Uveitis is an inflammatory condition that affects the uvea. This is the layer between the sclera and retina. It’s often linked to autoimmune disorders. In these cases, the immune system attacks healthy eye tissue by mistake.
Uveitis is a big cause of blindness in young people in the Western world. Knowing if it’s an autoimmune disease is key for early treatment. At Liv Hospital, we focus on our patients to tackle this complex issue.
Key Takeaways
- Uveitis is associated with autoimmune disorders.
- Autoimmune uveitis requires thorough treatment.
- Liv Hospital offers patient-focused care for uveitis patients.
- Early detection is vital to save vision.
- Uveitis can cause blindness if not treated.
What is Uveitis? Understanding the Basics
Uveitis is an inflammatory condition that affects the uvea, the middle layer of the eye. It causes inflammation in the uvea, leading to vision problems if not treated quickly.
Definition and Anatomy of the Uvea
The uvea is a key part of the eye, made up of the iris, ciliary body, and choroid. It supplies blood and nutrients to the eye and is essential for its health. Inflammation of the uvea, or uveitis, can result from various causes, including autoimmune disorders.
Uveitis is a major cause of vision loss worldwide, affecting about 38 to 714 per 100,000 people globally. It can appear in different forms, depending on where in the uvea the inflammation is.
Types of Uveitis Based on Location
Uveitis can be divided into types based on where the inflammation is in the eye. These include:
- Anterior Uveitis: Inflammation of the front part of the uvea, often linked to conditions like iritis.
- Intermediate Uveitis: Inflammation of the middle part of the uvea, affecting the ciliary body.
- Posterior Uveitis: Inflammation of the back part of the uvea, involving the choroid.
- Panuveitis: Inflammation that affects all parts of the uvea.
Each type of uveitis has its own characteristics and may be caused by different things, including autoimmune disorders. Knowing the specific type of uveitis is key to finding the right treatment.
The Prevalence and Impact of Uveitis
It’s important to know how common uveitis is and its effects on health. This eye condition affects thousands yearly, leading to discomfort and vision issues. It’s a big health concern that needs our focus.
Global Statistics and Demographics
Uveitis is a worldwide health issue. Its occurrence varies among different groups. Research shows it affects 17 to 52 people per 100,000 each year. Anyone can get it, but some groups face higher risks.
Age Distribution and Risk Factors
Uveitis affects people of all ages, but differently. Young adults often get anterior uveitis, while older adults are more likely to have posterior uveitis. Knowing the risk factors helps in early treatment.
Uveitis as a Cause of Blindness
Autoimmune uveitis is the main cause of uveitis and leads to 10-15 percent of blindness in Western countries. Its ability to cause blindness highlights the need for quick diagnosis and treatment. Understanding its causes helps us reduce its impact on vision and life quality.
Uveitis and Autoimmune Disorders: The Connection
Autoimmune mechanisms are key in uveitis, a condition where the uvea gets inflamed. This condition is linked to many autoimmune disorders. It shows how immune system problems can lead to eye inflammation.
The Autoimmune Nature of Uveitis
Recent studies show that autoimmune responses cause uveitis. Abnormal T cell responses are a big part of it. These T cells attack the uveal tissue, causing inflammation and damage.
Autoimmune conditions like multiple sclerosis and ankylosing spondylitis often have uveitis. This shows how important it is to look at autoimmune causes when diagnosing and treating uveitis.
Percentage of Uveitis Cases Attributed to Autoimmune Mechanisms
About 30-50% of uveitis cases are due to autoimmune issues. This number can change based on who is studied and how they are diagnosed.
“The recognition of autoimmune uveitis as a distinct clinical entity has significant implications for patient management, highlighting the need for targeted therapeutic strategies to address the underlying immune dysregulation.”
— Expert Opinion
Distinguishing Autoimmune from Other Causes
It’s important to tell autoimmune uveitis apart from other causes. Autoimmune uveitis often has specific signs, like both eyes being affected and being linked to other autoimmune diseases. Tests, like blood tests for autoimmune diseases, help figure out if it’s autoimmune uveitis.
- Presence of systemic autoimmune disease
- Bilateral uveitis
- Specific serological markers
Knowing how uveitis and autoimmune disorders are connected helps doctors treat patients better. This can lead to better results for those with this complex condition.
