Anterior disease includes many medical conditions that affect important body parts. These need quick diagnosis and expert care to avoid serious problems.
At Liv Hospital, we combine top medical skills with a focus on the patient. This ensures people get treatments backed by the latest research and guidelines.
Managing diseases like optic nerve disorder needs a clear guide. Our guide helps patients understand the steps for good care. It’s designed for those looking for top-notch medical help.
Key Takeaways
- Understanding the complexities of anterior disease and its impact on patients
- Liv Hospital’s commitment to delivering world-class healthcare with complete support
- The importance of evidence-based treatment guided by the latest academic protocols
- A step-by-step approach to managing anterior disease and related conditions
- Support for international patients seeking advanced medical treatments
Understanding the Spectrum of Anterior Disease
Anterior diseases cover a wide range of conditions affecting different parts of the body. It’s important to understand them well for effective management. These diseases can affect various structures, leading to different symptoms.
Definition and Classification of Anterior Pathologies
Anterior pathologies are diseases or injuries affecting the front parts of the body. Classification is key for diagnosis and treatment. For example, ACL injuries in the knee and eye disorders are common anterior pathologies.
Classifying these conditions helps doctors plan treatments. It’s based on where the problem is and what’s causing it. For example:
- ACL injuries are classified by how severe they are.
- Optic nerve problems are grouped by their cause, like inflammation or compression.
Epidemiology and Global Impact Statistics
The spread of anterior diseases varies by condition. Recent studies show they affect many people worldwide. For example, ACL surgeries are done on about 42.7 to 45.1 people per 100,000 each year.
Knowing how these diseases affect people globally is vital for healthcare planning. The impact can be huge, affecting quality of life, healthcare costs, and work productivity.
Exploring anterior diseases shows we need a detailed approach to tackle them. By understanding their definition, classification, and spread, we can improve care and outcomes for patients.
Recognizing Symptoms of Anterior Disease
Knowing the symptoms of anterior disease is the first step to getting the right treatment. Anterior diseases affect different parts of the body, like the eyes and muscles. The symptoms can vary, making it hard to diagnose. But, there are common signs and red flags that can help.
Common Clinical Presentations
Anterior diseases often show specific symptoms. For example, anterior uveitis, an eye inflammation, causes pain, redness, and blurred vision. LARS (Low Anterior Resection Syndrome) after surgery can lead to frequent bowel movements and pain.
These symptoms can really affect a person’s life. That’s why it’s important to know them early. This helps in getting the right treatment quickly.
Red Flags Requiring Immediate Attention
Some symptoms need immediate medical help. For eye issues like acute angle-closure glaucoma, look out for severe pain and vision loss. In heart problems like anterior myocardial infarction, chest pain and shortness of breath are urgent signs.
Knowing these red flags can save lives. It’s vital to seek help right away if you experience them.
Symptom Variation Across Different Anterior Conditions
How anterior disease shows up can differ a lot. For instance, knee injuries might cause pain and instability. Eye diseases can lead to vision problems.
Condition | Common Symptoms |
Anterior Uveitis | Pain, redness, photophobia, blurred vision |
LARS (Low Anterior Resection Syndrome) | Frequency or urgency of stools, fecal incontinence, rectal pain |
Anterior Cruciate Ligament Injury | Knee instability, pain, swelling |
It’s important to understand these differences. This helps in diagnosing and treating anterior diseases better. We aim to give care that meets each patient’s unique needs.
