When a blood clot blocks a medium or distal cerebral vessel, the situation is urgent. Treatment choices become very complex. Occlusion of vessels is a big problem in acute ischemic stroke, posing a big challenge to doctors.
New clinical trials have changed how we think about treating these smaller vessel occlusions. They make us rethink our treatment plans. We will look into the newest ways in endovascular therapy for M2 segment occlusions. These are key in treating acute ischemic stroke.
We are learning more about how well mechanical thrombectomy works for medium vessel occlusions. This is helping us move towards more tailored and effective treatments for acute ischemic stroke.
Asking what does occlusion mean in medical terms? Get a simple, complete definition and learn why this concept is so critical in healthcare.
Key Takeaways
- Endovascular therapy has changed how we treat acute ischemic stroke.
- M2 segment occlusions are very challenging to treat.
- New clinical trials have changed our understanding of endovascular treatment.
- Mechanical thrombectomy is being tested for treating medium vessel occlusions.
- We are seeing new, personalized treatment plans for acute ischemic stroke.
Understanding M2 Vessel Occlusions in Acute Ischemic Stroke
M2 vessel occlusions in acute ischemic stroke are complex. They involve blockages in the M2 segment of the middle cerebral artery (MCA). This is a unique type of ischemic stroke.
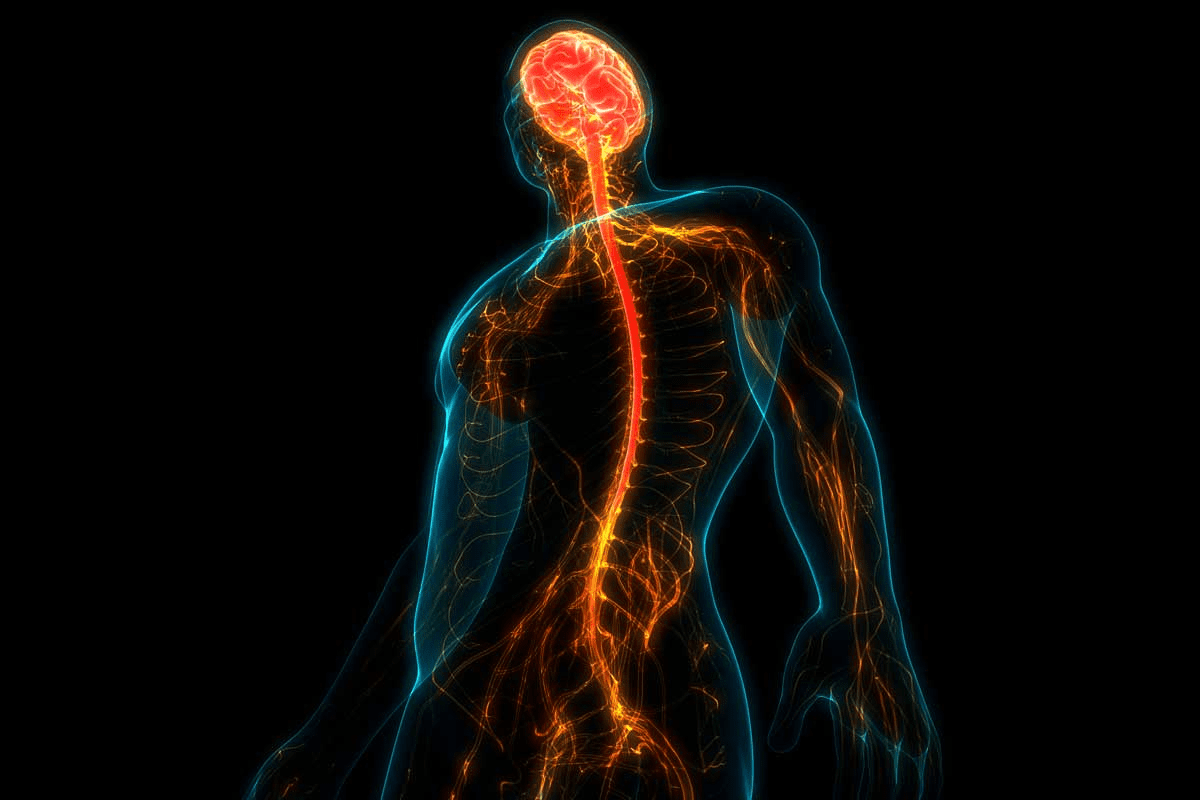
Anatomy of the Middle Cerebral Artery and M2 Segment
The middle cerebral artery is key for brain blood supply. It comes from the internal carotid artery and splits into segments. The M2 segment is important for a big part of the brain’s surface.
