Cranial nerve deficits can significantly impact daily life. They cause facial weakness, vision changes, and loss of sensation. These conditions affect thousands of people every year. At Liv Hospital, our team offers expert care and understanding. Learn the 7 alarming signs of cranial nerve deficits. Our critical guide explores the causes, from stroke to tumors, and your treatment options.
We aim to give a detailed look at cranial neuropathy. We’ll cover its causes, symptoms, and treatment options. Our goal is to help and support those affected by these conditions.
Key Takeaways
- Understanding cranial nerve disease and its impact on patients
- Recognizing the symptoms of neuropathy in the head
- Exploring the causes of cranial nerve deficits
- Discovering treatment options for cranial neuropathy
- The importance of prompt diagnosis and treatment
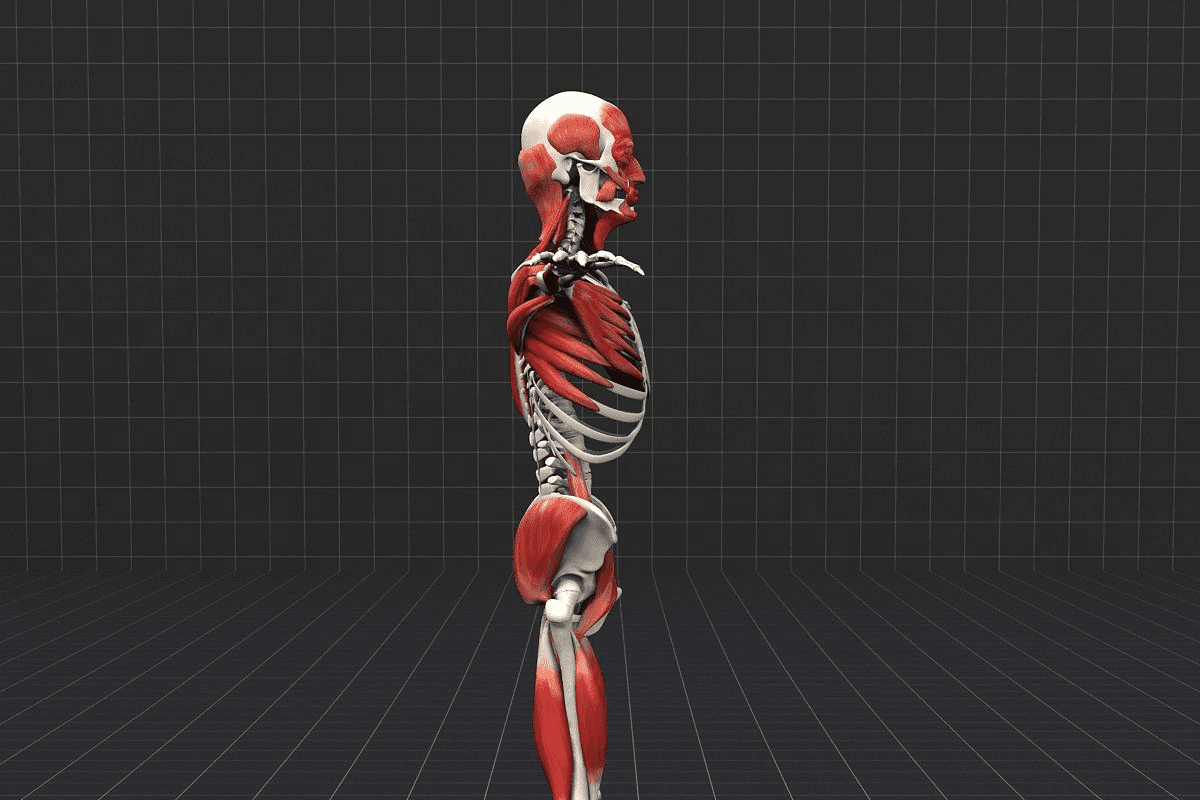
The Anatomy and Function of Cranial Nerves

Cranial nerves link the brain to the rest of the body. They help with many bodily functions like movement and sensation. Knowing about cranial nerves is key for diagnosing and treating cranial nerve disorders and cranial neuropathies.
