Cranial nerve disorders affect the 12 pairs of nerves that connect the brain to the head, neck, and trunk. These conditions need special care to fix problems and make life better. Our essential guide to 7 alarming cranial nerve disorders. Learn the critical symptoms, causes, and treatments for these conditions.
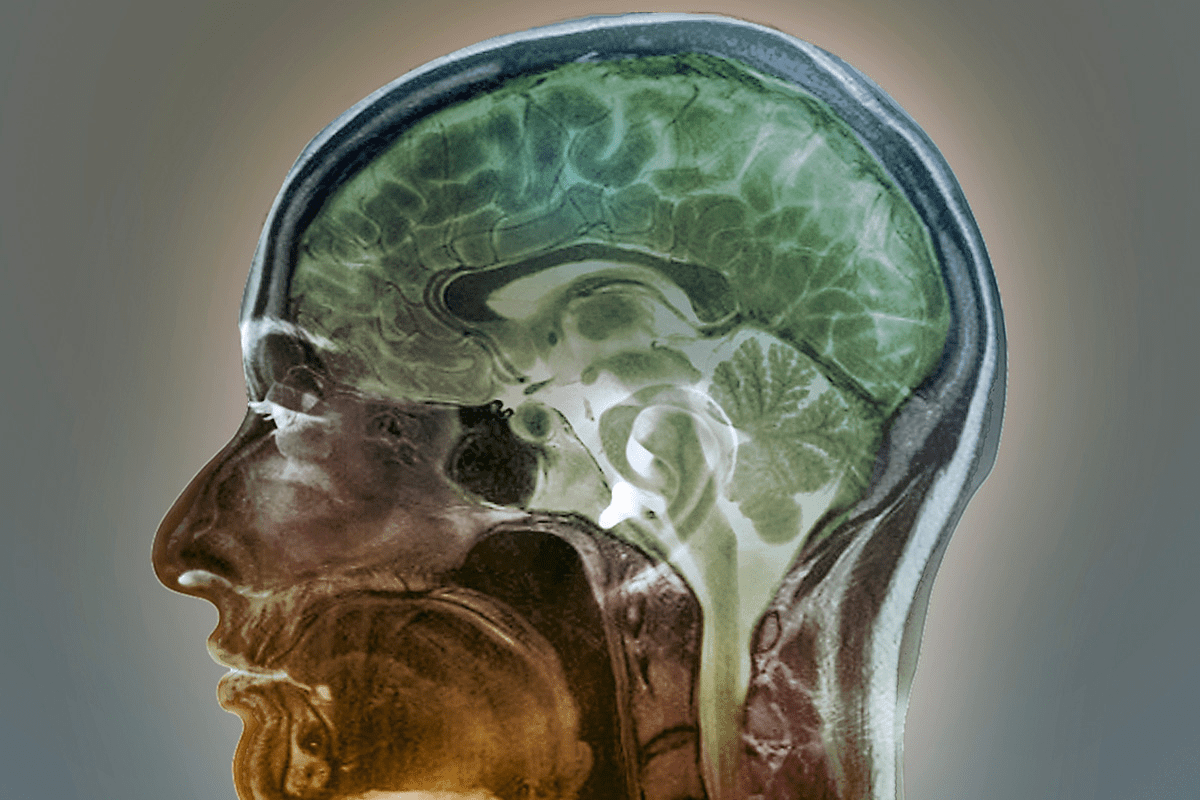
The cranial nerves start in the brain stem. Problems with them mean there’s something wrong in the brain stem or along the nerve path. At Liv Hospital, our team uses top-notch imaging, proven treatments, and new surgery methods to help patients.
Key Takeaways
- Understanding cranial nerve disorders is key for good treatment.
- These issues affect the 12 pairs of nerves from the brain to the body.
- Special care is needed to fix problems and improve life quality.
- Liv Hospital offers advanced imaging and new surgery techniques.
- A team approach ensures patients get the best care.
