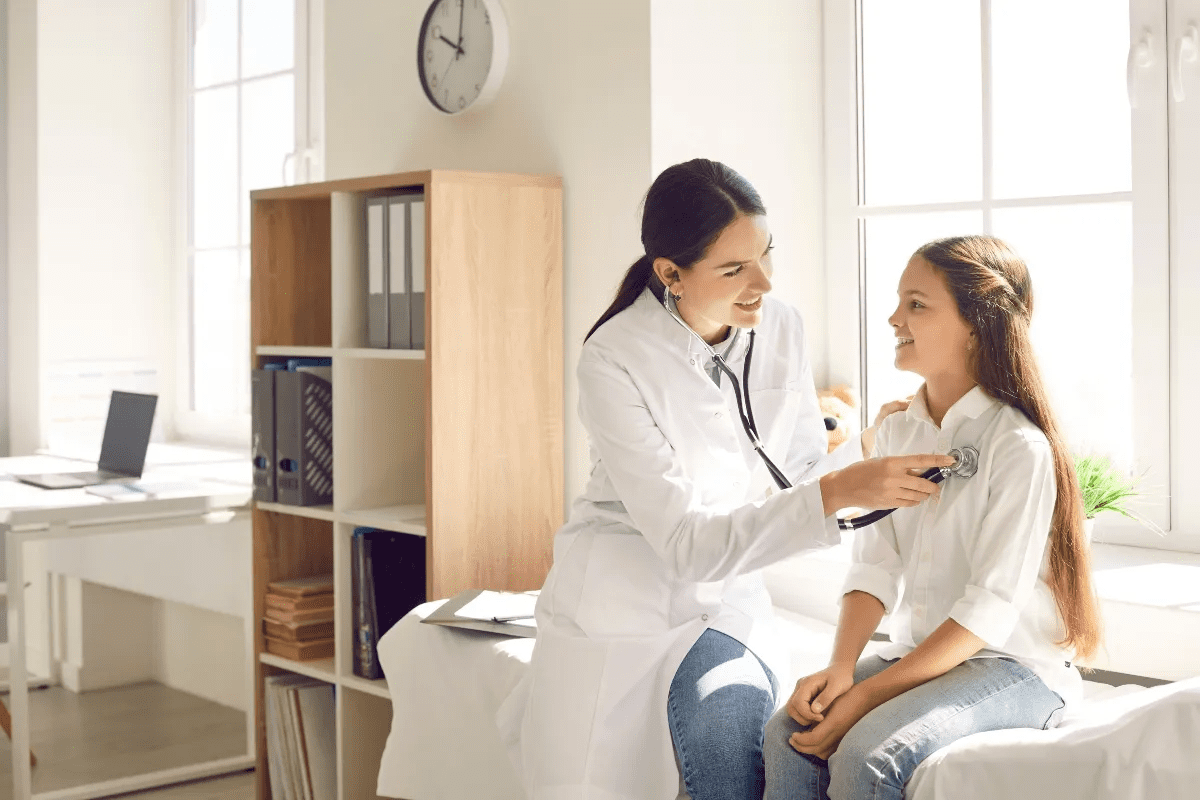
Multidisciplinary Approach
Diagnosing these disorders often needs a team effort. Ophthalmologists, rheumatologists, and other experts work together. Their combined knowledge helps us make a precise diagnosis and plan the best treatment.
Diagnostic Tool | Purpose | Information Gained |
Initial Eye Examination | Assess overall eye health | Visual acuity, external and internal eye structures |
Blood Tests | Identify biomarkers and antibodies | Presence of autoimmune diseases, inflammatory markers |
Imaging Techniques (OCT, Angiography) | Detailed assessment of eye structures | Condition of retina, optic nerve, and other structures |
By using these methods together, we can accurately find autoimmune eye disorders. Then, we can create a treatment plan that works well.