The 12 Cranial Nerves and Their Roles
The human body has 12 cranial nerves. Each plays a vital role in controlling bodily functions. For example, the olfactory nerve (I) handles smell, and the optic nerve (II) deals with vision.
The facial nerve (VII) is special. It carries both sensory and motor fibers. This makes it important for facial expressions and more.
Here’s a list of the 12 cranial nerves and their roles:
- Olfactory nerve (I): smell
- Optic nerve (II): vision
- Oculomotor nerve (III): eye movement
- Trochlear nerve (IV): eye movement
- Trigeminal nerve (V): facial sensation and motor functions
- Abducens nerve (VI): eye movement
- Facial nerve (VII): facial expressions, taste, and other functions
- Vestibulocochlear nerve (VIII): hearing and balance
- Glossopharyngeal nerve (IX): swallowing and taste
- Vagus nerve (X): various autonomic functions
- Spinal accessory nerve (XI): neck and shoulder movements
- Hypoglossal nerve (XII): tongue movements
How Cranial Nerves Connect the Brain to the Body
Cranial nerves connect the brain to different parts of the body. They allow for the exchange of information and help with many processes. For instance, the trigeminal nerve (V) sends sensation to the face and controls some motor functions, like chewing.
It’s important to understand how cranial nerves connect the brain to the body. This knowledge helps in diagnosing and treating cranial nerves diseases and brain neuropathy. Healthcare professionals can better manage these conditions by knowing the roles of these nerves.
Understanding Cranial Nerve Deficits
It’s important for both doctors and patients to know about cranial nerve deficits. These deficits happen when the twelve cranial nerves don’t work right. These nerves control many things like movement, feeling, and how organs work.
Definition and Classification
Cranial nerve deficits mean any problem with the cranial nerves. These problems can be based on which nerve is affected, the type of problem, and why it’s happening.
Knowing how to classify these deficits is key for treating them. For example, cranial nerve palsy means a nerve is paralyzed or weak. On the other hand, cranial nerve neuropathy is a wider term for nerve damage.
Prevalence and Demographics
Cranial nerve deficits are common, with different rates for each condition. For instance, facial nerve palsy happens to 15-40 out of 100,000 people each year. It’s more common in older adults than in kids.
Knowing who gets cranial nerve deficits helps doctors plan better care. This knowledge helps them diagnose and treat more effectively.
We know that cranial nerve disorders can really affect someone’s life. By understanding what they are, how they’re classified, how common they are, and who they affect, we can help more people.
7 Common Types of Cranial Nerve Deficits
It’s important to know about different cranial nerve deficits for accurate diagnosis and treatment. These deficits can greatly affect a person’s life, impacting facial expressions, eye movements, and sensory perceptions.
Facial Nerve Palsy (Bell’s Palsy)
Facial Nerve Palsy, also known as Bell’s Palsy, causes sudden weakness or paralysis of facial muscles. It usually affects one side of the face. This happens because of damage to the seventh cranial nerve, which controls facial expressions.
The symptoms of Bell’s Palsy can vary. They may include:
- Rapid onset of facial weakness or paralysis
- Difficulty closing the eye on the affected side
- Drooping of the mouth or difficulty smiling
- Changes in taste or hearing
Trigeminal Neuralgia
Trigeminal Neuralgia is a chronic pain condition affecting the trigeminal nerve. This nerve is responsible for face sensation and motor functions like chewing. It causes intense, shock-like pain in the face.
Characteristics | Description |
Pain Episodes | Brief, intense pain attacks triggered by facial movements |
Affected Areas | Typically one side of the face, involving the cheek, lips, or gums |
Triggers | Light touch, eating, talking, or even a gentle breeze |
Oculomotor Nerve Palsy
Oculomotor Nerve Palsy affects the third cranial nerve. This nerve controls most eye movements, pupil constriction, and keeps the eyelid open. Damage to this nerve can cause eye movement problems, drooping eyelids, and double vision.
