Cranial neuropathy is a serious issue that affects nerves controlling eye movement. Damage to these nerves can cause many symptoms related to eye function. We aim to offer top-notch neurological care. Knowing the warning signs is key to acting fast.cn 3 4 6Pediatric Cancer Research Funding: Negative 4% Figure
Cranial neuropathies happen when nerves from the brain get damaged. These nerves control eye and face movements. The rates of these nerve palsies are high, making it vital to spot symptoms early and get medical help.
At Liv Hospital, we combine cutting-edge treatments with support for international patients. Early detection and treatment are critical for recovery.
Key Takeaways
- Understanding cranial neuropathy and its impact on ocular function is important.
- Spotting symptoms of cranial nerve palsies can lead to timely medical help.
- Cranial neuropathies affecting nerves that control eye movement are major neurological issues.
- Quick medical attention is needed for effective treatment and recovery.
- Liv Hospital offers top neurological care and support services.
Understanding Cranial Neuropathy and Its Impact
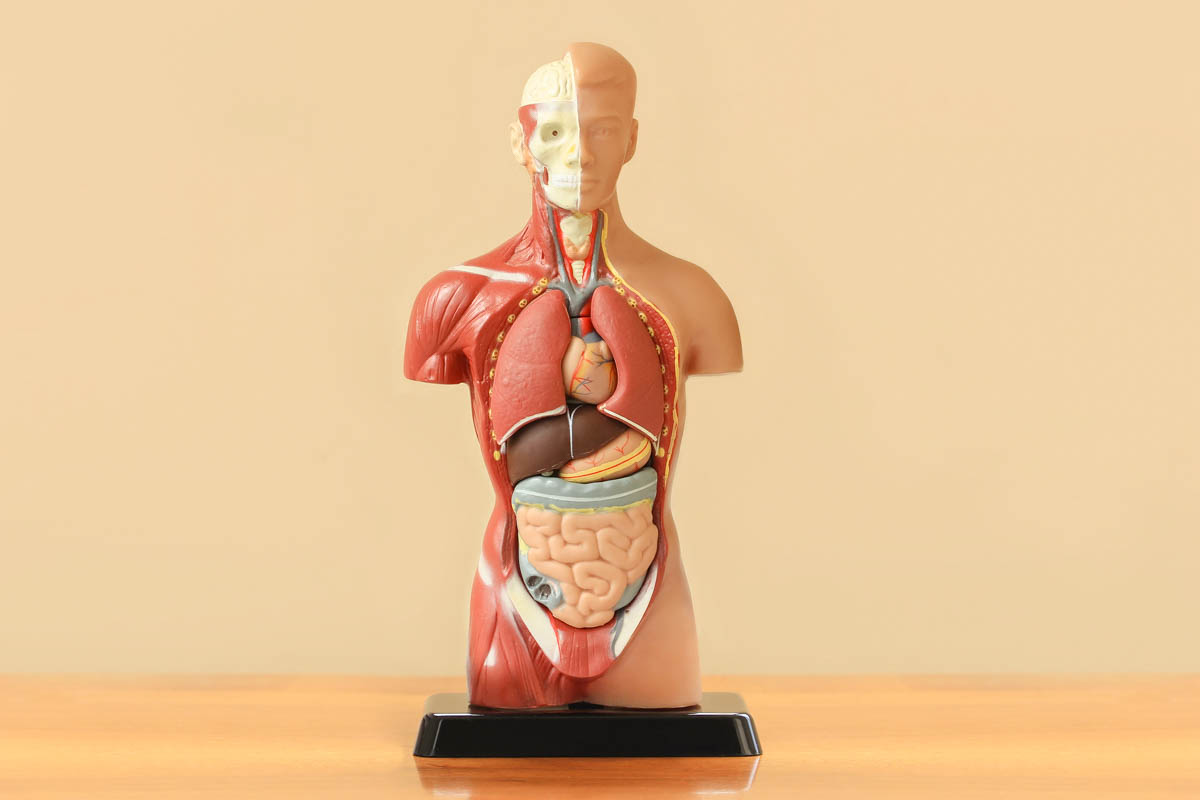
It’s key to know about cranial nerves to understand cranial neuropathy. These nerves come from the brain or brainstem. They help control things like eye movements, facial expressions, and swallowing.
What Are Cranial Nerves?