Sjögren’s Syndrome and Dry Eye Disease
We look into how Sjögren’s syndrome and dry eye disease are connected. Dry eye disease affects millions worldwide, making life harder. Sjögren’s syndrome is an autoimmune disease that harms the glands that make tears and saliva, causing dry eyes and mouth.
Understanding Lacrimal Gland Dysfunction
The lacrimal gland is key for eye health, making tears. In Sjögren’s syndrome, the immune system attacks this gland. This leads to inflammation and less tear production, causing dry eye disease symptoms.
Dry eye disease makes eyes feel dry, irritated, and uncomfortable. People might feel like there’s something in their eyes, be more sensitive to light, and see blurry. These issues can make daily life tough.
Key Symptoms and Warning Signs
Knowing the signs of dry eye disease linked to Sjögren’s syndrome is important. Look out for:
- Dryness and irritation
- Redness and inflammation
- Sensitivity to light
- Blurred vision
- Discomfort wearing contact lenses
If you notice these, see an eye doctor. They can spot Sjögren’s syndrome early.
Treatment Options
Dealing with dry eye disease from Sjögren’s syndrome needs a few steps. Treatments include:
- Artificial tears and eye drops to help with tear loss
- Anti-inflammatory meds to lessen gland inflammation
- Punctal plugs to keep tears in the eyes
- Prescription meds like Restasis to boost tear production
Understanding Sjögren’s syndrome and dry eye disease helps manage symptoms. This improves life for those with this chronic condition.
Rheumatoid Arthritis and Scleritis
Rheumatoid arthritis (RA) is a chronic autoimmune disorder that can affect many parts of the body, including the eyes. This leads to conditions like scleritis. It shows how autoimmune diseases can impact eye health.
Inflammation Effects on Eye Tissues
Rheumatoid arthritis can cause inflammation in the body, including the eyes. When RA hits the eyes, it can cause scleritis. This condition brings severe eye pain and vision problems.
“Scleritis is a serious condition that needs quick medical attention to avoid vision loss,” says Medical Expert, an ophthalmologist. Managing scleritis often means treating RA and the eye inflammation directly.
Recognizing Scleritis and Episcleritis
Scleritis and episcleritis are both eye inflammation conditions. But they differ in severity and the eye layers they affect. Scleritis affects the sclera, the white outer layer of the eyeball, and is very painful. Episcleritis affects the episclera, a thin layer on top of the sclera, and is less severe.
- Scleritis Symptoms: Severe eye pain, redness, sensitivity to light, and possible vision problems.
- Episcleritis Symptoms: Eye redness, mild discomfort, and sometimes watery discharge.
Treatment Approaches
Treating scleritis and episcleritis requires a multi-faceted approach. For scleritis, treatment includes oral NSAIDs or corticosteroids to reduce inflammation. In severe cases, immunosuppressive medications may be needed. Episcleritis, being less severe, might be managed with topical lubricants or mild anti-inflammatory eye drops.
Key Treatment Strategies:
- Anti-inflammatory medications to reduce swelling and pain.
- Immunosuppressive therapy for severe or refractory cases.
- Supportive care, such as lubricating eye drops, to manage symptoms.
Understanding the link between rheumatoid arthritis and eye conditions like scleritis is key for effective management. By treating both systemic inflammation and ocular symptoms, healthcare providers can help patients achieve better outcomes and improved quality of life.
Graves’ Disease and Thyroid Eye Disease
Graves’ disease and thyroid eye disease are linked by an autoimmune response. This response affects the thyroid gland and the eye tissues. Graves’ disease mainly targets the thyroid gland but can also cause thyroid eye disease (TED). TED inflames and swells the eye tissues.
The Thyroid-Eye Connection
The thyroid gland and eyes are connected through immune responses and cellular interactions. In Graves’ disease, the immune system attacks the thyroid gland, causing hyperthyroidism. This attack can also target the eye tissues, leading to TED. The exact mechanisms are not fully understood, but it’s believed that both the thyroid gland and orbital tissues share common antigens.