The Anatomy and Function of Cranial Nerves
Learning about cranial nerves is key to diagnosing and treating health issues. These nerves control many body functions, like movement and feeling. There are 12 pairs, each with its own job.
The 12 Pairs of Cranial Nerves and Their Roles
The 12 pairs of cranial nerves are named with Roman numerals (I-XII). They are named based on their functions or structures. Here’s a list of them:
- Olfactory Nerve (I): It sends information about smells to the brain.
- Optic Nerve (II): It carries visual information from the eyes to the brain.
- Oculomotor Nerve (III): It controls most eye movements and how the pupils work.
- Trochlear Nerve (IV): It helps rotate the eye.
- Trigeminal Nerve (V): It handles facial sensations and chewing.
- Abducens Nerve (VI): It helps move the eye outward.
- Facial Nerve (VII): It controls facial expressions, taste, and some movements.
- Vestibulocochlear Nerve (VIII): It’s involved in hearing and balance.
- Glossopharyngeal Nerve (IX): It has fibers for taste and swallowing.
- Vagus Nerve (X): It handles swallowing, speaking, and controls the body’s internal organs.
- Accessory Nerve (XI): It provides motor control to neck and shoulder muscles.
- Hypoglossal Nerve (XII): It controls tongue movements.
As stated by
“The cranial nerves are a complex system that requires precise understanding for effective diagnosis and treatment of related disorders.”
How Cranial Nerves Connect the Brain to Body Systems
Cranial nerves link the brain to different body systems. They help us do many things, from feeling sensations to moving our bodies. For example, the trigeminal nerve is key for facial feelings. The vagus nerve helps with heart rate and other autonomic functions.
Knowing how cranial nerves connect the brain to the body is vital. It helps in diagnosing and treating cranial nerve deficits or neuropathy in the head. Healthcare experts can better help patients with cranial nerve problems by understanding these nerves’ roles.
Understanding Common Cranial Nerve Disorders

Cranial nerve disorders affect nerves that connect the brain to other parts of the body. They can be caused by inflammation, infections, vascular issues, trauma, tumors, and neurodegenerative diseases.
Inflammatory, Infectious, and Vascular Causes
Conditions like meningitis and encephalitis can damage cranial nerves. Vascular problems, such as strokes or aneurysms, can also harm these nerves. This can lead to disorders like third nerve palsy.
Bell’s palsy, a facial paralysis, is often caused by inflammation of the seventh cranial nerve. Knowing the causes helps in finding the right treatment.
Traumatic, Tumoral, and Neurodegenerative Etiologies
Trauma can directly damage cranial nerves. Tumors, whether benign or malignant, can compress these nerves. Neurodegenerative diseases like Alzheimer’s or Parkinson’s can also impact nerve function.
For example, acoustic neuromas, which affect the eighth cranial nerve, can cause hearing loss and balance problems. Understanding these causes is key to diagnosing and managing these disorders.
General Symptoms and Warning Signs
Symptoms of cranial nerve disorders vary widely. They can include pain, weakness, numbness, or paralysis in different areas. Visual problems, hearing loss, and issues with speech or swallowing are common too.
Recognizing these symptoms early is vital for effective treatment. Knowing the symptoms and their causes can greatly improve treatment outcomes.
Cause | Common Disorders | Typical Symptoms |
Inflammatory/Infectious | Bell’s Palsy, Meningitis | Facial paralysis, headache |
Vascular | Third Nerve Palsy, Stroke | Eye movement issues, ptosis |
Traumatic | Traumatic neuropathy | Numbness, weakness |
Tumoral | Acoustic Neuroma | Hearing loss, balance issues |
Neurodegenerative | Parkinson’s Disease | Tremors, rigidity |
Bell’s Palsy: Seventh Cranial Nerve Disorder
Bell’s palsy affects the seventh cranial nerve, causing sudden facial weakness. It’s a common reason for facial paralysis. We’ll look into its symptoms, causes, and treatments.