The causes of Oculomotor Nerve Palsy vary. They can include:
- Diabetes
- Trauma
- Aneurysms
- Tumors
Trochlear and Abducens Nerve Palsies
The trochlear and abducens nerves are the fourth and sixth cranial nerves. They are important for eye movements. Palsies of these nerves can cause double vision because the eyes can’t align properly.
Trochlear nerve palsy affects the superior oblique muscle. This muscle rotates the eye downward and outward. Abducens nerve palsy impacts the lateral rectus muscle, which is responsible for outward eye movement.
Comparison of Oculomotor, Trochlear, and Abducens Nerve Palsies:
Nerve | Function | Palsy Symptoms |
Oculomotor (III) | Most eye movements, pupil constriction, eyelid opening | Ptosis, limited eye movement, dilated pupil |
Trochlear (IV) | Superior oblique muscle (downward and outward eye movement) | Vertical diplopia, head tilt |
Abducens (VI) | Lateral rectus muscle (outward eye movement) | Horizontal diplopia, limited outward eye movement |
Recognizing Symptoms of Cranial Nerve Deficits
It’s important to know the signs of cranial nerve deficits for proper care. These deficits can show up in different ways, depending on the nerve. We’ll look at common symptoms grouped by type.
Facial Symptoms and Sensory Changes
Facial symptoms often show up when the facial nerve is affected. These can include:
- Facial drooping or weakness
- Difficulty closing the eye
- Altered taste sensation
- Numbness or tingling in the face
These symptoms can really affect a person’s life. For example, trouble closing the eye can cause dryness and eye infections.
