Dermal fillers are a popular choice for facial enhancements without surgery. But, injecting them into a blood vessel can cause vascular occlusion. This is a serious complication that needs quick action.
It’s vital to know the warning signs of vascular occlusion after getting fillers. Look out for sudden pain, changes in skin color, or unusual bruising. If ignored, it can lead to severe damage, like tissue necrosis.
Quick action is key to avoid lasting harm. Knowing the risks of dermal fillers and the signs of vascular occlusion helps protect your health. By being proactive, you can ensure your safety.
Know the 5 warning signs of blood vessel occlusion after filler. This is a critical, time-sensitive emergency. Learn what to look for.
Key Takeaways
- Recognizing the signs of vascular occlusion is key after dermal filler injections.
- Sudden pain and skin discoloration are key indicators of vascular occlusion.
- Prompt medical attention is necessary to prevent severe consequences.
- Understanding the risks associated with dermal fillers can help in taking preventive measures.
- Timely intervention can significantly reduce the risk of long-term damage.
Understanding Vascular Occlusion in Dermal Fillers
It’s key for those giving dermal fillers to know about vascular occlusion. This serious issue can happen if not caught and treated fast. With more people getting dermal fillers, vascular occlusion cases are also rising.
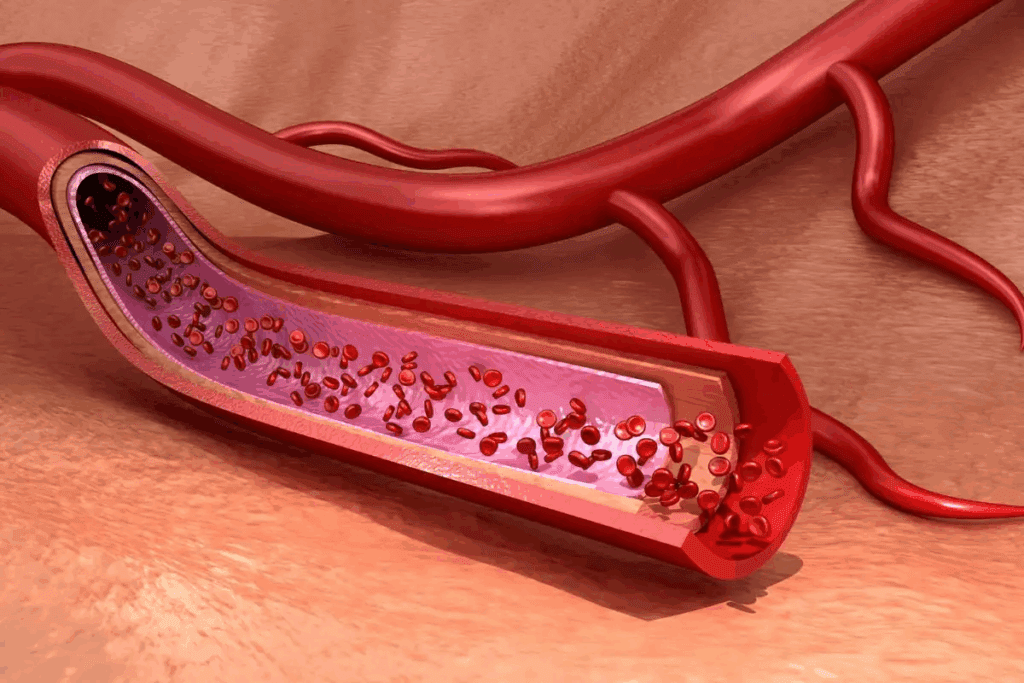
Definition and Mechanism of Occlusion
Vascular occlusion happens when a blood vessel gets blocked by filler. This can cause tissue to not get enough blood, leading to serious problems. These problems can include acute pain and even permanent scarring.
Even with careful technique, vascular occlusion can occur. So, it’s vital for doctors to know the risks and spot symptoms of vascular occlusion early.
Prevalence and Statistics in Aesthetic Medicine
Vascular occlusion is rare, happening in about 0.01 to 0.05 percent of treatments. But, with so many filler treatments happening, more cases are seen. In the U.S., over 4 million treatments are done each year, making quick action important.