Facial Weakness and Asymmetry Symptoms
The main sign of Bell’s palsy is facial weakness or paralysis on one side. This can cause facial asymmetry. It makes smiling, closing the eye, or controlling facial expressions hard. Other symptoms include:
- Drooling
- Difficulty eating or drinking
- Changes in tear production or saliva
- Numbness or pain around the jaw or behind the ear
Viral Causes and Risk Factors
Bell’s palsy is often caused by viral infections, like the herpes simplex virus. Other risk factors include:
Risk Factor | Description |
Family History | Having a family history of Bell’s palsy may increase the risk. |
Viral Infections | Certain viral infections can trigger Bell’s palsy. |
Diabetes | People with diabetes are at a higher risk of developing Bell’s palsy. |
Treatment Options and Recovery Timeline
Treatment for Bell’s palsy includes corticosteroids and antiviral medications. Sometimes, physical therapy is suggested to strengthen facial muscles. Most people recover fully within a few months.
It’s important to understand Bell’s palsy for both patients and doctors. Early recognition and treatment can greatly improve outcomes.
Trigeminal Neuralgia: Fifth Cranial Nerve Pain
Trigeminal neuralgia is a disorder of the fifth cranial nerve. It causes severe, shock-like or stabbing pain in the face. The trigeminal nerve controls sensation in the face and helps with chewing.
Characteristics of Trigeminal Pain Attacks
The pain from trigeminal neuralgia is intense and can be very debilitating. It usually happens on one side of the face. Simple actions like brushing teeth or chewing can trigger it. The pain attacks can last from a few seconds to several minutes.
Key characteristics of trigeminal neuralgia pain include:
- Sudden, severe, shock-like or stabbing pain
- Pain typically on one side of the face
- Triggered by everyday activities or light touch
- Duration of pain can vary from seconds to minutes
Blood Vessel Compression and Other Causes
The exact cause of trigeminal neuralgia often involves a blood vessel compressing the nerve. This compression can damage the nerve’s protective covering, causing pain. Other causes include tumors, multiple sclerosis, or nerve injury.
Understanding the cause is key to finding the right treatment.
Medication, Procedures, and Surgical Interventions
Treatment for trigeminal neuralgia starts with medication to manage pain. Anticonvulsants are often used because they can help reduce or stop the pain. If medication doesn’t work, procedures like percutaneous rhizotomy or stereotactic radiosurgery might be considered. Sometimes, surgery is needed to relieve pressure on the nerve.
Treatment options include:
- Medications such as anticonvulsants
- Percutaneous rhizotomy to damage the pain-causing nerve fibers
- Stereotactic radiosurgery to target the trigeminal nerve root
- Surgical decompression to relieve pressure on the nerve
Living with trigeminal neuralgia can be tough. Our team is dedicated to providing full care and support to manage this condition well.
Microvascular Cranial Nerve Palsy
Cranial nerve palsies caused by microvascular issues are a big worry for people with diabetes and high blood pressure. This condition affects the nerves in the head, often linked to diabetes and high blood pressure.
Impact on Cranial Nerves 3, 4, and 6
Mostly, cranial nerves 3, 4, and 6 are affected by microvascular cranial nerve palsy. These nerves control eye movements. The third nerve helps move the eye, open the eyelid, and narrow the pupil. The fourth nerve also helps with eye movement. The sixth nerve is key for moving the eye outward.
“These nerve problems can cause double vision, eyelids that droop, and trouble moving the eyes,” says Medical Expert, a neurologist. “It’s important to know how these nerves work to diagnose and treat microvascular cranial nerve palsy.”
Relationship to Diabetes and Hypertension
Diabetes and high blood pressure are closely linked to microvascular cranial nerve palsy. These conditions harm the small blood vessels that feed the nerves, causing them to malfunction. “Keeping diabetes and high blood pressure under control is key to avoiding this condition,” says Medical Expert, an endocrinologist. “Managing blood sugar and blood pressure well can greatly lower the risk of getting this condition.”