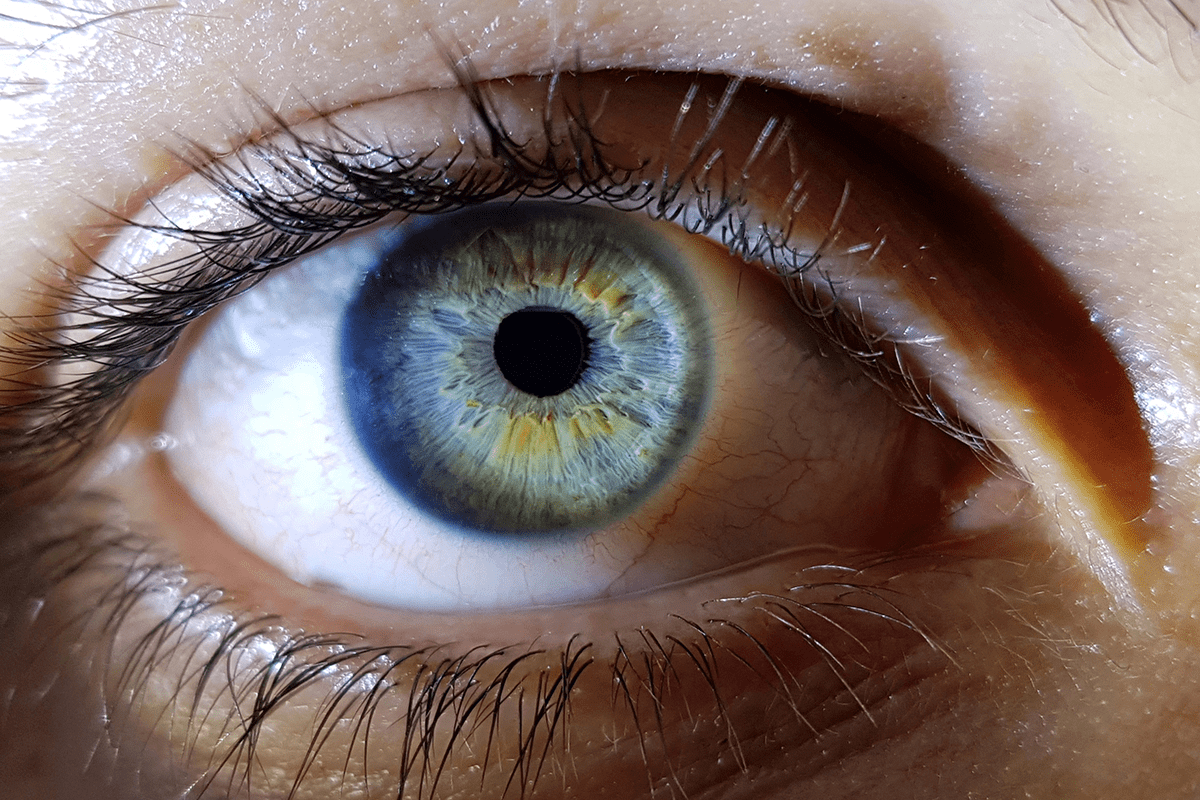
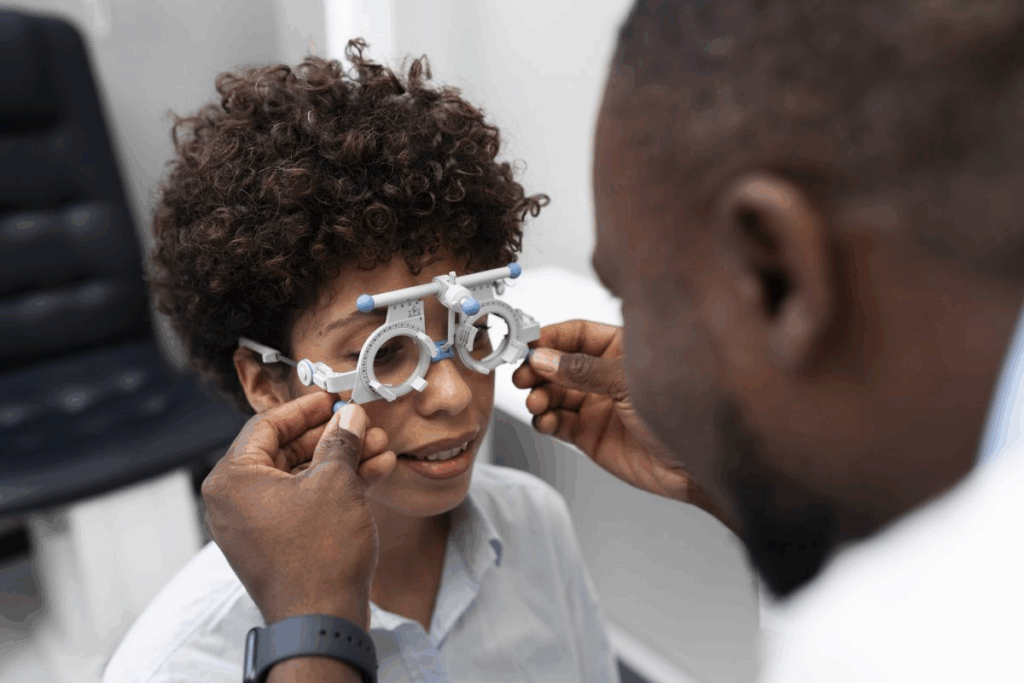
Visual and Ocular Disturbances
Visual problems are another big issue with cranial nerve deficits. Symptoms can include:
- Double vision (diplopia)
- Difficulty moving the eyes
- Pupil dilation or constriction
- Drooping eyelids (ptosis)
These eye issues come from problems with nerves like the oculomotor, trochlear, or abducens.
Swallowing and Speech Difficulties
Cranial nerve deficits can also mess with swallowing and speech. Symptoms may include:
- Difficulty swallowing (dysphagia)
- Slurred speech (dysarthria)
- Changes in voice quality
These problems usually come from issues with the glossopharyngeal and vagus nerves. These nerves are key for swallowing and speaking.
Hearing and Balance Problems
Problems with hearing and balance can also happen due to cranial nerve deficits. These often affect the vestibulocochlear nerve. Symptoms can include:
- Hearing loss or tinnitus
- Vertigo or dizziness
- Balance disturbances
These symptoms can really mess up a person’s day-to-day life. They can make it hard to talk and stay balanced.
In summary, the symptoms of cranial nerve deficits are varied and can affect many areas of health. Spotting these symptoms early is key for getting the right medical help.
Underlying Causes and Risk Factors
Cranial nerve deficits can come from vascular conditions, injuries, and infections. Knowing these causes helps doctors diagnose and treat these disorders well.