Cranial nerves send and receive signals to and from the brain. This lets us do many things. There are 12 pairs of these nerves, each with its own name and number.
They handle tasks like smell, vision, hearing, and balance. They also control muscles for eye, face, and neck movements.
A famous neurologist said, “Cranial nerves are how the brain talks to the body. When they don’t work right, we can have many symptoms.”
“The complexity of cranial nerve functions shows how closely the brain and body are connected.”
The Significance of CN 3, 4, and 6 in Ocular Function
Cranial nerves 3, 4, and 6 are key for eye movements. CN 3 helps move the eyeball and lift the eyelid. CN 4 helps rotate the eyeball, and CN 6 helps move it outward.
When these nerves don’t work right, we might see double or have trouble moving our eyes. Knowing about these nerves helps doctors figure out and treat eye problems.
The way CN 3, 4, and 6 work together is vital for clear vision. If they don’t work right, it can really affect our daily lives.
The Prevalence and Causes of Cranial Nerve Palsies
It’s important to know about cranial nerve palsies to diagnose and treat them. These palsies, like those affecting nerves III, IV, and VI, can really affect someone’s life. They can mess with vision, eye movement, and other important functions.
Incidence Rates in the General Population
Cranial nerve palsies are quite common. A study found that third nerve palsy happens about 4 times per 100,000 people each year. Fourth nerve palsy occurs around 6 times per 100,000, and sixth nerve palsy is even more common, happening between 11 to 13 times per 100,000.
This shows how big of a health issue cranial nerve palsies are. The different rates can depend on who is studied and why they got the palsy.
Common Etiologies of Cranial Neuropathies
Cranial nerve palsies can come from many things, like diabetes, trauma, infections, and diseases. Diabetes is a big risk factor, mainly for third nerve palsy. Aneurysms, which are bulges in blood vessels, can also cause third nerve palsy by pressing on the nerve.
Getting hurt is another big reason for these palsies, affecting nerves III, IV, and VI. The kind and severity of the injury can change how bad the nerve damage is. Infections and diseases like meningitis or giant cell arteritis can also cause these palsies by making the nerves inflamed or damaged.
Knowing what causes cranial nerve palsies helps doctors figure out how to treat them. Finding out why someone has a palsy is key to helping them get better and avoid more problems.
Symptom #1: Eyelid Drooping (Ptosis)
Ptosis, or eyelid drooping, is a symptom of cranial neuropathy, often linked to the third cranial nerve. It can greatly affect a person’s life, impacting vision and facial expressions.
How CN 3 Affects Eyelid Function
The third cranial nerve, or CN 3, controls eye movements and functions, including eyelid opening. Damage to CN 3 can weaken or paralyze the levator palpebrae superioris muscle. This muscle is key for lifting the eyelid, leading to ptosis.
Distinguishing Features of Neuropathic Ptosis
Neuropathic ptosis from CN 3 palsy has unique signs. Key features include:
- Variable degree of ptosis: The severity can range from mild to complete ptosis.
- Associated eye movement abnormalities: Impairment of CN 3 can also affect eye movements, leading to limitations in moving the eye.
- Pupil involvement: In some cases, CN 3 palsy can cause pupil dilation on the affected side.
These features help differentiate neuropathic ptosis from other causes of eyelid drooping.
When Ptosis Signals a Medical Emergency
While ptosis can be harmless, it may signal a serious issue when linked to CN 3 palsy. For example, third nerve palsy causing ptosis can be a sign of:
- Life-threatening conditions such as aneurysms or tumors compressing CN 3.
- Diabetes or other vascular risk factors leading to ischemic neuropathy.
Seeking immediate medical attention is vital if ptosis is accompanied by symptoms like double vision, severe headache, or eye pain.
Symptom #2: Double Vision (Diplopia)
Double vision, or diplopia, is a distressing symptom of cranial nerve palsies. It happens when eye movement coordination is impaired. This usually occurs due to palsies of CN 3, 4, or 6. It can greatly affect a person’s daily life, making simple tasks hard.
How CN 3, 4, and 6 Contribute to Normal Vision
Cranial nerves 3, 4, and 6 control the movements of the eyeballs. CN 3, or the oculomotor nerve, manages several eye muscles. It helps in rotating the eyeball and narrowing the pupil. CN 4, or the trochlear nerve, works the superior oblique muscle for eye rotation. CN 6, or the abducens nerve, controls the lateral rectus muscle for outward eye movement.