The risk of vascular occlusion is real and can affect both patients and doctors. Knowing how common it is helps in keeping care safe and effective.
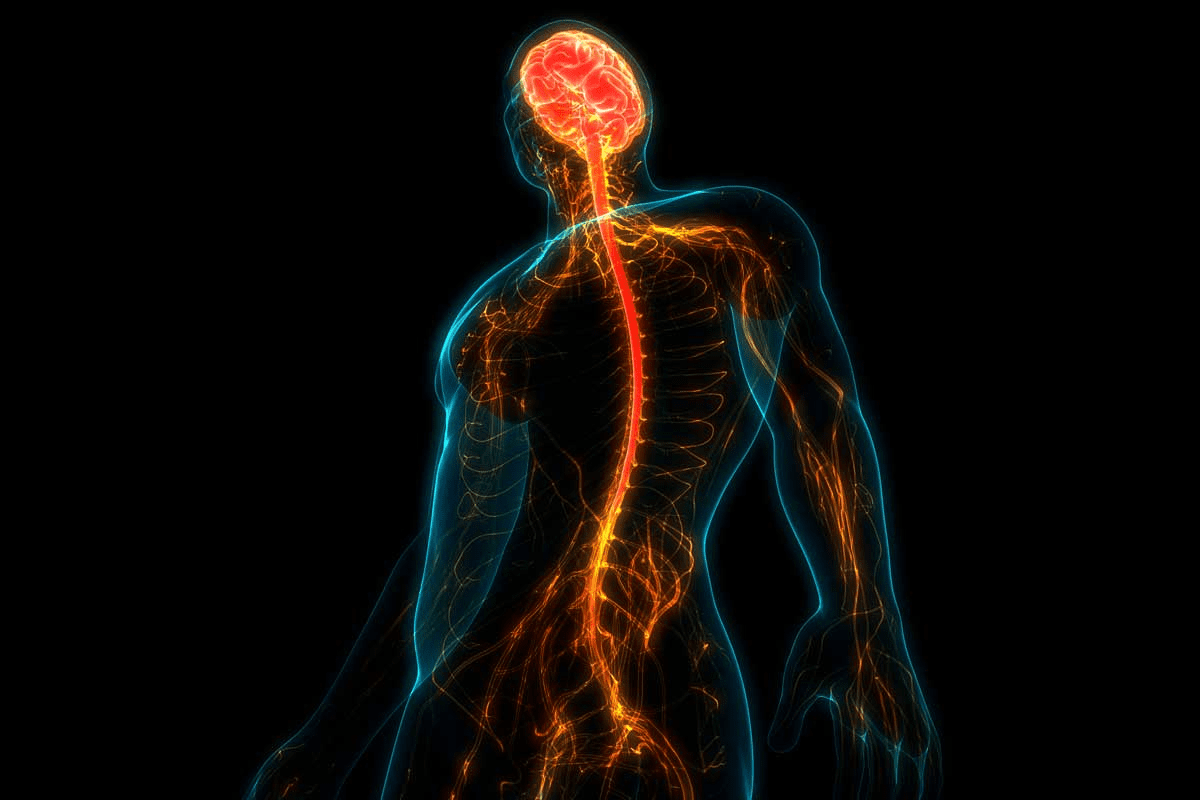
The Science Behind Blood Vessel Occlusion in Filler Procedures
The science behind blood vessel occlusion in filler procedures is complex. It involves many anatomical and physiological factors. Vascular occlusion is a serious complication that can happen with dermal filler injections. It’s important to understand its mechanisms to prevent and manage it effectively.
Vascular occlusion can happen in two main ways: intravascular embolism and external compression. Intravascular occlusion occurs when filler material is accidentally injected into an artery or vein. This can cause an embolism, leading to tissue ischemia or even necrosis. External compression happens when the filler material presses on a blood vessel from the outside, blocking blood flow.
Intravascular vs. External Compression Mechanisms
Intravascular occlusion is more severe and can be catastrophic. Direct injection into an artery can cause the filler material to block smaller vessels, leading to tissue necrosis. External compression is also serious but symptoms may develop more slowly.