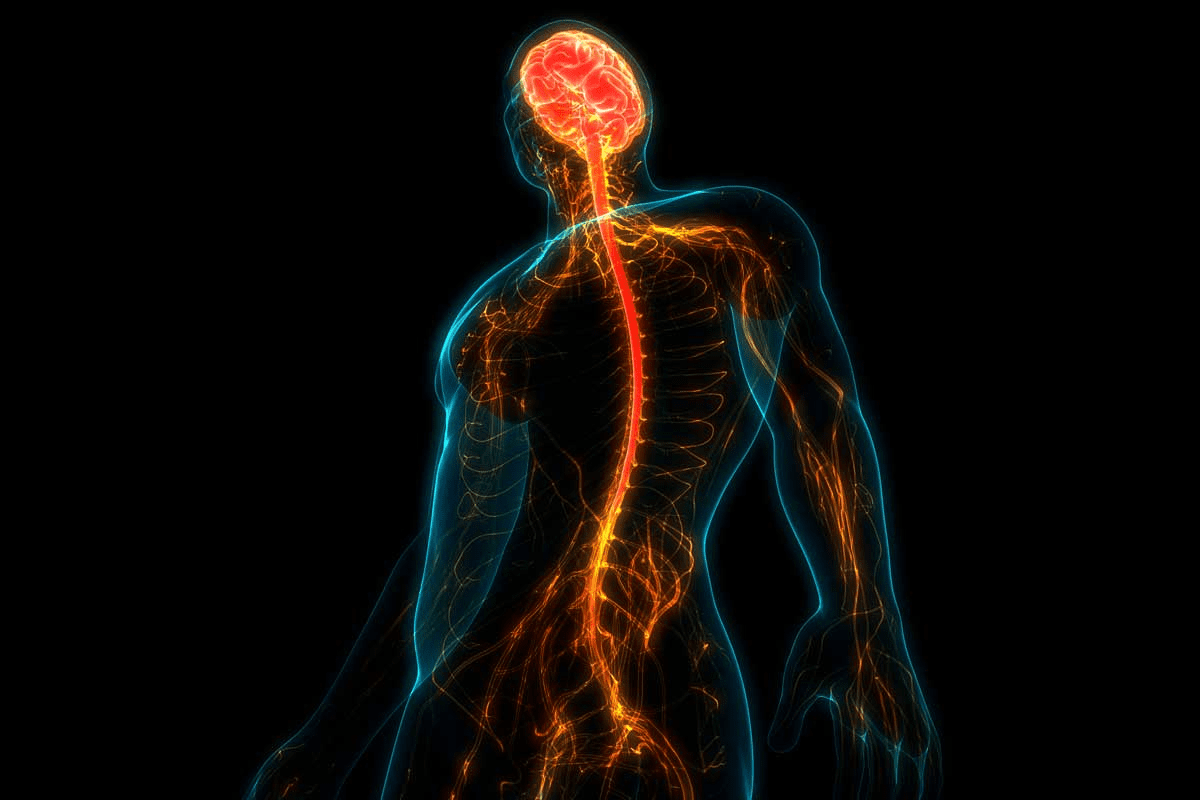
The Immunological Mechanisms Behind Autoimmune Uveitis
Understanding how the immune system works in autoimmune uveitis is key to finding treatments. This condition happens when the immune system attacks the uvea, causing inflammation and serious vision problems.
Abnormal T Cell Responses
T cells are important in the immune system. In autoimmune uveitis, they mistakenly see the eye’s tissues as enemies. This leads to an immune attack on the eye.
“The misdirected immune response in autoimmune uveitis highlights the complex interplay between genetic predisposition and environmental triggers.”
The Role of Th17 T Cell Sub-populations
Th17 cells are a part of T helper cells involved in autoimmune uveitis. They make IL-17, a cytokine that causes inflammation and damage.
Self-antigen Recognition in Ocular Tissue
In autoimmune uveitis, the immune system sees self-antigens in the eye as foreign. This mistake triggers an immune response. Recognizing self-antigens is a key step in the disease’s development.
Breakdown of Ocular Immune Privilege
The eye is usually protected from the immune system’s attacks. This protection prevents damage to the eye’s delicate tissues. In autoimmune uveitis, this protection fails, causing inflammation and damage.
As we learn more about autoimmune uveitis, it’s clear that understanding its immune mechanisms is vital. This knowledge is essential for creating effective treatments for this complex condition.