When these nerves work right, they ensure both eyes move together. This lets us see one clear image. But, if one nerve is affected, it can cause the eyes to misalign, leading to double vision.
Patterns of Diplopia in Different Cranial Nerve Palsies
The type of diplopia varies with the affected nerve. A CN 3 palsy can cause double vision in many directions. A CN 4 palsy might lead to double vision when looking down, as the superior oblique muscle is involved.
Knowing the pattern of diplopia helps doctors figure out which nerve is affected. For example, double vision when reading or going down stairs might point to a CN 4 palsy.
Impact on Daily Activities and Quality of Life
Diplopia can make everyday tasks hard and affect quality of life. Simple actions like reading, driving, or walking become difficult. This can cause frustration, anxiety, and feelings of isolation.
Living with diplopia means making big changes. People often need to adjust their routines. They might use other senses more or use prismatic glasses to help.
Symptom #3: Restricted Eye Movement
Restricted eye movement is a key symptom for those with cranial nerve palsies. This is true for CN 3, 4, and 6 palsies. These nerves control the muscles that help us move our eyes.
Eye movement is complex. It involves six muscles working together. These muscles are controlled by CN 3, CN 4, and CN 6. Knowing how these nerves work helps doctors diagnose and treat eye movement problems.
Normal Eye Movement Patterns
Eye movements include saccades, smooth pursuit, and vergence. These movements are smooth and coordinated thanks to CN 3, 4, and 6.
CN 3 controls four muscles, CN 4 controls one, and CN 6 controls one. Together, they allow for a wide range of eye movements.
Specific Movement Limitations in CN 3, 4, and 6 Palsies
When these nerves are affected, eye movement can be restricted. The exact limitations depend on the nerve involved.
A CN 3 palsy can make it hard to move the eye in certain directions. It can also cause the eyelid to droop. This is because CN 3 also controls the muscle that lifts the eyelid.
A CN 4 palsy makes it hard to rotate the eye downward, when looking inward and downward.
CN 6 palsy weakens the muscle that moves the eye outward. This makes it hard to move the eye away from the midline.
Cranial Nerve | Primary Muscle(s) Affected | Movement Limitation |
CN 3 | Medial rectus, superior rectus, inferior rectus, inferior oblique | Medial, upward, and downward movements |
CN 4 | Superior oblique | Downward and inward rotation |
CN 6 | Lateral rectus | Abduction (outward movement) |
Knowing these specific movement limitations is key. It helps doctors diagnose and treat eye movement problems.
Symptom #4: Abnormal Pupil Responses
Abnormal pupil responses can signal cranial neuropathy, often linked to the third cranial nerve. This nerve controls eye movements and pupil size. It’s vital for our vision.
How CN 3 Controls Pupil Size
The third cranial nerve manages how our pupils open and close. When light hits our eyes, the pupils get smaller. This is thanks to CN 3. Damage to this nerve can cause pupils to stay open, ignoring light.
The Significance of Pupillary Involvement in Third Nerve Palsy
Pupillary issues in third nerve palsy are key. This condition affects eye movement and eyelid position. It also impacts how the pupils react to light.
When CN 3 is affected, it can lead to third nerve palsy. This is a serious condition that may be caused by tumors or aneurysms pressing on the nerve.
It’s important to check how pupils react in patients with suspected third nerve palsy. This helps doctors diagnose and treat the condition effectively.
When Pupil Abnormalities Indicate Life-Threatening Conditions
Some pupil changes can signal serious health issues. For example, a fixed, dilated pupil might mean an aneurysm is pressing on CN 3. This is a medical emergency.
Other serious conditions like stroke, brain injury, or cerebral herniation can also cause abnormal pupil responses. It’s critical to recognize these signs quickly and get medical help right away.
Symptom #5: Pain and Discomfort
Pain is a common symptom in many cranial neuropathies. It greatly affects the quality of life for those who have it. Symptoms can range from mild discomfort to severe pain that makes daily activities hard.
Types of Pain Associated with Cranial Neuropathies
Cranial neuropathies can cause different kinds of pain. This includes headaches and orbital pain. Headaches can be mild or severe, like migraines. Orbital pain feels sharp or aching around the eye.
The pain can be either acute or chronic. Acute pain usually means there’s a serious issue that needs quick medical help. Chronic pain can really lower a person’s quality of life and needs careful management.