Recognizing TED Symptoms
Thyroid eye disease can show in different ways, making it important to spot its symptoms early. Common signs include:
- Protrusion of the eyeballs (exophthalmos)
- Swelling and redness of the eyelids and conjunctiva
- Double vision (diplopia)
- Dryness and irritation of the eyes
- In severe cases, vision loss
Early diagnosis is critical to prevent damage and start treatment. TED can affect one or both eyes and doesn’t always match the severity of Graves’ disease.
Modern Treatment Options
Treating thyroid eye disease requires a team effort from endocrinologists, ophthalmologists, and sometimes orbital surgeons. The goal is to manage the thyroid, reduce orbital inflammation, and alleviate symptoms.
Modern treatments include:
- Medications: Corticosteroids to reduce inflammation, and immunosuppressive drugs to control the autoimmune response.
- Orbital Radiotherapy: To reduce inflammation and swelling in the orbital tissues.
- Surgical Options: Orbital decompression surgery to relieve pressure on the eyeball, and eyelid surgery to correct eyelid retraction or other abnormalities.
We are dedicated to providing full care for patients with thyroid eye disease. We use the latest treatments to improve outcomes and quality of life.
Multiple Sclerosis and Optic Neuritis
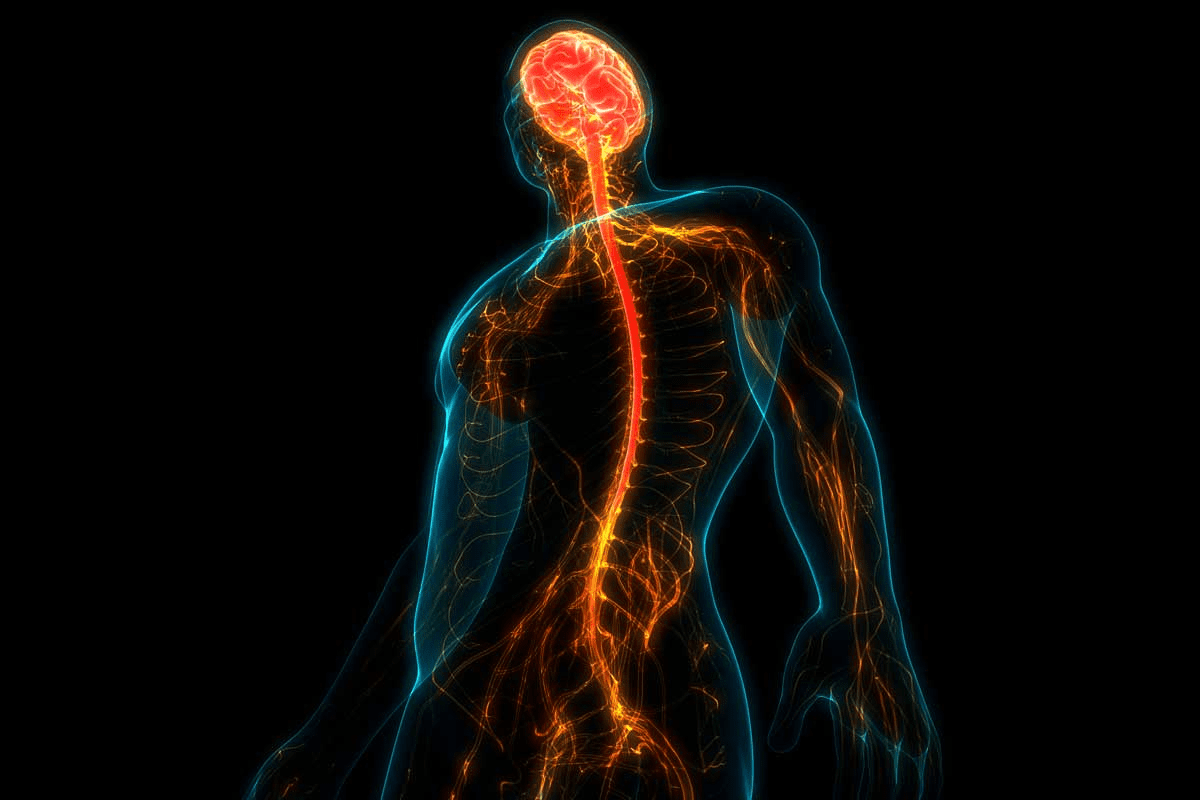
Multiple sclerosis (MS) is a complex autoimmune disease. It can greatly affect the visual system, often through optic neuritis. This inflammation of the optic nerve can cause vision problems. It’s important to understand and manage this aspect of MS.