Common Systemic Autoimmune Diseases Associated with Uveitis
Uveitis, an eye inflammation, is linked to several autoimmune diseases. These diseases can cause inflammation in the uvea. Knowing these connections helps in diagnosing and treating uveitis.
Ankylosing Spondylitis and Related Spondyloarthropathies
Ankylosing spondylitis is often linked with uveitis. People with this condition may have recurring uveitis. The presence of HLA-B27 increases the risk of both conditions.
Key Features:
- Acute anterior uveitis
- HLA-B27 positivity
- Recurrent episodes
Inflammatory Bowel Diseases (Crohn’s and Ulcerative Colitis)
Crohn’s disease and ulcerative colitis can lead to uveitis. Uveitis in these patients often appears as anterior uveitis. It’s important to manage IBD to control uveitis.
Notably, IBD can affect the eye in many ways. This makes eye care essential for these patients.
Behcet’s Disease
Behcet’s Disease is a condition that affects many parts of the body and is linked to uveitis. It can cause severe uveitis, which may lead to vision loss if not treated aggressively.
Key Ocular Features:
- Posterior uveitis
- Retinal vasculitis
- Severe vision loss if untreated
Autoimmune Thyroiditis
Autoimmune thyroiditis, or Hashimoto’s thyroiditis, is connected to uveitis. Though less common, it shows how different autoimmune diseases can affect each other.
Managing autoimmune thyroiditis requires a holistic approach. This includes considering the risk of eye problems.
Understanding the links between systemic autoimmune diseases and uveitis helps healthcare providers. They can then offer better care, reducing the risk of vision loss and improving patient outcomes.