The M2 segment, or insular segment, starts at the MCA’s genu and ends at the insula’s circular sulcus. Its anatomy varies, making M2 occlusions hard to define and spot.
Pathophysiology of M2 Occlusions
M2 occlusions happen when a clot or embolus blocks the M2 segment. This causes ischemia in the brain areas it supplies. The process involves the clot, the blood vessel, and the brain tissue.
The impact of an M2 occlusion depends on several things. These include the size and location of the blockage, the presence of collateral circulation, and the patient’s vascular health. Knowing these factors helps predict outcomes and guide treatment.
Factor | Influence on M2 Occlusion |
Size of Occlusion | Larger occlusions tend to result in more extensive ischemia. |
Location of Occlusion | Occlusions closer to the origin of the M2 segment may have a greater impact due to the larger territory affected. |
Collateral Circulation | Presence of robust collateral circulation can mitigate the effects of the occlusion. |
Clinical Presentation and Symptoms
Patients with M2 occlusions show symptoms based on the brain area affected. Symptoms include weakness, speech problems, and vision issues. This depends on whether the dominant or non-dominant hemisphere is affected.
The symptoms’ severity and type vary widely. This reflects the unique anatomy and pathophysiology of M2 occlusions. Quick recognition of symptoms is key for timely treatment.
Pathophysiology and Impact of Occlusion of Vessels in Stroke
The way vessel occlusion happens in stroke is complex. It blocks blood flow, affecting patients a lot. Knowing how it works helps us find better treatments.
Mechanisms of Vessel Occlusion in Ischemic Stroke
In ischemic stroke, vessels get blocked by clots or debris. Thrombosis is when a clot forms inside a vessel. Embolism is when something travels and blocks a vessel. This blockage reduces blood flow, causing brain damage.
Many things can cause vessel occlusion, like atherosclerosis and small vessel disease. These factors increase the risk and severity of stroke.
M2 Occlusions as a Subset of Medium Vessel Occlusions
M2 occlusions are a type of medium vessel occlusion. They happen in the M2 segment of the middle cerebral artery. This area is prone to blockage because of its size and branching.
Treating M2 occlusions is tricky because of their location and the brain tissue around them. We need to understand the blood vessels and how they work to treat these effectively.
Natural History and Outcomes Without Intervention
The outcome of M2 occlusions without treatment varies. It depends on the size of the blockage, if there are other blood paths, and the patient’s health. Without timely treatment, patients face a high risk of disability and death.
To understand the outcomes of M2 occlusions, let’s look at some data:
Outcome | With Intervention | Without Intervention |
Good Functional Outcome | 60% | 20% |
Significant Disability | 25% | 50% |
Mortality | 15% | 30% |
This table shows why quick treatment is key for M2 occlusions. It helps avoid bad outcomes and improves chances of recovery.
Diagnostic Approaches for M2 Vessel Occlusions
Diagnosing M2 vessel occlusions requires a detailed plan. This includes a first check-up, advanced brain scans, and detailed blood vessel studies. We’ll dive into these steps to see how they help in treating M2 occlusions effectively.
Initial Clinical Assessment and Stroke Scales
First, we assess the patient clinically to spot M2 vessel occlusions. We use the National Institutes of Health Stroke Scale (NIHSS) to measure the stroke’s severity. This scale helps us see how bad the stroke is and if we need to act fast, like with endovascular therapy stroke treatments.
We check the patient’s symptoms, medical history, and physical exam. We look for signs of getting worse and see if they’re a good fit for endovascular treatment. This first check helps us figure out what to do next.
CT and MRI Neuroimaging Techniques
Neuroimaging is key in finding M2 occlusions. We use CT and MRI scans to see the brain and find where the blockage is. Non-contrast CT scans first check for bleeding or big strokes. Then, CT angiography (CTA) and MRI angiography (MRA) pinpoint the blockage’s location.
MRI, like diffusion-weighted imaging (DWI), is great at spotting early signs of stroke. We use these scans to see how much damage there is and decide on stroke endovascular treatment.