- Diabetes harms blood vessels with high blood sugar.
- Hypertension strains blood vessels, making them more prone to damage.
- Regularly checking and managing these conditions is vital for prevention.
Diagnostic Approach and Management Strategies
Diagnosing microvascular cranial nerve palsy requires a detailed neurological check, imaging tests, and looking at underlying health issues. Treatment aims to fix the root causes, like managing diabetes and high blood pressure, and easing symptoms.
Treatment options may include:
- Medicines to control diabetes and high blood pressure.
- Eye patches or prism glasses to fix double vision.
- Physical therapy to boost eye movement.
By knowing the causes and using the right treatments, we can manage microvascular cranial nerve palsy well. This helps improve patient outcomes.
Acoustic Neuroma: Vestibular Schwannoma
Acoustic neuroma, also known as vestibular schwannoma, is a benign tumor. It affects the eighth cranial nerve. This nerve is key for sound and balance information from the inner ear to the brain. We will look at symptoms, development, and treatment options for this condition.
Eighth Cranial Nerve Symptoms and Progression
The symptoms of acoustic neuroma vary based on the tumor’s size and location. Common symptoms include:
- Hearing loss or distortion on one side
- Tinnitus (ringing in the ears)
- Balance problems or dizziness
- Facial numbness or weakness
As the tumor grows, it can press on nearby nerves. This leads to more symptoms. It’s important to seek medical attention if you notice any of these symptoms.
Tumor Development and Growth Patterns
Acoustic neuromas are slow-growing tumors. They start from Schwann cells around the vestibular nerve, part of the eighth cranial nerve. The exact cause is not fully understood, but they’re linked to genetic conditions like neurofibromatosis type 2.
The growth pattern of acoustic neuromas varies. Some tumors stay small and don’t cause symptoms. Others grow large and cause significant symptoms.
Treatment Options from Observation to Surgery
The treatment for acoustic neuroma depends on the tumor’s size, growth rate, and the patient’s health. Treatment options include:
Treatment Option | Description | Applicability |
Observation | Regular monitoring with MRI scans to track tumor growth. | Small, asymptomatic tumors |
Radiation Therapy | High-precision radiation to stop tumor growth. | Small to medium-sized tumors |
Surgery | Surgical removal of the tumor. | Large tumors or those causing significant symptoms |
Each treatment option has its benefits and risks. We work closely with patients to find the best treatment plan. This is based on their individual needs and preferences.
Glossopharyngeal Neuralgia: Ninth Nerve Disorder
Glossopharyngeal neuralgia is a rare condition that affects the ninth cranial nerve. It causes severe pain episodes. These pains are sharp and stabbing, mainly in the throat and ear.
Throat and Ear Pain Characteristics
The pain from glossopharyngeal neuralgia is very severe. It can start from simple actions like swallowing or talking. The pain usually hits one side of the throat or ear, feeling like stabbing or electric shocks.
Distinguishing from Other Pain Syndromes
It’s hard to diagnose glossopharyngeal neuralgia because it looks like other pain syndromes. A detailed check-up and patient history are key to tell it apart. We look at where the pain is and what triggers it to make a correct diagnosis.
Pharmacological and Surgical Treatment Approaches
First, doctors try medicines like anticonvulsants to lessen pain. If meds don’t work, surgery might be needed. Options include microvascular decompression or rhizotomy. We’ll dive into these treatments to understand how to manage glossopharyngeal neuralgia.