Impact on the Optic Nerve
MS can harm the optic nerve in many ways, causing optic neuritis. The optic nerve is key for sending visual information to the brain. When it gets inflamed, it can cause pain and temporary vision loss, usually in one eye.
The exact reasons for MS causing optic neuritis are not fully known. But, it’s thought that the immune system’s attack on the optic nerve’s myelin sheath is a big part. This demyelination disrupts the flow of electrical impulses, causing the symptoms of optic neuritis.
Recognizing the Symptoms
To spot optic neuritis, look for its main symptoms:
- Pain when moving the affected eye
- Temporary vision loss or blurring
- Impaired color vision
- Visual field loss
These symptoms can vary in how bad they are and how fast they come on. It’s key for people with these symptoms to see a doctor right away. This can help prevent lasting vision damage.
Effective Treatment Protocols
Treating optic neuritis usually means fighting the inflammation and managing symptoms. Common treatments include:
- Corticosteroids: To reduce inflammation and speed up recovery.
- Plasma exchange: In severe cases, to remove antibodies from the blood.
- Vision therapy: To improve visual function.
We also work on managing the underlying MS to stop more episodes of optic neuritis and other symptoms. This all-around approach helps patients with MS and optic neuritis get the best care possible.
Understanding Autoimmune Eye Disorders: Uveitis
The uvea, a key part of the eye, is hit by uveitis, an inflammatory issue tied to autoimmune diseases. This condition inflames the uvea, which includes the iris, ciliary body, and choroid. It can cause serious vision issues and is a major reason for sight-threatening problems.
Types and Classification
Uveitis is divided based on the uvea part it affects, its length, and if it’s linked to a systemic disease. The main types are:
- Anterior Uveitis: Hits the front of the uvea, often tied to ankylosing spondylitis.
- Intermediate Uveitis: Affects the middle of the uvea, sometimes linked to multiple sclerosis.
- Posterior Uveitis: Hits the back of the uvea, possibly tied to infections or autoimmune diseases.
- Panuveitis: Involves all layers of the uvea.
Symptoms and Warning Signs
Symptoms of uveitis vary by type and severity but often include:
- Eye pain and redness
- Blurred vision
- Sensitivity to light
- Floaters
Seeing a doctor is key if these symptoms show up. Untreated uveitis can cause cataracts, glaucoma, and permanent vision loss.
“Early diagnosis and treatment of uveitis are critical to preventing long-term vision damage and improving patient outcomes.”
Treatment Approaches
Treatment for uveitis aims to cut inflammation and manage symptoms. Methods include:
- Corticosteroids: To reduce inflammation.
- Immunosuppressive drugs: For cases tied to autoimmune diseases.
- Biologic agents: Targeted therapy for specific cases.
We tailor treatment plans to each patient’s needs and underlying conditions.
Lupus and Ocular Complications
Systemic lupus erythematosus (SLE) is a complex autoimmune disease. It can affect many parts of the body, including the eyes. SLE can be hard to diagnose and treat, making eye problems a big challenge.
Ocular Manifestations of SLE
SLE can cause a variety of eye issues. These range from mild dry eye to severe problems like retinal vasculitis and optic neuritis. Retinal vasculitis is a serious issue that can cause vision loss if not treated quickly. It happens when the blood vessels in the retina get inflamed, affecting vision.