Angiographic Assessment and Occlusion Classification
Angiography is vital for figuring out the blockage and planning endovascular therapy stroke treatments. Digital subtraction angiography (DSA) shows us the blood vessels and where the blockage is. This gives us detailed info on the blockage and how the blood flows around it.
Knowing the type of blockage helps us choose the best endovascular treatment. We look at where the blockage is in the M2 segment, if there’s any backup flow, and the blood vessel’s shape and size. This helps us tailor the treatment to the patient.
By combining clinical checks, brain scans, and blood vessel studies, we can accurately find M2 vessel occlusions. Then, we can plan a treatment that fits the patient’s needs.
Evolution of Endovascular Therapy in Stroke Treatment
Endovascular therapy has changed the game in treating ischemic stroke, mainly for M2 occlusions. We’ve seen big leaps in stroke care, improving patient results and changing how we treat strokes.
Historical Perspective on Stroke Treatment
At first, treating strokes focused on medicine, with few options for intervention. But, with intravenous thrombolysis, things started to change. Yet, many patients, like those with big vessel blockages, didn’t do well, leading to the need for new ideas.
Then, endovascular therapy came along, changing everything. Early studies showed mechanical thrombectomy could help patients with big blockages. This led to more research on using endovascular therapy for M2 occlusions too.
Development of Endovascular Techniques and Devices
New tools and methods in endovascular therapy have been key in improving stroke care. Stent retrievers and other devices have made it easier to clear blockages. Better catheters have made procedures safer and more effective.
Device technology keeps getting better, allowing for treatment of smaller, harder-to-reach blockages like M2 occlusions. This means more patients can now get help through endovascular therapy.
Transition from Large Vessel to Medium Vessel Applications
At first, endovascular therapy was mainly for big blockages. But, as tools and methods got better, we started treating medium blockages, like M2 occlusions. The ESCAPE-MeVO trial showed it works well for these cases too.
Using endovascular therapy for medium blockages is a big step forward. It means more patients can get better care. As we keep improving and learning, we expect to help even more people.
Patient Selection for M2 Occlusion Endovascular Treatment
Choosing the right patients for endovascular therapy for M2 vessel occlusions is key. It’s all about clinical and imaging criteria. This ensures the best treatment for each patient, with the highest benefits and lowest risks.
Clinical Criteria for Intervention
Clinical criteria are vital in deciding who gets endovascular treatment. Severity of symptoms and timing of presentation are major factors. Those with severe symptoms and quick action are often chosen for treatment.
We look at how severe the symptoms are and how long ago the stroke happened. Patients within 6 to 24 hours might get endovascular therapy, based on other factors.
Imaging Selection Parameters
Imaging is essential in picking patients for endovascular treatment of M2 occlusions. Advanced neuroimaging techniques like CT perfusion and MRI show how much brain is at risk. This helps decide who can benefit from treatment.
We use imaging to see how much brain is damaged and how much can be saved. Those with a lot of brain that can be saved are good candidates for treatment.
Contraindications and Limitations
Endovascular therapy has its limits. Certain conditions, like big infarct cores or hemorrhage, make it not suitable. Also, some vascular anatomies or high risk for complications are not ideal.
It’s important to weigh these factors carefully. We assess everything to make sure treatment is right for each patient. This way, we avoid risks and tailor treatment to each person’s needs.
Technical Aspects of Endovascular Therapy for M2 Occlusions
Endovascular therapy for M2 occlusions needs careful planning and execution. We will look at the key technical elements that help these procedures succeed.
Access Techniques and Catheter Selection
Choosing the right access and catheter is vital for M2 occlusion treatment. Radial or femoral access depends on the patient’s body and the doctor’s choice. The right catheters and guidewires are also key to safely navigating the brain’s blood vessels.
We use a guide catheter and a microcatheter together to reach the M2 segment. The guide catheter keeps things stable, while the microcatheter helps us get to the small vessels.
Thrombectomy Approaches for Distal Vessels
Thrombectomy methods for M2 occlusions have improved a lot. The method chosen depends on the blockage, the blood vessel, and the doctor’s skill.
- Stent retriever thrombectomy is often used for M2 occlusions, with a high success rate.
- Aspiration thrombectomy works well for small blockages or when stent retrievers are hard to use.
- Combined techniques use stent retrievers and aspiration catheters together for better results.
Adjunctive Therapies and Medications
Supporting treatments and medicines are important for M2 occlusion care. Antiplatelet therapy is started during or after the procedure to stop new blockages.