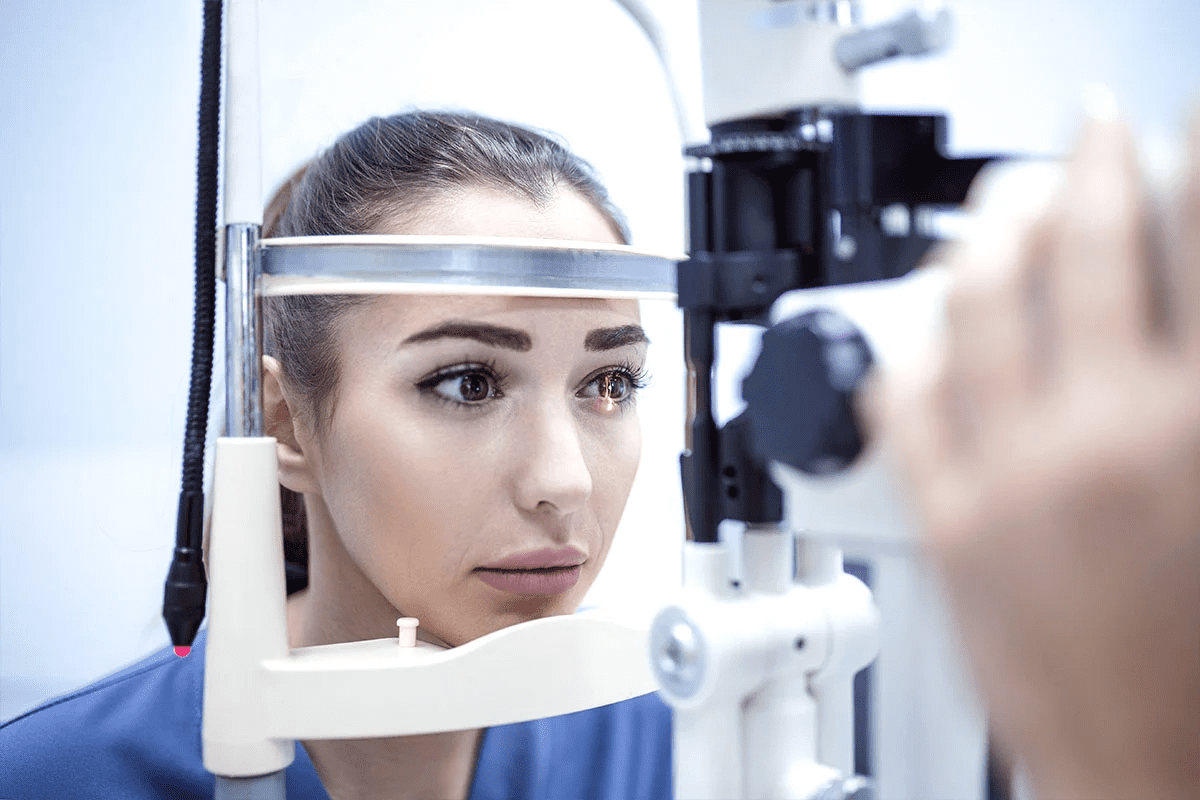
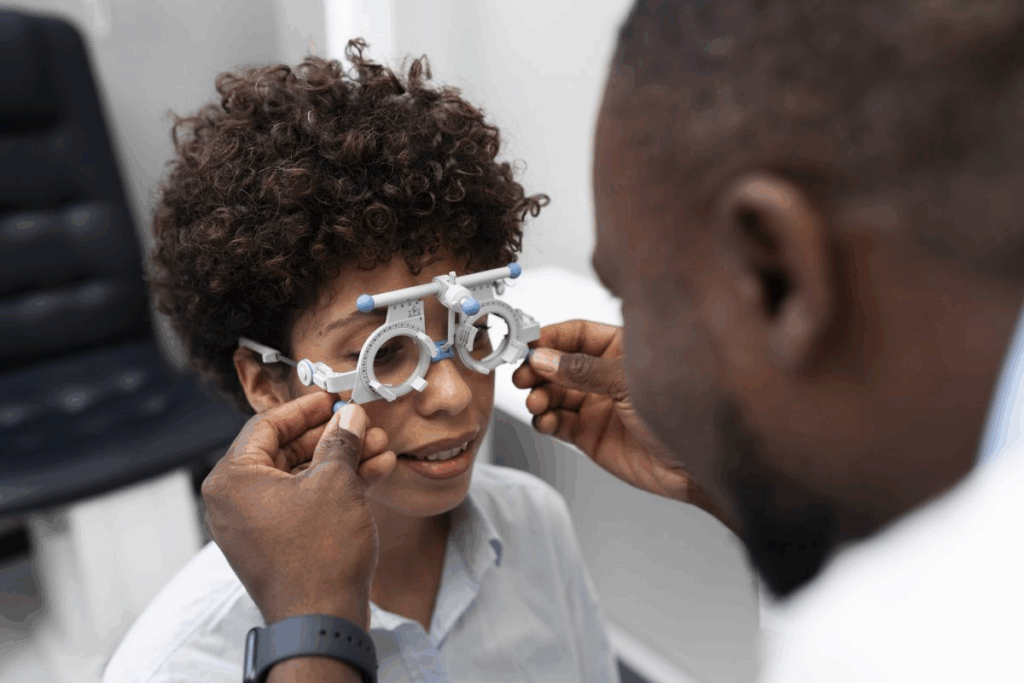
Optic Neuritis: Second Cranial Nerve Inflammation
Optic neuritis is an inflammation of the optic nerve. It can cause various visual symptoms and complications. This condition affects the second cranial nerve, which is key for sending visual information from the eye to the brain.
It causes inflammation of the optic nerve, leading to pain and temporary vision loss in one eye. Symptoms can include blurred vision, loss of color vision, and pain when moving the eye. The severity of these symptoms can range from mild to severe, affecting daily life and quality of life.
Visual Symptoms and Associated Conditions
The visual symptoms of optic neuritis can be alarming and disrupt daily life. Common symptoms include:
- Blurred vision or loss of visual acuity
- Impaired color vision
- Pain on eye movement
- Temporary vision loss
These symptoms can be linked to other conditions, making a thorough diagnosis important. It’s essential to seek medical attention if you experience sudden vision changes.
Relationship to Multiple Sclerosis
Optic neuritis is often linked to multiple sclerosis (MS), a chronic condition affecting the central nervous system. Studies show that those with optic neuritis are at a higher risk of developing MS. The presence of lesions on MRI scans can indicate a higher risk of MS in patients with optic neuritis.
“The relationship between optic neuritis and multiple sclerosis is significant, with a considerable proportion of patients with optic neuritis eventually developing MS.”