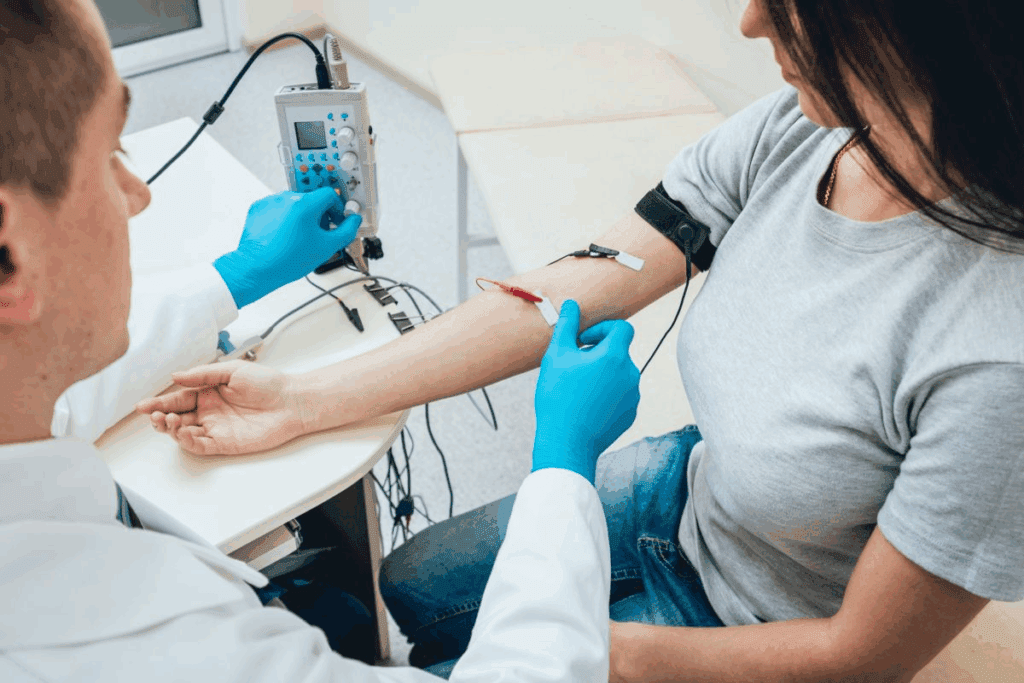
Essential Diagnostic Protocols for Anterior Disease
Diagnosing anterior disease requires a detailed approach. This includes initial checks, imaging, and special tests. We’ll cover the key steps doctors take to spot these diseases.
Initial Assessment Framework
The first step is vital in diagnosing anterior diseases. It starts with a detailed medical history and physical exam. This helps find symptoms and signs of disease in the front part of the eye.
Clinical evaluation is key. It helps doctors narrow down what might be wrong and decide on more tests.
For example, in suspected anterior uveitis, a slit lamp exam is used. It looks for signs of inflammation in the front part of the eye. For LARS after rectal cancer surgery, checking bowel function is important.
Imaging Techniques and Their Applications
Imaging is a big part of diagnosing anterior diseases. Ultrasound biomicroscopy (UBM) and anterior segment optical coherence tomography (AS-OCT) give detailed views of the front part of the eye. They help spot issues like uveitis and glaucoma.
These tools help see the angle of the anterior chamber, find tumors, and check for damage. For instance, AS-OCT is great for glaucoma, while UBM looks at the ciliary body and finds tumors.
Laboratory and Specialized Testing
Lab and special tests are key to confirming anterior disease diagnoses. For uveitis, tests look for inflammation and underlying causes like autoimmune disorders.
For LARS, tests like anorectal manometry and rectal compliance testing are used. They help understand how LARS affects bowel function and quality of life.
By using clinical checks, imaging, and lab tests together, doctors get a full picture of anterior diseases. They can then create treatment plans that fit each patient’s needs.
Step-by-Step Management of Anterior Cruciate Ligament Conditions
Managing ACL conditions requires a step-by-step plan. It starts with the acute phase, then moves to either conservative or surgical treatments. The final step is rehabilitation.
Acute Phase Management
The first step in managing ACL injuries is to reduce pain and swelling. It also involves restoring range of motion and strengthening the muscles around the knee. This phase is key in deciding the next steps in treatment.
- Immediate care involves the RICE principle: Rest, Ice, Compression, and Elevation.
- Pain management is achieved through a combination of medication and physical therapy modalities.
- Early mobilization helps in preventing stiffness and promoting healing.
Conservative Treatment Protocols
For some, conservative management is the best first step. This includes a structured rehabilitation program. It aims to improve knee function and stability.
Key components include:
- Physical therapy to strengthen the quadriceps and hamstring muscles.