Both mechanisms can cause significant problems, including pain, skin discoloration, and even vision loss. These complications are more likely in high-risk areas.
Anatomical Considerations in Vascular Events
Knowing the anatomy is key to preventing vascular occlusion. Certain facial areas are at higher risk due to their vascular anatomy. For example, the glabellar region and the nasal area have complex vascular networks.
- The glabellar region is risky due to its dense vascular network and anastomoses between major arteries.
- The nasal area, including the nasolabial fold, is also high-risk. It has a rich vascular supply and can be prone to filler material injection or compression.
Understanding these anatomical considerations is vital for practitioners. It helps them minimize the risk of vascular occlusion during filler procedures. By knowing the risks and taking precautions, we can reduce complications.
Hyaluronic acid fillers, which make up about 80% of the market, can cause vascular occlusion complications. While rare, other fillers like calcium hydroxylapatite and poly-L-lactic acid can also lead to vascular events. The key to managing these risks is a deep understanding of facial anatomy, precise injection techniques, and recognizing early warning signs.
Common Types of Fillers and Associated Occlusion Risks
Many types of fillers are used in cosmetic treatments. Each has its own benefits and risks. Knowing these risks is important for both doctors and patients.
Hyaluronic Acid Fillers
Hyaluronic acid fillers are the most popular, making up 80% of the market. They are known for being safe and easy to reverse. But, they are also linked to most cases of vascular occlusion.
Key characteristics of hyaluronic acid fillers include:
- High patient satisfaction rates
- Reversible with hyaluronidase
- Variety of formulations for different applications
Even though they are safe, hyaluronic acid fillers can cause vascular occlusion if not injected right. Doctors need to know the anatomy and use the right technique to avoid risks.
Calcium Hydroxylapatite Products
Calcium hydroxylapatite fillers are also popular. They last longer and help produce collagen. But, they can’t be reversed like hyaluronic acid fillers, which makes vascular occlusion riskier.
Important considerations for calcium hydroxylapatite fillers:
- Longer-lasting results compared to hyaluronic acid fillers
- Not reversible, making precise placement critical
- Potential for nodule formation
There have been cases of vascular occlusion with calcium hydroxylapatite fillers. This shows the need for experienced doctors.
Poly-L-Lactic Acid and Other Fillers
Poly-L-lactic acid fillers stimulate collagen production over time. Other fillers, like polymethylmethacrylate, have their own risks and benefits.
Risks associated with poly-L-lactic acid and other fillers:
- Gradual onset of effect, which can make immediate complications harder to detect
- Potential for delayed complications
- Importance of proper dilution and injection technique
Even though less common, these fillers can also cause vascular occlusion. It’s important to carefully evaluate patients and administer the fillers skillfully.
In conclusion, different fillers have different risks and benefits. Understanding these differences is key to avoiding complications like vascular occlusion. Doctors need to stay updated on the latest research and guidelines to keep patients safe.
High-Risk Anatomical Areas for Vascular Complications
Some facial areas face a higher risk of vascular problems because of their complex blood vessel layout. Knowing these high-risk spots is key for doctors to avoid issues during dermal filler treatments.
Nasolabial Fold and Perioral Region
The nasolabial fold is often chosen for filler injections because it’s so noticeable. But, it’s also packed with blood vessels, making it a risky spot for blockages. The close proximity to big blood vessels and the dense smaller ones raise the chance of blood vessel problems.
When filling the nasolabial fold, doctors need to be careful. They should use a smaller needle and inject slowly, watching for any signs of blood vessel trouble.
Glabellar and Nasal Danger Zones
The glabellar area, between the eyebrows, is also at high risk because of its blood vessel layout. Its large vessels that connect to deeper ones make it prone to serious issues. The nasal area is also risky because of its many blood vessels and connections to deeper ones.
Doctors should be extra careful when working on these spots. They might choose to use cannulas instead of needles and use methods that lower the risk of blood vessel problems.
Temple, Forehead, and Other Vulnerable Sites
The temple and forehead are also at risk for blood vessel problems. This is because of the big vessels near the surface. The temporal area, in particular, has branches of the temporal artery that can get damaged during injections.