Recognizing Autoimmune Eye Inflammation: Symptoms of Uveitis
It’s important for patients to know the signs of autoimmune uveitis. This condition can cause different symptoms that affect vision. Knowing these symptoms helps in getting early treatment.
Common Ocular Symptoms
Uveitis can show itself in many ways, including:
- Pain and Redness: The eye may hurt and look red because of inflammation.
- Vision Disturbances: You might see things blurry, have floaters, or be sensitive to light.
- Decreased Vision: In serious cases, you could see less clearly.
Systemic Symptoms That May Accompany Uveitis
Uveitis can also be linked to diseases that affect the whole body. These diseases can cause symptoms like:
- Joint Pain and Swelling: Conditions like ankylosing spondylitis can make your joints hurt and swell.
- Skin Rashes: Some autoimmune diseases can cause rashes on the skin.
- Gastrointestinal Issues: Diseases like Crohn’s can lead to stomach problems.
When to Seek Medical Attention
If you think you might have uveitis, get help right away. Waiting too long can cause serious problems, like permanent vision loss. If you notice any of these, see an eye doctor:
- Sudden eye pain or redness
- Blurred vision or vision loss
- Being more sensitive to light
Symptom | Description | Action |
Eye Pain | Pain or discomfort in the eye | Seek immediate medical attention |
Blurred Vision | Loss of sharpness or clarity in vision | Consult an eye care professional |
Floaters | Spots or specks floating in the visual field | Monitor and report to your doctor if persistent or severe |
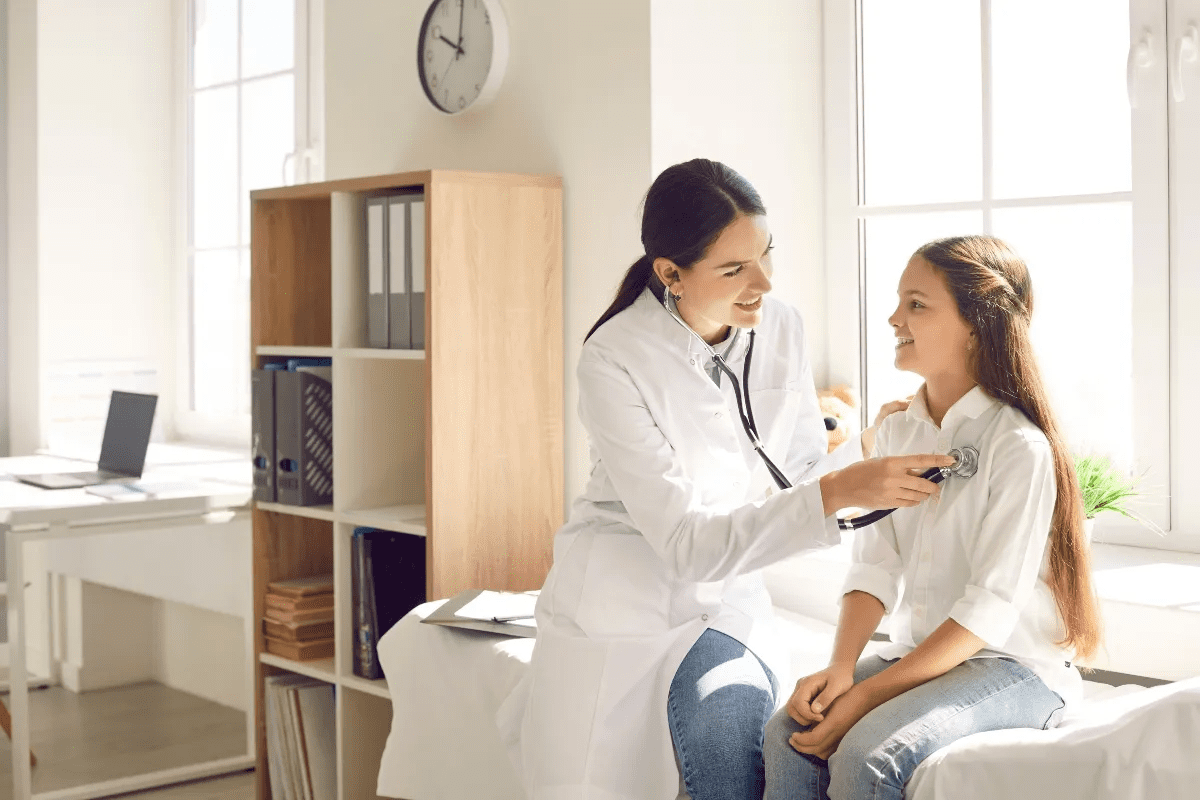