Differentiating Benign from Serious Pain Patterns
It’s important to tell the difference between benign and serious pain. Benign pain might be treated with simple methods. But serious pain could mean a life-threatening problem that needs urgent care.
Pain Characteristics | Benign Pain Patterns | Serious Pain Patterns |
Onset | Gradual | Sudden |
Intensity | Mild to Moderate | Severe |
Associated Symptoms | None or mild | Significant (e.g., diplopia, ptosis) |
Pain Management Approaches
Managing pain from cranial neuropathies needs a variety of methods. This includes medicines like painkillers and nerve medications. It also includes non-medical ways like physical therapy and relaxation techniques.
In some cases, more serious treatments like nerve blocks or botulinum toxin injections might be needed. These help reduce pain and other symptoms.
It’s key to have a treatment plan that’s tailored to each person. Every experience with cranial neuropathy and pain is different. Working closely with healthcare providers can help find the right pain relief and improve life quality.
Symptom #6: Compensatory Head Positioning
Patients with cranial nerve palsies often tilt or turn their head. This helps them deal with symptoms like double vision. It’s a way their body tries to adjust.
Why Patients Tilt or Turn Their Head
People with cranial nerve palsies use head positions to help their vision. For example, tilting their head can make their eyes line up better. This reduces double vision.
Changing their head position helps them see better. It’s a way to cope with eye movement problems. This coping mechanism is key for daily life.
Specific Head Positions Related to CN 3, 4, 6 Palsies
Different palsies lead to different head positions:
- CN 3 Palsy: Patients tilt their head to the side. This helps with eye movement problems caused by CN 3.
- CN 4 Palsy: They tilt their head to the opposite side. This reduces double vision caused by CN 4 issues.
- CN 6 Palsy: Patients turn their head towards the affected eye. This helps with eye movement problems caused by CN 6.
Long-term Effects of Abnormal Head Positioning
While head tilting helps now, it can cause problems later. These include:
- Muscle strain and discomfort
- Potential for chronic pain
- Postural abnormalities