Vascular Conditions
Vascular issues are a big reason for cranial nerve problems. Stroke and cerebral vasculitis can damage nerves by affecting blood flow. This leads to nerve dysfunction.
Diabetes is also a risk factor for cranial nerve issues, like cranial neuropathies. Diabetes-related inflammation and blood vessel damage can harm nerve function.
Traumatic Injuries
Traumatic brain injuries (TBI) often cause cranial nerve problems. The injury’s force can damage the nerves’ delicate structures. This results in various symptoms based on the nerves affected.
Car accidents, falls, and sports injuries can lead to TBI and nerve damage. It’s important to get medical help quickly after a head injury.
Infections and Inflammatory Disorders
Infections and inflammatory disorders can also cause cranial nerve issues. Conditions like meningitis and encephalitis can inflame and damage nerves.
Lyme disease and sarcoidosis are systemic infections and disorders that can harm nerve function. Early treatment is key to avoiding permanent nerve damage.
Tumors and Space-Occupying Lesions
Tumors, whether benign or malignant, can press on or invade cranial nerves, causing deficits. Acoustic neuromas and meningiomas are tumors that can affect nerve function.
These lesions can cause symptoms like hearing loss, facial weakness, and vision problems. This depends on where they are and which nerves they affect.
Diagnostic Approaches for Cranial Nerve Deficits
Healthcare providers use several methods to diagnose cranial nerve deficits. These include clinical assessment, imaging, and electrophysiological studies. This approach helps us find the cause of nerve problems and plan treatment.
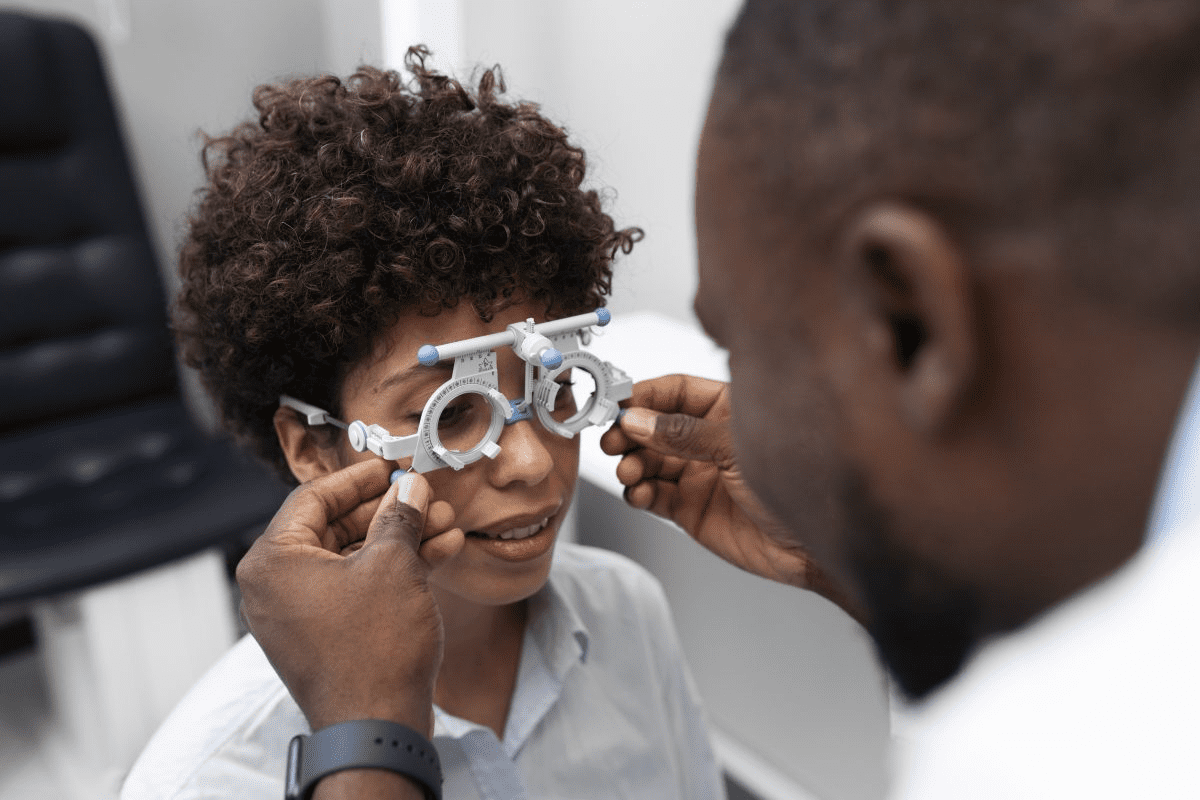
Clinical Examination Techniques
A detailed clinical exam is key to diagnosing cranial nerve disorders. We check how well cranial nerves work using different methods. These include:
- Cranial nerve palpation and percussion
- Checking muscle strength and reflexes
- Testing sensory functions like pain and vibration
- Looking at eye movements and pupil responses
Imaging Studies
Imaging is vital for diagnosing cranial nerve issues. We use:
- Magnetic Resonance Imaging (MRI): to see cranial nerves and find problems
- Computed Tomography (CT) scans: to spot bone or blood vessel issues
- Angiography: to check blood vessels for problems
These tools help us understand nerve problems and plan treatment.
Laboratory Tests
Laboratory tests are key when we think a systemic condition might be involved. We might do:
- Blood tests for infections or metabolic issues
- Cerebrospinal fluid analysis for conditions like multiple sclerosis
These tests give us clues about nerve problems and help decide treatment.
Electrophysiological Studies
Electrophysiological studies, like EMG and NCS, are important for checking nerve function. They help us:
- Look at muscle electrical activity