Anticoagulation therapy is used in some cases to lower the risk of blood clots. The type and amount of medicine given depends on the patient’s needs and situation.
By focusing on these technical details, we can make endovascular therapy for M2 occlusions more effective. This helps improve patient care.
Evidence from Clinical Trials on M2 Occlusion Treatment
Recent studies have made big strides in understanding how to treat M2 occlusions. These trials have shown that endovascular therapy is both effective and safe for treating M2 occlusions.
ESCAPE-MeVO Trial Results and Implications
The ESCAPE-MeVO trial was a major study on treating M2 occlusions with endovascular therapy. It found that this therapy greatly improved patient outcomes compared to just medical treatment.
Key findings from the ESCAPE-MeVO trial include:
- Improved functional outcomes at 90 days
- Higher rates of successful reperfusion
- No significant increase in adverse events
These results are very important. They suggest that endovascular therapy is a good option for patients with M2 occlusions.
DISTAL Trial Findings
The DISTAL trial added more evidence for using endovascular therapy for M2 occlusions. It focused on how well modern thrombectomy devices worked.
Trial | Primary Outcome | Key Findings |
DISTAL | Functional independence at 90 days | Significant improvement in functional outcomes with endovascular therapy |
ESCAPE-MeVO | Functional independence at 90 days | Improved outcomes with endovascular therapy |
DISCOUNT Trial and Other Recent Evidence
The DISCOUNT trial and other recent studies have added to the evidence for endovascular therapy in M2 occlusions. These studies have shown that endovascular treatment is beneficial for certain patients.
The evidence from these trials is very important. It shows that endovascular therapy is a valuable option for treating M2 occlusions.
In conclusion, the latest clinical trials, including ESCAPE-MeVO, DISTAL, and DISCOUNT, support using endovascular therapy for M2 occlusions. These findings will likely change how doctors treat patients with acute ischemic stroke caused by M2 occlusions.
Complications and Management Challenges
Endovascular interventions for M2 occlusions face unique challenges. These include procedural complications that need careful management. Endovascular therapy is key for treating acute ischemic stroke caused by M2 occlusions. It’s vital to understand and manage its complications to improve patient outcomes.
Procedural Complications Specific to M2 Interventions
Procedural complications during endovascular therapy for M2 occlusions are significant. These include vessel perforation, dissection, and thromboembolism to other territories. The smaller size and more distal location of M2 vessels increase the risk of these complications. We must carefully navigate these challenges to ensure the best possible outcomes.
The risk of vessel perforation is concerning due to the risk of severe hemorrhage. Using softer and more navigable catheters and wires can help. Meticulous pre-procedural planning and imaging assessment are also key in identifying risks and planning the approach.
Post-Procedure Management
Effective post-procedure management is critical in minimizing complications and ensuring a good clinical outcome. This includes close monitoring in a neuro-intensive care unit. Here, neurological status can be frequently assessed, and any changes can be quickly addressed.
Post-procedure imaging, such as non-contrast CT or MRI, is essential to assess for any procedural complications. Antiplatelet therapy and anticoagulation strategies are also important. They help prevent re-occlusion and manage the risk of bleeding.
Strategies to Minimize Complications
To minimize complications during endovascular therapy for M2 occlusions, several strategies can be employed. First, careful patient selection is key. This includes considering the patient’s overall health, the specific anatomy of the occlusion, and any contraindications to endovascular therapy.
Second, operator experience is vital. Procedures should be performed by experienced neuro-interventionalists. Continuous education and training in the latest endovascular techniques are essential for maintaining a high level of proficiency.
- Utilize advanced imaging techniques for better procedural planning.
- Employ the latest generation thrombectomy devices designed for distal occlusions.
- Maintain a multidisciplinary team approach for a more complete care.
By understanding the complications and implementing strategies to minimize them, we can improve the outcomes of endovascular therapy for M2 occlusions. This provides the best possible care for our patients.
Clinical Outcomes and Prognostic Factors
Clinical results after treating M2 vessel occlusions with endovascular methods depend on several factors. Knowing these factors is key to better patient care and results.
Functional Outcomes After Endovascular Treatment
Results for patients treated with endovascular therapy for M2 occlusions can differ a lot. The patient’s age, how severe the blockage is, and how quickly they get treated are all important.