To lessen these risks, doctors need to know the blood vessel layout in these areas well. They should also use safe injection methods.
High-Risk Area | Vascular Risks | Precautionary Measures |
Nasolabial Fold | Intravascular injection, external compression | Use smaller gauge needles, inject slowly |
Glabellar Region | Deep vessel communication, serious complications | Consider using cannulas, minimize intravascular injection |
Temple and Forehead | Superficial significant vessels | Understand vascular anatomy, use safe injection techniques |
Immediate Warning Signs of Blood Vessel Occlusion
It’s important to know the signs of blood vessel occlusion after getting dermal fillers. This condition can show up with clear signs, like sudden or growing pain at the injection site or elsewhere.
Acute Pain: Characteristics and Patterns
Acute pain is a common warning sign of vascular occlusion. This pain can be very strong and happen right during or after the injection. It’s key to tell this pain apart from the usual discomfort of getting the injection.
The pain’s feel and pattern can differ, but it’s often a sharp, intense feeling that doesn’t go away.
White Blanching: Recognition and Significance
White blanching, or sudden skin paleness, is another important sign. It happens when blood flow to the area is cut off. Spotting white blanching is critical because it shows a possible blockage in the blood vessel.
Practitioners need to be quick to act if they see this sign.
Immediate Skin Color Changes and Their Meaning
Color changes in the skin can also mean vascular occlusion. These changes might include white blanching or other colors like blue or purple, showing poor blood flow. Knowing what these color changes mean is key for catching and handling vascular occlusion early.
The main signs to look out for are:
- Severe pain during or after injection
- White blanching of the skin
- Immediate changes in skin color
Staying alert to these signs helps doctors act fast, which can stop serious problems. It’s also important for patients to know these signs. This way, they can get help right away if they see them.
Delayed Manifestations of Vascular Occlusion
It’s key to spot signs of vascular occlusion early. Some signs show up right away, but others can take hours or days. Keeping an eye out for these signs is vital to treat them quickly and avoid problems.
Progressive Skin Changes Hours After Treatment
After getting dermal fillers, skin changes can happen hours later. These might include skin darkening or discoloration, which could mean serious issues. It’s important to teach patients to watch for these changes and tell us if they see anything odd.
A medical expert says, “Delayed skin changes can warn of vascular problems. We must stay alert and act fast.”
“The key to managing vascular occlusion lies in early detection and swift intervention. Delayed manifestations require careful monitoring and a proactive approach.”
— Medical Expert, Aesthetic Medicine Specialist
Development of Livedo Reticularis Pattern
Livedo reticularis, a skin discoloration, can signal vascular occlusion. It might show up hours to days post-procedure. We need to know about this and tell our patients it’s a big warning sign.
Late-Onset Symptoms Requiring Attention
Signs of vascular occlusion can pop up later, like ongoing pain, skin death, or color changes. These need quick checking and treatment to avoid lasting harm. We should stress the need for follow-up visits and tell patients to speak up if they notice anything off.
Symptom | Onset | Action Required |
Progressive Skin Changes | Hours to Days | Monitor Closely, Report Changes |
Livedo Reticularis | Hours to Days | Immediate Medical Attention |
Late-Onset Pain or Discoloration | Days | Prompt Evaluation and Treatment |
Knowing about these late signs of vascular occlusion helps us give better care. This way, we can lower the chance of problems and make sure our patients get the best results.
Site-Specific Signs of Vascular Occlusion
Vascular occlusion shows different signs in various body parts. It’s important to know these signs well for quick and right treatment.
Lip Filler Complications and Unique Presentations
Lip fillers are mostly safe but can cause vascular problems. Lip filler complications might show up as:
- Blanching or discoloration of the lip
- Pain or tenderness in the lip area
- Swelling or asymmetry
These signs mean you might have vascular occlusion and need to see a doctor right away.