Diagnosing Uveitis: The Clinical Approach
To diagnose uveitis, doctors use many tools and methods. It’s not just about looking at the eye. They need to find the cause of the inflammation and rule out other issues.
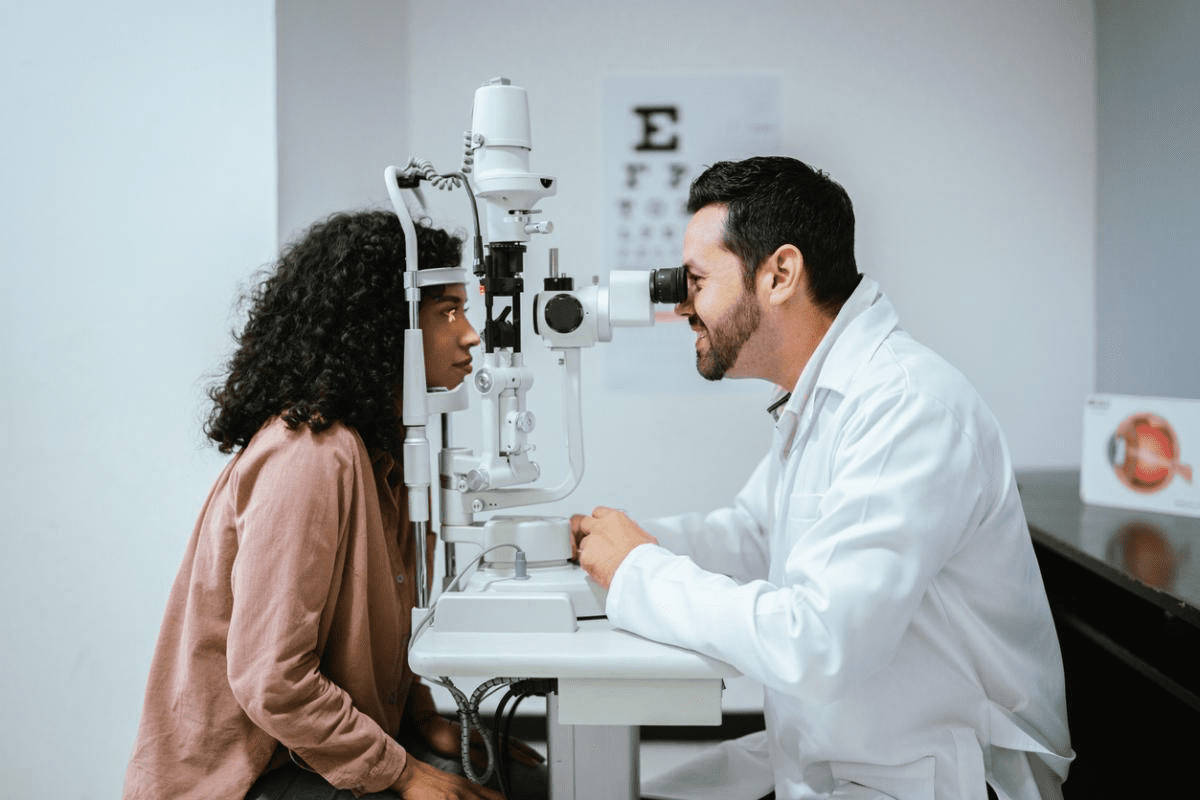
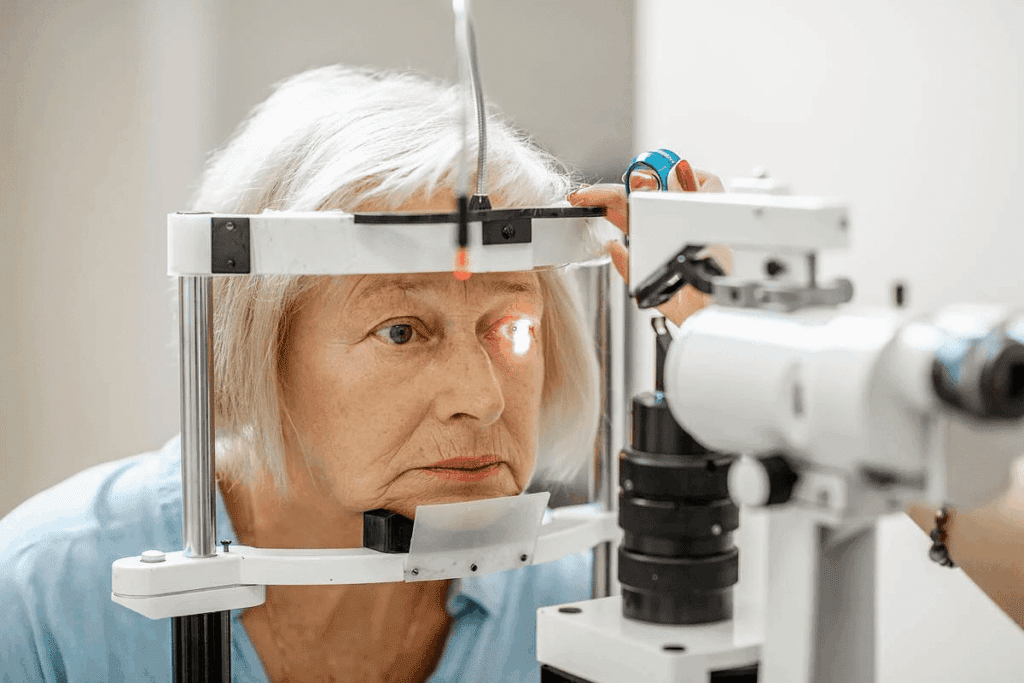
Comprehensive Eye Examination
The first step is a detailed eye check. This includes a medical history, vision tests, and a slit-lamp exam. A thorough eye exam helps doctors understand the type and severity of uveitis.
Laboratory Tests for Autoimmune Markers
Lab tests are key in finding the cause of uveitis, like autoimmune diseases. Tests for antinuclear antibodies (ANA) or rheumatoid factor (RF) are common. These tests help doctors see if an autoimmune disease is involved.
Imaging Studies
Imaging helps doctors see how bad the inflammation is. Optical coherence tomography (OCT) and fluorescein angiography give detailed eye images. This helps doctors understand the severity and track changes.
Ruling Out Infectious Causes
It’s important to check for infections that could cause uveitis. Tests for things like toxoplasmosis or herpes simplex virus are used. A detailed diagnostic process is needed to find the right cause.
Doctors use eye exams, lab tests, and imaging to accurately diagnose uveitis. This way, they can create a treatment plan that fits the patient’s needs.
Differentiating Between Autoimmune and Infectious Uveitis
It’s important to tell the difference between autoimmune and infectious uveitis for the best treatment. Uveitis is a serious eye condition that can cause vision loss. Knowing the cause helps doctors treat it right.