Table: Factors Influencing Functional Outcomes
Factor | Description | Impact on Outcome |
Age | Patient’s age at the time of treatment | Older patients tend to have poorer outcomes |
Occlusion Severity | Degree of vessel occlusion | More severe occlusions are associated with worse outcomes |
Time to Treatment | Time elapsed between stroke onset and treatment | Earlier treatment is associated with better outcomes |
Predictors of Good Clinical Response
Finding out who will do well with endovascular therapy is important. We look at the patient’s starting health, any other health issues, and how well blood can flow around the blockage.
Long-term Follow-up Considerations
Keeping up with patients over time is vital. It helps us see how well the treatment worked and handle any problems that come up. Regular check-ups and rehab help patients get better.
By learning more about the outcomes and factors for M2 occlusions treated with endovascular therapy, we can make our treatments better. This leads to better care for our patients.
Conclusion: Future Directions in M2 Occlusion Management
Endovascular therapy has changed how we treat M2 occlusions in acute ischemic stroke. It brings new hope to patients. We need to look at the current evidence and think about what’s next in managing M2 occlusions.
New research and better endovascular therapy will help us more. We’ll see better results for patients. New technologies and methods will make treatments more precise and effective.
We should keep working on improving M2 occlusion management. This means finding better ways to treat patients and care for them. By doing this, endovascular therapy will keep being a key part of treating acute ischemic stroke.
The future of M2 occlusion management will be shaped by new findings and medical technology. This will help us treat M2 occlusions more effectively.
FAQ
What is endovascular therapy for M2 vessel occlusions?
Endovascular therapy is a minimally invasive treatment. It uses catheters and devices to remove blockages in the M2 segment of the middle cerebral artery. This restores blood flow to the brain’s affected areas.
What are M2 occlusions, and why are they significant?
M2 occlusions block the M2 segment of the middle cerebral artery. This artery supplies blood to a large part of the brain. These occlusions can cause severe damage and are a challenge in treating strokes.
How are M2 occlusions diagnosed?
Diagnosing M2 occlusions involves several steps. First, doctors assess symptoms using stroke scales. Then, they use CT and MRI scans and angiography to plan treatment.
What is the role of endovascular therapy in treating M2 occlusions?
Endovascular therapy has changed how we treat strokes, including M2 occlusions. It provides a quick and effective way to restore blood flow and reduce damage.
What are the clinical criteria for selecting patients for endovascular treatment of M2 occlusions?
Doctors consider several factors to decide if a patient needs endovascular treatment. These include the severity of symptoms, how quickly the patient is treated, and imaging results.
What are the technical aspects of endovascular therapy for M2 occlusions?
The technical aspects involve careful planning and execution. This includes choosing the right access techniques and catheters. Doctors also use thrombectomy and other therapies to support the procedure.
What do recent clinical trials say about the effectiveness of endovascular therapy for M2 occlusions?
Recent trials like ESCAPE-MeVO, DISTAL, and DISCOUNT have shown endovascular therapy’s effectiveness. They provide evidence for its role in treating M2 occlusions.
What are the possible complications of endovascular therapy for M2 occlusions?
Complications can occur during M2 interventions. It’s important to have strategies for managing these complications to ensure the best outcomes for patients.
What are the prognostic factors for clinical outcomes after endovascular treatment of M2 occlusions?
Several factors influence outcomes after treatment. These include the severity of symptoms, the extent of damage, and the presence of collateral circulation.
What is the significance of long-term follow-up for patients treated with endovascular therapy for M2 occlusions?
Long-term follow-up is vital. It helps monitor outcomes, manage complications, and provide ongoing care to improve recovery and quality of life.
What is the future direction of M2 occlusion management?
The future involves ongoing research and innovation. This includes improving endovascular techniques, devices, and therapies. It also means optimizing patient selection and post-procedure care.
What is a distal occlusion?
A distal occlusion is a blockage in a distant or peripheral blood vessel. This can include the M2 segment of the middle cerebral artery and can cause ischemic damage.
What is an occlusion stroke?
An occlusion stroke happens when a brain blood vessel is blocked. This leads to ischemic damage and can cause severe neurological problems. It requires quick and effective treatment.
What is medium vessel occlusion?
Medium vessel occlusion is when blood vessels of intermediate size, like the M2 segment of the middle cerebral artery, are blocked. This can cause significant ischemic damage.
References
National Center for Biotechnology Information. Endovascular Therapy for M2 Vessel Occlusion in Acute Stroke. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC7015199/