Cheek and Midface Indicators
The cheek and midface are common places for fillers. Cheek filler issues can show as:
Signs | Possible Indications |
Skin discoloration | Vascular compromise |
Pain or discomfort | Ischemia or occlusion |
Swelling or inflammation | Reaction to filler or vascular event |
Chin, Jawline, and Temple Warning Signs
Fillers in the chin, jawline, and temple can also cause vascular occlusion. Chin filler and vascular occlusion chin filler problems might include:
- Numbness or paresthesia in the treated area
- Visible changes in skin color or texture
- Pain or discomfort that persists or worsens
Knowing these specific signs is key to spotting and treating vascular occlusion right. By recognizing these signs in different areas, doctors can give the best care quickly.
Differentiating Normal Side Effects from Vascular Emergencies
It’s important for both patients and doctors to know the difference between normal side effects and serious vascular problems after getting dermal fillers. Knowing this helps keep patients safe and ensures they get the right help when they need it.
Expected Post-Procedure Reactions
After getting dermal fillers, people might see some swelling, bruising, or redness where the needle was. These are usually mild and go away in a few days. Common expected reactions include:
- Mild bruising
- Swelling
- Redness
- Slight tenderness
These side effects are usually nothing to worry about and are just a normal part of the healing process.
Red Flags That Require Immediate Medical Attention
But, there are some signs that mean something more serious might be happening, like vascular occlusion. Immediate medical attention is required if patients experience:
- Severe pain that is not relieved by pain medication
- Skin discoloration, specially if it’s big or comes with other symptoms
- Progressive swelling or bruising that gets worse over time
- Difficulty moving facial muscles or other neurological symptoms
These signs can mean vascular occlusion or other serious problems that need quick treatment.
Patient Self-Monitoring Guidelines
It’s key to teach patients how to watch for changes after getting dermal fillers. They should be told to:
- Keep an eye on the injection site for any unusual changes
- Watch for signs of infection, like more redness, swelling, or pus
- Tell their healthcare provider right away if they have severe or getting worse symptoms
- Go to their follow-up appointments as scheduled
By staying alert and informed, patients can help prevent serious problems and aid in their recovery.
Diagnostic Approaches for Suspected Occlusion
Diagnosing vascular occlusion accurately is key. It requires a mix of clinical checks, advanced imaging, and detailed documentation. We’ll dive into these methods to help healthcare teams tackle vascular occlusion well.
Clinical Evaluation Techniques
First off, clinical evaluation is vital for diagnosing vascular occlusion. It involves checking the patient’s symptoms and doing a physical exam. Important techniques include:
- Checking capillary refill time to see if blood flow is okay.
- Looking for skin color changes like blanching or livedo reticularis, signs of vascular issues.
- Feeling for pain or tenderness, as sudden pain can mean vascular occlusion.
Capillary Refill Assessment is a simple yet effective way to check skin microcirculation. If capillary refill time is long, it might mean blood flow is blocked.
Imaging and Advanced Diagnostic Tools
Along with clinical checks, imaging and advanced tools are key to confirming vascular occlusion. These include:
- Doppler Ultrasound: Great for checking blood flow in affected vessels.
- Angiography: Gives detailed views of the vascular system and spots occlusions.
- Near-Infrared Spectroscopy (NIRS): Helps check tissue oxygen levels and spot vascular problems.
The right imaging choice depends on the situation and what’s available. Quick and precise imaging is vital for managing vascular occlusion.
Documentation Protocols for Medical Providers
Good documentation is critical for both medical and legal reasons. It should cover:
Documentation Aspect | Description |
Patient History | A detailed record of the patient’s medical history, including past filler treatments. |
Procedure Details | Notes on the filler procedure, like the type and amount used. |
Symptoms and Signs | A record of the patient’s symptoms and clinical findings. |
Diagnostic Results | Results from any imaging or diagnostic tests. |
Treatment and Follow-Up | Details on the treatment given and future care plans. |
Accurate and detailed documentation helps manage vascular occlusion and serves as a legal record of events and actions.
Emergency Response Protocol for Vascular Occlusion
An emergency response plan is key for handling vascular occlusion well. Quick and right actions can greatly help patient results.
Immediate Steps for Practitioners
When we see signs of vascular occlusion, we must act fast. First, we stop the injection or procedure right away. Then, we check how bad the occlusion is.