- Check nerve speed and find damage
By using these methods together, we can accurately diagnose and treat cranial nerve deficits.
Treatment Options for Cranial Nerve Deficits
Dealing with cranial nerve deficits needs a wide range of treatments. The right treatment depends on the cause, how bad the deficit is, and the patient’s health. We’ll look at the different ways to treat cranial nerve deficits, their good points, and their limits.
Medical Management
Medical treatment is often the first step for cranial nerve deficits. It usually involves corticosteroids to lessen swelling around the nerve. For example, corticosteroids help with Bell’s palsy if used quickly. Doctors may also give medicines for pain, dizziness, or seizures.
Surgical Interventions
Surgery is needed sometimes to fix nerve problems. Microvascular decompression is a surgery for trigeminal neuralgia to ease nerve pressure. Other surgeries might include nerve grafting or repair.
Physical and Occupational Therapy
Physical and occupational therapy are key for recovery. They help with facial movements, swallowing, and more. Each patient gets a special exercise plan to help them get better and live better.
Alternative and Complementary Approaches
Some people find help in alternative and complementary therapies. Acupuncture is one example. It’s important for patients to talk to their doctors about these options to make sure they’re safe and right for them.
Prevention Strategies
To prevent cranial nerve deficits, it’s important to know their causes. By understanding these causes, we can lower the risk of related problems. This helps keep our nerves healthy.
Managing Underlying Health Conditions
Managing health conditions is key to preventing cranial nerve deficits. Diabetes and hypertension can harm our nerves. Working with doctors to control these conditions is vital.
Staying on top of treatments and making healthy lifestyle choices helps. Eating well and exercising regularly are important. They help manage health issues and keep nerves strong.
Lifestyle Modifications
Making lifestyle changes is also important. A healthy lifestyle can lower the risk of nerve problems. Avoiding smoking, drinking less alcohol, and staying active are good steps.
Eating foods full of nutrients is also beneficial. Foods with antioxidants, vitamins, and minerals protect nerves. Getting advice from nutritionists or doctors on diet plans is helpful.
Protective Measures for Head Injuries
Head injuries can cause nerve problems. So, it’s important to protect our heads. Wearing helmets and making homes safer can help prevent injuries.
- Use helmets during cycling, motorcycling, or contact sports.
- Install safety gates at the top of stairs.
- Ensure proper lighting in living areas.
By taking these steps, we can lower the risk of nerve problems from head injuries. Knowing the risks of certain activities and taking precautions is also important.