– A medical study on the link between optic neuritis and MS
Steroid Treatment and Visual Prognosis
Treatment for optic neuritis usually involves corticosteroids to reduce inflammation. Intravenous steroid treatment can accelerate visual recovery, though the long-term visual outcome may not be significantly different.
The visual prognosis for most patients with optic neuritis is generally good. Many see significant improvement within a few months. Yet, some may have persistent visual disturbances.
Hypoglossal Nerve Disorder: Twelfth Cranial Nerve Dysfunction
Hypoglossal nerve disorder affects the twelfth cranial nerve. It causes trouble with tongue movement and coordination. This nerve is key for tongue control, important for speech, eating, and swallowing.
Tongue Movement Abnormalities and Speech Issues
The hypoglossal nerve controls tongue muscles. Its dysfunction can cause weakness, paralysis, or abnormal movements of the tongue. These issues can make speaking, swallowing, and eating hard.
One sign of this disorder is tongue deviation. The tongue moves to one side when pushed out. This happens because the tongue’s affected side is weaker, pulling it towards the lesion.
Causes from Stroke to Motor Neuron Disease
Hypoglossal nerve disorder can come from stroke, trauma, tumors, and neurodegenerative diseases like ALS. Stroke is a common cause, damaging the nerve or its brain pathways. Head or neck trauma can also harm the nerve.
It can also be linked to other neurological conditions or an underlying disease. For example, ALS can weaken the tongue over time, causing severe weakness and atrophy.