Key Differences in Presentation
Autoimmune uveitis and infectious uveitis show different signs. Autoimmune uveitis often comes with other diseases like ankylosing spondylitis. It usually affects both eyes. On the other hand, infectious uveitis is caused by germs and can look different based on the germ.
Knowing these differences helps doctors choose the right tests and treatments. For example, autoimmune uveitis might need drugs to calm the immune system. But infectious uveitis needs antibiotics or antiviral drugs.
Diagnostic Challenges
Figuring out what causes uveitis can be hard. Both types can have similar symptoms like eye pain and blurry vision. This makes it tricky to diagnose.
To solve this, doctors use a detailed approach. They look at the patient’s history, do eye exams, run tests, and use imaging. Tests might check for signs of autoimmune diseases or germs.
Importance of Accurate Diagnosis for Treatment
Getting the right diagnosis is key for treating uveitis. If doctors get it wrong, the treatment might not work. This could make the condition worse and even cause permanent vision loss.
For autoimmune uveitis, doctors use drugs to fight inflammation. But for infectious uveitis, they need to target the germ causing it.
Characteristics | Autoimmune Uveitis | Infectious Uveitis |
Cause | Associated with systemic autoimmune diseases | Caused by pathogens (bacteria, viruses, fungi) |
Presentation | Often bilateral, associated with systemic symptoms | Varies depending on the causative agent, can be unilateral or bilateral |
Treatment | Immunosuppressive therapy | Antimicrobial therapy |
In conclusion, telling autoimmune uveitis from infectious uveitis is vital for the right treatment. A detailed check-up is needed to figure out which one it is.
Treatment Approaches for Autoimmune Eye Disease
Managing autoimmune uveitis needs a mix of treatments to fight inflammation and save vision. We’ll look at how to treat this condition, focusing on reducing inflammation and keeping vision sharp.
Anti-inflammatory Medications
Anti-inflammatory meds, mainly corticosteroids, are key in treating autoimmune uveitis. They quickly cut down inflammation and ease symptoms. But, long-term use can cause serious side effects, so careful management is needed.
Corticosteroids are often the first choice for treating acute uveitis flare-ups. They can be applied topically, injected, or taken orally, based on the inflammation’s severity and location.
Immunosuppressive Therapy
For long-term management or severe disease, immunosuppressive therapy is used. This method uses drugs to weaken the immune system, reducing inflammation and preventing damage.
Immunosuppressive drugs can be used alone or with corticosteroids. This helps lower steroid doses and reduces their side effects.
Biologic Agents
Biologic agents are a newer treatment option that targets specific immune responses. They’re great for patients who don’t respond to traditional immunosuppressive therapy.
Biologics have shown great promise in treating autoimmune uveitis. They reduce inflammation and improve vision. Their use is customized based on the patient’s condition and response.
Local vs. Systemic Treatment
The choice between local and systemic treatment depends on the uveitis’s extent and severity, and the patient’s health. Local treatments, like intravitreal injections, are preferred for their targeted action and fewer side effects.
Systemic treatments are used for bilateral disease or when it’s linked to systemic autoimmune conditions. The choice is based on a thorough patient assessment.
Managing Complications and Preventing Vision Loss
Managing uveitis well is key to keeping your vision safe and preventing damage. Uveitis, linked to autoimmune disorders, can cause serious problems if not treated right.
Common Complications of Uveitis
Uveitis can lead to cataracts, glaucoma, retinal detachment, and macular edema. These issues can hurt your vision and quality of life. Early treatment is key to avoiding or lessening these problems.
- Cataract formation due to chronic inflammation or steroid use
- Glaucoma resulting from increased intraocular pressure
- Retinal detachment, which can cause sudden vision loss
- Macular edema, leading to swelling and vision distortion
Strategies to Preserve Vision
Keeping vision safe in uveitis patients needs a detailed plan. This includes controlling inflammation, managing complications, and stopping it from coming back. Customizing treatment for each patient is vital for the best results.
Strategies include:
- Using anti-inflammatory and immunosuppressive medications to control uveitis
- Implementing regular monitoring to detect complications early
- Adjusting treatment plans as needed to prevent flare-ups
- Educating patients on the importance of adherence to treatment and follow-up appointments
Regular Monitoring and Follow-up
Regular check-ups and follow-up are vital in managing uveitis. Regular eye exams help catch complications early and check if treatment is working. Changes to treatment plans can then be made to get better results.