Living with Cranial Nerve Deficits
For those with cranial nerve deficits, finding ways to cope and getting support is essential. Coping with the challenges of these disorders needs a mix of medical care, lifestyle changes, and emotional support.
Coping Strategies
It’s important to find ways to manage symptoms of cranial nerve deficits. This includes physical therapy to boost strength and mobility, speech therapy for communication issues, and counseling for emotional support.
Learning to relax is also helpful. Techniques like meditation and deep breathing exercises can reduce stress and anxiety.
Support Resources and Communities
Access to support groups and resources is key for those with cranial nerve deficits. These groups offer a place to share experiences, get advice, and find emotional support from others who understand.
Organizations focused on neurological disorders also provide valuable help. They offer educational materials, advocacy, and connections to specialists in cranial nerve conditions.
Long-term Outlook and Prognosis
The future outlook for those with cranial nerve deficits depends on the cause and extent of nerve damage. Some conditions may improve with treatment, while others need ongoing care.
Knowing the prognosis and working with healthcare providers is important. It helps plan for the future and make informed care decisions. Staying updated on the latest research and treatments is also key.
By using effective coping strategies, getting support, and understanding their future, people with cranial nerve deficits can live fulfilling lives despite their challenges.
Conclusion
Understanding cranial nerve deficits is key for early diagnosis and treatment. This improves patient outcomes. We’ve looked at the anatomy and function of cranial nerves, the types of deficits, and their causes.
A cranial neuropathy overview shows these conditions can greatly affect a person’s life. They can cause facial weakness, visual problems, and swallowing issues. It’s important to recognize these symptoms and get medical help quickly.
In conclusion, managing health conditions and making lifestyle changes are vital. Protecting ourselves from head injuries also helps prevent cranial nerve issues. This way, we can lower the risk of these conditions and keep our cranial nerves healthy.
Our summary on cranial nerve issues stresses the need for awareness and education. Knowing the causes, symptoms, and treatment options helps healthcare providers and patients work together. This leads to better outcomes.
FAQ
What are cranial nerve deficits?
Cranial nerve deficits happen when the 12 cranial nerves don’t work right. This can cause problems like facial weakness, vision issues, and trouble swallowing.
What causes cranial nerve palsies?
Many things can cause cranial nerve palsies. These include blood vessel problems, injuries, infections, and tumors. Knowing the cause helps find the right treatment.
What are the symptoms of cranial neuropathy?
Symptoms of cranial neuropathy vary. They can include facial pain, numbness, or weakness. You might also see vision problems, double vision, or have trouble swallowing or speaking.
How are cranial nerve deficits diagnosed?
Doctors use several methods to diagnose cranial nerve deficits. They include clinical exams, imaging, lab tests, and electrophysiological studies. These tools help find the cause of the problem.
What are the treatment options for cranial nerve disorders?
Treatment for cranial nerve disorders depends on the cause. It might include medicine, surgery, therapy, or other methods. A team approach is often best.
Can cranial nerve deficits be prevented?
Some cranial nerve deficits can’t be prevented. But, managing health, making lifestyle changes, and avoiding head injuries can help lower the risk.
How do cranial nerve deficits affect quality of life?
Cranial nerve deficits can really affect daily life. They can make simple tasks hard, impact social life, and affect mood. Support and resources can help manage these challenges.
What is the prognosis for individuals with cranial nerve deficits?
The outlook for cranial nerve deficits varies. It depends on the cause, how severe it is, and the treatment’s success. With the right care, many people see big improvements.
Are there any support resources available for individuals with cranial nerve deficits?
Yes, there are many resources for those with cranial nerve deficits. You can find online forums, support groups, and organizations that offer help and information.
What is cranial neuritis?
Cranial neuritis is when a cranial nerve gets inflamed. This can cause pain, numbness, or weakness. It can be caused by infections, autoimmune issues, or trauma.
How do diseases of the cranial nerves affect the brain?
Diseases of the cranial nerves can harm the brain. They disrupt nerve function, leading to symptoms. Untreated, they can cause lasting damage.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4481793/