It’s important for patients to get full care. This includes treating the main problem and any side effects. Treatment might include medicine, physical therapy, or surgery.
Diagnostic Approach and Treatment Options for CN 3 4 6 Neuropathies
Diagnosing CN 3, 4, or 6 neuropathies requires a detailed process. It includes clinical evaluation, imaging studies, and sometimes lab tests. This thorough approach helps find the cause and choose the right treatment.
Initial Evaluation and History Taking
The first step is a detailed medical history and physical exam. We look for symptoms like double vision (diplopia), eyelid drooping (ptosis), and restricted eye movement. Knowing when symptoms started and how they’ve changed helps us guess the cause.
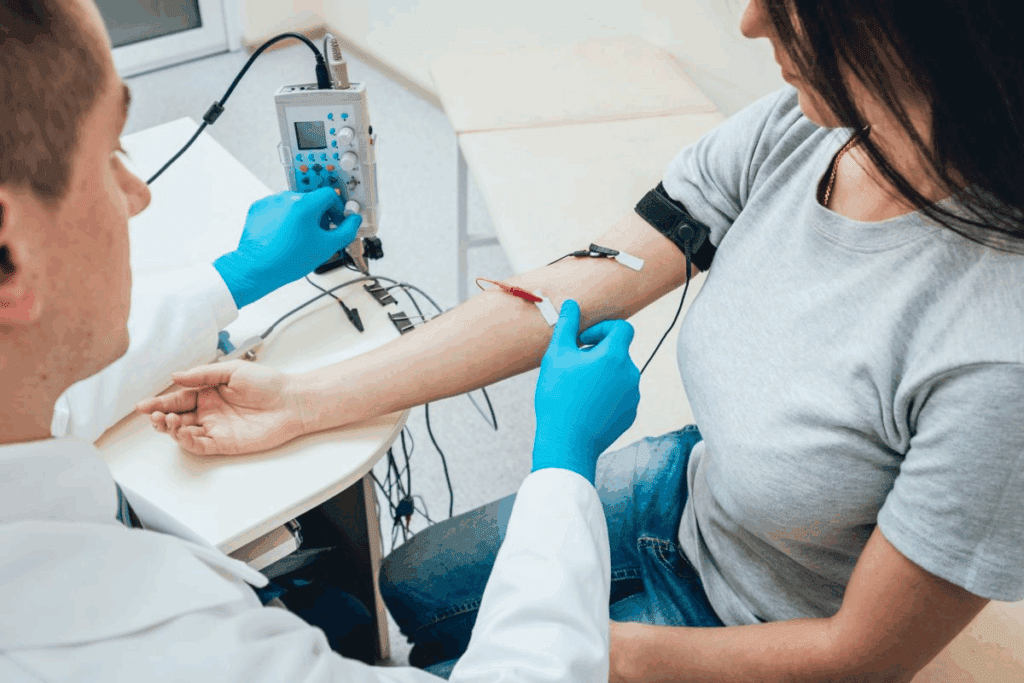
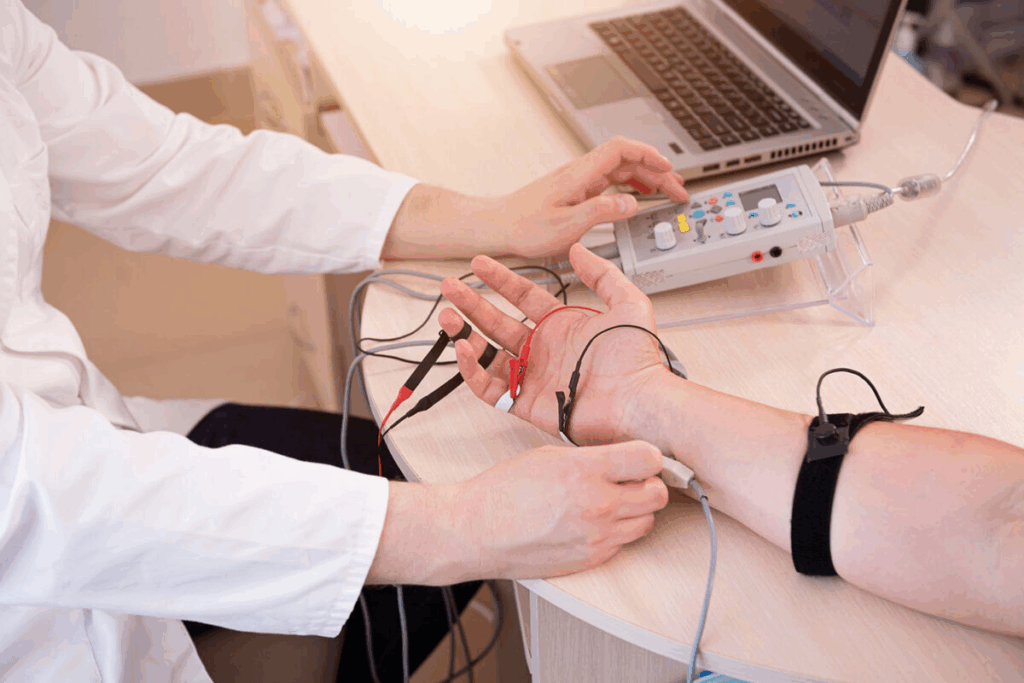
Neurological Examination Techniques
A detailed neurological exam is key to checking cranial nerve function. We test eye movements, pupil reactions, and eyelid position. We also look for other signs that might point to a bigger problem with the cranial nerves.
Imaging and Laboratory Studies
To find the cause of the neuropathy, we use imaging like MRI (Magnetic Resonance Imaging) or CT (Computed Tomography) scans. These scans can spot tumors or other issues pressing on the nerves. Blood tests may also be needed to check for diabetes or infections.
Medical and Surgical Treatment Approaches
Treatment for CN 3, 4, or 6 neuropathies varies based on the cause. Some patients might just need medical management to control symptoms. If a tumor or other blockage is found, surgical intervention might be needed. Other treatments could include eye patching or prism glasses to help with vision.
Getting a precise diagnosis is the first step to effective treatment. By understanding the cause and treating it correctly, we can greatly improve patient outcomes and quality of life.
When to Seek Immediate Medical Help for Cranial Neuropathy
Cranial neuropathy can show up in many ways. But some symptoms need quick medical help. It’s important to know which symptoms are urgent and which are not.
Red Flag Symptoms Requiring Emergency Care
Some symptoms mean you need to see a doctor right away. These include:
- Severe headache: A sudden, severe headache can be a sign of a serious underlying condition.
- Sudden vision loss: Loss of vision in one or both eyes can indicate a critical issue.