Follow-up care should include:
- Regular eye exams to monitor disease activity and complications
- Assessment of visual acuity and quality of life
- Adjustments to medication based on disease activity and side effects
By being proactive and detailed in managing uveitis, we can greatly improve patient outcomes and protect vision.
Living with Autoimmune Uveitis: Lifestyle and Psychological Considerations
Living with autoimmune uveitis can be tough, but there are ways to make life better. A good plan includes medical care, lifestyle changes, and mental support.
Coping with Flare-ups
Handling flare-ups of autoimmune uveitis needs both medical help and lifestyle changes.
- Medication Adherence: It’s key to take your meds as told to manage flare-ups.
- Rest and Relaxation: Rest well and try relaxation methods like meditation to lessen stress and symptoms.
- Protecting Your Eyes: Wear sunglasses with UV protection and stay away from things that might irritate your eyes.
Dietary and Environmental Considerations
What you eat and your environment can help manage autoimmune uveitis.
- Anti-inflammatory Diet: Eating foods that fight inflammation, like fruits, veggies, and omega-3s, can help.
- Avoiding Triggers: Stay away from things that might trigger flare-ups, like smoking or certain chemicals.
Quitting smoking can really help with uveitis. There are many programs and resources for those with autoimmune eye disease who want to stop smoking.
The Psychological Impact of Chronic Eye Conditions
Autoimmune uveitis can really affect your mind, impacting your mental health and happiness.
- Stress and Anxiety: Living with a chronic eye condition can make you feel stressed and anxious.
- Support Systems: Having people you can count on, like family and friends, is very important for dealing with the mental side of the condition.
Support Resources for Patients
There are many resources for people with autoimmune uveitis, including:
- Support groups, online or in-person, where you can share and get advice.
- Mental health experts who can offer counseling and therapy.
- Info and resources that help you understand and manage your condition.
Conclusion
Uveitis is a complex eye condition linked to autoimmune disorders. It happens when the body’s immune system attacks the uvea. This leads to inflammation and can cause severe vision loss.
It’s important to see uveitis as an autoimmune disease for effective treatment. With the right diagnosis and treatment, most people can live full lives with good vision. This is true for those with uveitis and diseases like ankylosing spondylitis and inflammatory bowel disease.
Understanding the immune system’s role in uveitis helps doctors create better treatments. These treatments aim at the root causes of the condition. This approach helps manage symptoms and lowers the risk of vision problems.
As research grows, we can better care for those with uveitis and autoimmune diseases. This means giving patients the support they need to manage their conditions well.
FAQ
What is uveitis and how is it related to autoimmune diseases?
Uveitis is a serious eye condition where the eye’s uvea gets inflamed. It can happen when the body’s immune system attacks its own tissues, including the eye.
Is uveitis considered an autoimmune disease?
Yes, in some cases, uveitis is seen as an autoimmune disease. This is when the inflammation is caused by an abnormal immune response. Many uveitis cases are linked to autoimmune issues.
What are the common symptoms of autoimmune uveitis?
Symptoms include eye pain, redness, and blurred vision. You might also see floaters and feel sensitive to light. Sometimes, you might have joint pain or skin rashes too.
How is autoimmune uveitis diagnosed?
Doctors do a detailed eye exam and run lab tests to find autoimmune markers. They might also use imaging studies. It’s important to check for infections first to treat it right.
What are the treatment approaches for autoimmune uveitis?
Treatment options include anti-inflammatory meds, immunosuppressive therapy, and biologic agents. The choice depends on how severe the disease is.
Can uveitis lead to blindness if left untreated?
Yes, if not treated quickly and well, uveitis can cause blindness. It’s key to keep an eye on it and follow up regularly to avoid serious problems.
What lifestyle changes can help manage autoimmune uveitis?
Making lifestyle changes can help. This includes coping with flare-ups, eating right, and avoiding things that might make it worse. Stress management and support are also important.
Are there any systemic autoimmune diseases commonly associated with uveitis?
Yes, diseases like ankylosing spondylitis, inflammatory bowel disease, Behcet’s disease, and autoimmune thyroiditis are linked to uveitis.
How does the immune system contribute to autoimmune uveitis?
The immune system’s wrong response, including T cell issues and breaking down eye protection, is key in autoimmune uveitis.
What is the role of biologic agents in treating autoimmune uveitis?
Biologic agents target the immune response that causes inflammation. They are a good option for those who don’t get better with usual treatments.