Eye problems in SLE patients can differ a lot. Some common issues include:
- Dry eye syndrome
- Retinal vasculitis
- Optic neuritis
- Scleritis
- Uveitis
Diagnosis Challenges
Diagnosing eye problems in SLE patients can be tough. This is because many symptoms are not specific. A detailed eye exam is key for accurate diagnosis. This includes tests like visual acuity, slit-lamp examination, and imaging studies like OCT.
When looking at eye symptoms, we must also consider the patient’s medical history and SLE activity. Blood tests for inflammatory markers and autoimmune antibodies can help a lot.
Treatment Strategies
Managing eye problems in SLE needs a team effort from rheumatologists and ophthalmologists. The treatment plan is made for each patient’s specific eye condition and how severe it is.
For mild issues like dry eye, eye drops and lifestyle changes might be enough. But for serious problems like retinal vasculitis or scleritis, stronger treatments like immunosuppressants or biologic agents might be needed. These help control inflammation and prevent vision loss.
The treatment should be tailored to the patient’s health, SLE activity, and eye condition. This ensures the best care for each patient.
Conclusion: Living With Autoimmune Eye Conditions
We’ve looked at different autoimmune eye disorders, their symptoms, causes, and treatments. To manage these conditions, it’s key to understand them well. A supportive care plan is essential to handle their complexities.
Early detection and the right treatment are vital. Knowing the warning signs and getting medical help quickly can help a lot. This way, people can keep their vision and quality of life better.
Handling autoimmune eye disorders needs a team effort. Ophthalmologists, rheumatologists, and others work together. They create treatment plans that fit each person’s needs, helping them stay healthy and well.
Being proactive and working together with healthcare teams helps a lot. People with autoimmune eye conditions can face their challenges better. This approach can lead to better long-term results.
FAQ
What are autoimmune eye disorders?
Autoimmune eye disorders happen when the body’s immune system attacks the eyes. This can cause serious vision problems.
What are the common symptoms of autoimmune eye diseases?
Symptoms include dry eyes, eye pain, redness, and vision issues. You might also feel sensitive to light.
How are autoimmune eye disorders diagnosed?
Doctors use several steps to diagnose these disorders. First, they do an eye exam. Then, they take blood tests and use imaging to see how bad it is.
What is Sjögren’s syndrome and how does it affect the eyes?
Sjögren’s syndrome is a chronic condition that mainly affects the glands that make tears and saliva. It leads to dry eyes and mouth.
Can rheumatoid arthritis affect the eyes?
Yes, rheumatoid arthritis can cause eye problems. It can lead to severe pain and vision issues.
What is thyroid eye disease and how is it related to Graves’ disease?
Thyroid eye disease is linked to Graves’ disease. It causes inflammation and swelling around the eyes.
How does multiple sclerosis impact the eyes?
Multiple sclerosis can damage the optic nerve. This can cause vision loss, pain, and other vision problems.
What is uveitis and how is it related to autoimmune diseases?
Uveitis is eye inflammation that can be linked to autoimmune diseases. It can cause serious vision problems.
Can systemic lupus erythematosus affect the eyes?
Yes, systemic lupus erythematosus can harm the eyes. It can lead to various eye problems.
What are the treatment options for autoimmune eye disorders?
Treatment depends on the condition. It may include medications to reduce inflammation and manage symptoms. Lifestyle changes are also important.
Why is early detection and treatment important for autoimmune eye disorders?
Early treatment is key to managing these disorders. It helps prevent severe vision loss and improves life quality.
What is the role of the immune system in autoimmune eye disorders?
In these disorders, the immune system mistakenly attacks the eyes. This leads to inflammation and damage.
Are there any specific autoimmune diseases that commonly affect the eyes?
Yes, several diseases can affect the eyes. These include Sjögren’s syndrome, rheumatoid arthritis, Graves’ disease, multiple sclerosis, and systemic lupus erythematosus.
References
National Center for Biotechnology Information. Autoimmune Eye Disorders: Symptoms, Causes, and Treatment. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8593335/