Diagnostic Workup and Management Options
Diagnosing hypoglossal nerve disorder involves a detailed neurological exam. This includes checking tongue movements and strength. Imaging like MRI or CT scans might be used to find causes like tumors or vascular lesions.
Managing hypoglossal nerve disorder depends on the cause. If it’s due to a treatable condition, like a tumor, surgical intervention or other treatments might help. For irreversible damage, speech therapy and rehabilitation can improve function and help adapt to changes.
Dealing with hypoglossal nerve disorder is tough. Our team is dedicated to providing full care and support to manage this condition well.
Conclusion: Advances in Cranial Nerve Disorder Treatment
We’ve looked at different cranial nerve disorders, their signs, reasons, and how to treat them. New ways to treat these disorders have made a big difference. Research keeps going, helping us understand and manage these conditions better.
Treatment for cranial nerve disorders is getting better, focusing on better care and results. With new treatments, patients can handle their symptoms better and live a better life. Our knowledge and treatment of these disorders will keep growing, helping those affected more.
The future for treating cranial nerve disorders is bright, with ongoing research and new therapies. By learning more and finding new ways to treat, we can support patients with these disorders more effectively.
FAQ
What are cranial nerve disorders?
Cranial nerve disorders affect the 12 pairs of cranial nerves. These nerves control movement, sensation, and organ function.
What are the common causes of cranial nerve disorders?
Causes include inflammation, infections, and vascular issues. Also, trauma, tumors, and neurodegenerative diseases like diabetes and hypertension.
What are the symptoms of cranial nerve disorders?
Symptoms vary by nerve. They can include pain, numbness, and weakness. Also, vision loss, hearing loss, and speech or swallowing issues.
What is Bell’s palsy, and how is it treated?
Bell’s palsy affects the seventh cranial nerve. It causes facial weakness and asymmetry. Treatment includes corticosteroids and antiviral medications. Physical therapy helps improve facial function.
What is trigeminal neuralgia, and how is it managed?
Trigeminal neuralgia affects the fifth cranial nerve. It causes intense pain attacks. Treatment includes medications and surgical interventions like microvascular decompression.
What is microvascular cranial nerve palsy, and how is it related to diabetes and hypertension?
It affects the third, fourth, and sixth cranial nerves. Often caused by diabetes and hypertension. Management includes controlling blood sugar and blood pressure and addressing symptoms.
What is acoustic neuroma, and how is it treated?
Acoustic neuroma is a tumor on the eighth cranial nerve. It causes hearing loss, tinnitus, and balance problems. Treatment ranges from observation to surgery, based on the tumor’s size and growth.
What is glossopharyngeal neuralgia, and how is it managed?
Glossopharyngeal neuralgia affects the ninth cranial nerve. It causes throat and ear pain. Treatment includes pain relievers and anticonvulsants, as well as surgery.
What is optic neuritis, and how is it related to multiple sclerosis?
Optic neuritis affects the second cranial nerve. It causes vision loss and pain. It’s often linked to multiple sclerosis. Treatment includes corticosteroids to reduce inflammation and improve vision.
What is hypoglossal nerve disorder, and how is it diagnosed?
Hypoglossal nerve disorder affects the twelfth cranial nerve. It causes tongue movement issues and speech problems. Diagnosis involves examination, imaging, and electromyography to find the cause.
What are the advances in cranial nerve disorder treatment?
Advances include better diagnostic tools and new treatments. These include gene therapy and stem cell therapy. They offer hope for patients with these conditions.
What is cranial neuropathy?
Cranial neuropathy is damage or dysfunction of cranial nerves. It can cause pain, numbness, weakness, and vision or hearing loss.
What are the symptoms of cranial nerve palsies?
Symptoms vary by nerve. They can include double vision, drooping eyelids, facial weakness, and speech or swallowing issues.
Reference:
National Center for Biotechnology Information. Cranial Nerve Disorders: Symptoms, Causes, and Treatment. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6462363/)