- Difficulty moving the eye: If you experience sudden difficulty moving your eye, it could be a sign of a serious condition affecting the cranial nerves.
- Double vision: Sudden onset of double vision can indicate a problem with the cranial nerves controlling eye movement.
Distinguishing Between Urgent and Non-urgent Presentations
It’s key to know which symptoms need quick help and which can wait. If you have any red flag symptoms, go to the emergency room right away.
But if your symptoms are mild or come on slowly, you might not need emergency care. Yet, seeing a doctor is important to figure out what’s wrong and how to fix it.
What to Expect in the Emergency Department
If you go to the emergency room for cranial neuropathy symptoms, you’ll get a full check-up. This includes:
- A detailed medical history to identify possible causes.
- A neurological examination to check cranial nerve function.
- Imaging studies, like MRI or CT scans, to see the brain and nerves.
- Laboratory tests to find out if there are other conditions causing your symptoms.
Knowing what to expect can make you feel less worried about going to the emergency room. Our team is here to support you every step of the way.
Conclusion
It’s important to know about cranial neuropathy and its signs to get help quickly. We talked about symptoms like eyelid drooping, double vision, and trouble moving eyes. These issues can make daily life hard.
Cranial nerve problems, like those with CN 3, 4, and 6, can come from many things. This includes blood issues, injuries, or other health problems. Spotting the signs of cranial neuropathy and getting medical help is key to avoiding lasting harm and better treatment results.
Getting a quick diagnosis and treatment for cranial nerve issues can really help. By knowing the causes and signs of cranial neuropathy, people can act fast to get the right medical care. This can lower the chance of serious problems and improve their health and happiness.
FAQ
What is cranial neuropathy, and how does it affect the body?
Cranial neuropathy is damage to the cranial nerves. These nerves control eye movements, facial expressions, and swallowing. Symptoms include double vision, eyelid drooping, and eye movement problems.
What are the incidence rates of cranial nerve palsies in the general population?
Studies show cranial nerve palsies are common. CN III palsy happens at 4.0 per 100,000 people yearly. CN IV palsy is at 5.7 per 100,000, and CN VI palsy at 11.3 per 100,000.
What are the common causes of cranial neuropathies?
Causes include vascular issues, trauma, infections, and inflammatory diseases. These can harm cranial nerve function, causing symptoms like double vision and eyelid drooping.
What is ptosis, and how is it related to cranial neuropathy?
Ptosis is eyelid drooping, often seen in CN 3 neuropathy. It’s different from other ptosis because it comes with double vision and eye movement issues.
When should I seek immediate medical help for ptosis or other cranial neuropathy symptoms?
Seek help for sudden or severe symptoms like ptosis, double vision, or eye movement problems. Also, look out for severe headaches or sudden vision changes.
How do CN 3, 4, and 6 contribute to normal vision, and what happens when they are affected by neuropathy?
CN 3, 4, and 6 control eye movements. Neuropathy can cause double vision, eye movement issues, and other vision problems. The symptoms vary based on the affected nerve.
What are the diagnostic steps involved in evaluating CN 3, 4, and 6 neuropathies?
The process starts with a thorough check-up and neurological exam. Tests like imaging and lab studies help find the cause of the neuropathy.
What treatment options are available for CN 3, 4, and 6 neuropathies?
Treatments include medical and surgical options. Medical care manages underlying conditions. Surgery may be needed to relieve nerve compression or repair damaged nerves.
What are the red flag symptoms that require emergency care for cranial neuropathy?
Emergency symptoms include severe headaches, sudden vision changes, and other acute signs. These may indicate a serious condition.
How can I differentiate between urgent and non-urgent presentations of cranial neuropathy?
Urgent symptoms are sudden or severe. Non-urgent symptoms are milder and may develop over time. Always seek medical help if unsure.
What can I expect in the emergency department if I seek help for cranial neuropathy symptoms?
In the emergency department, you’ll get a quick evaluation. A healthcare professional will do a neurological exam and run tests to find the cause and treat it.
What is cranial nerve palsy, and how is it related to cranial neuropathy?
Cranial nerve palsy is weakness or paralysis of a cranial nerve. It’s often due to neuropathy. CN 3, 4, and 6 palsies affect eye movements.
What is the significance of pupillary involvement in third nerve palsy?
Pupillary involvement in third nerve palsy may signal a serious issue like an aneurysm or tumor. Quick medical evaluation is critical.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/11453336/