Key immediate steps include:
- Discontinue the procedure
- Assess the patient’s condition
- Administer appropriate treatment
Hyaluronidase Administration for HA Fillers
For HA filler occlusions, hyaluronidase is the best fix. We use it to break down the filler and get blood flowing again.
The right dose and how we give it are very important. We stick to the rules to treat well and avoid bad side effects.
Additional Interventions and Medications
Along with hyaluronidase, we might need more steps. This could be creams, massage, or other meds to help symptoms and aid healing.
We look at each patient’s needs and the occlusion details to pick the best action.
When to Refer to Emergency Medical Services
It’s important to know when to call for emergency help. If the occlusion is really bad or if there’s a lot of tissue damage, we call for more medical aid.
Indicators for referral include:
- Severe pain
- Significant skin discoloration
- Evidence of tissue necrosis
With a solid emergency plan, we can tackle vascular occlusion well and cut down on problems.
Conclusion: Prevention Strategies and Patient Education
Preventing vascular occlusion is a team effort. It involves educating doctors, following safe injection rules, and teaching patients. Knowing the risks and signs helps make aesthetic treatments safer.
Good prevention means knowing facial anatomy well and using safe injection methods. It also means teaching patients about warning signs. We stress the importance of patient education in lowering vascular occlusion risks. Patients need to know the risks and report any unusual symptoms after treatments.
Preventing vascular occlusion needs teamwork between doctors and patients. Together, we can lower the chances of complications from dermal fillers.
FAQ
What is vascular occlusion in the context of dermal fillers?
Vascular occlusion happens when a filler blocks a blood vessel. This can be through direct injection or external pressure. It leads to reduced blood flow and can harm the tissue.
What are the immediate signs of vascular occlusion after filler injections?
You might feel sudden pain, see white blanching, or notice skin color changes right away. These signs need quick action to avoid serious problems.
How does the type of filler used affect the risk of vascular occlusion?
Different fillers, like hyaluronic acid or calcium hydroxylapatite, have different risks. This is because of their unique features and how they work in the body.
What are the high-risk anatomical areas for vascular complications during filler procedures?
Certain areas, like the nasolabial fold or the glabellar region, are at higher risk. This is because of their complex blood vessels.
Can vascular occlusion symptoms be delayed, and if so, what are they?
Yes, some symptoms can show up hours later. Look out for skin changes, a livedo reticularis pattern, or late-onset symptoms that need medical help.
How can practitioners differentiate between normal side effects and signs of vascular occlusion?
Know what normal reactions are after a treatment. Look out for red flags like severe pain, skin color changes, or other unusual signs that need immediate care.
What is the role of hyaluronidase in treating vascular occlusion caused by hyaluronic acid fillers?
Hyaluronidase is an enzyme that breaks down hyaluronic acid fillers. It’s used right away to treat vascular occlusion caused by these fillers. It helps restore blood flow and prevent damage.
What are the key diagnostic approaches for suspected vascular occlusion?
To diagnose, use clinical checks, imaging, and advanced tools. Also, keep detailed records to accurately diagnose and manage vascular occlusion.
When should a patient be referred to emergency medical services for vascular occlusion?
Refer patients to emergency services for severe symptoms like significant tissue damage, vision issues, or other serious problems. Or if initial treatments don’t work.
How can vascular occlusion be prevented during filler procedures?
Prevention involves education for practitioners, safe injection methods, and patient awareness. Teach patients about the risks and signs of vascular occlusion and how to reduce these risks.
What are the signs of vascular occlusion after lip fillers?
Look out for acute pain, white blanching, and immediate skin color changes. Also, watch for delayed symptoms like skin changes or livedo reticularis.
What is the significance of white blanching after filler injections?
White blanching is a key sign of vascular occlusion. It means there’s no blood flow to the area. It needs quick action to restore blood flow and prevent tissue damage.
References
National Health Service (NHS). Vascular Occlusion After Filler: Recognition and Prompt Action. Retrieved from https://www.england.nhs.uk/publication/facial-aesthetic-non-surgical-procedures-guidance/