- Neuromuscular training to enhance knee stability.
- Activity modification to avoid high-risk activities.
Surgical Intervention Decision-Making
If conservative management fails or is not suitable, surgery may be needed. The decision to have surgery depends on several factors. These include the patient’s age, activity level, and the presence of other knee injuries.
Surgical options include ACL reconstruction and ACL repair. ACL reconstruction involves grafting a new ligament. ACL repair is less common.
Rehabilitation Progression Timeline
Rehabilitation after ACL surgery or injury is a gradual process. It can last several months. It’s important for restoring knee function and safely returning to sports or activities.
- The initial phase focuses on pain reduction and regaining range of motion.
- The strengthening phase involves progressive resistance exercises.
- The final phase includes functional training and sports-specific drills.
Critical Care Pathway for Anterior Myocardial Infarction
A quick and effective care pathway is key for treating anterior myocardial infarction. We stress the need for fast action to better patient outcomes.
10-Minute Response Protocol
When a patient is diagnosed with anterior myocardial infarction, we start a 10-minute plan. This includes:
- Quickly checking the patient’s condition
- Getting the cardiac catheterization lab ready
- Preparing for possible treatments
“Time is muscle” is a saying in cardiology that shows how urgent action is.
“The American Heart Association stresses the importance of quick reperfusion therapy for acute myocardial infarction.”
Revascularization Strategies and Timing
Revascularization is a vital part of treating anterior myocardial infarction. We look at several options:
- Primary percutaneous coronary intervention (PCI)
- Thrombolysis
- Pharmacotherapy
The right revascularization method depends on the patient’s situation and what’s available. Primary PCI is usually the best choice when it can be done quickly.
Revascularization Strategy | Timing | Clinical Considerations |
Primary PCI | Within 90 minutes of diagnosis | Best for patients who can’t get thrombolysis |
Thrombolysis | Within 30 minutes of diagnosis | Used when PCI is not available |
Post-Intervention Monitoring
After treatment, we keep a close eye on the patient. We focus on:
- Checking vital signs
- Testing for cardiac biomarkers
- Monitoring the heart with an ECG
Secondary Prevention Measures
Secondary prevention is key for patients after myocardial infarction. We suggest:
- Making lifestyle changes like diet and exercise
- Using medicines like antiplatelets and statins
- Managing risk factors like high blood pressure and diabetes
These steps help improve long-term results for patients with anterior myocardial infarction.
Comprehensive Approach to Optic Nerve Disorders
Managing optic nerve disorders needs a deep understanding of their types, diagnosis, and treatments. We will look at all parts of optic nerve disorders. This will give you a full view of how to manage them.
Classification of Anterior Visual Pathway Diseases
Optic nerve disorders can be grouped by their cause. These causes include inflammation, compression, ischemia, and trauma. Knowing the cause helps decide the best treatment.
- Inflammatory Causes: Conditions like optic neuritis need quick medical help.
- Compressive Causes: Tumors or aneurysms pressing on the optic nerve can cause vision loss if not treated fast.
- Ischemic Causes: Ischemic optic neuropathy happens when the optic nerve doesn’t get enough blood.
- Traumatic Causes: Head or eye injuries can hurt the optic nerve, needing fast medical care.
Diagnostic Workup for Optic Nerve Abnormalities
Identifying the cause of optic nerve disorders needs a detailed check-up. This includes a full medical history, vision tests, and scans like MRI or CT.
Lab tests might also be done to find other conditions that could be causing the problem.
Medical Management Protocols
How to treat optic nerve disorders depends on the cause. For inflammation, doctors might use corticosteroids. For ischemic optic neuropathy, managing risks like high blood pressure and diabetes is key.
Surgical Interventions for Optic Nerve Decompression
When the optic nerve is compressed, surgery might be needed to fix it. This could mean removing a tumor or draining an abscess.
Surgery to relieve optic nerve compression is very careful. It aims to improve vision and avoid more harm.
Managing Temporomandibular Joint Anterior Disc Displacement
Managing temporomandibular joint anterior disc displacement needs a mix of clinical checks and treatment plans. We must look at different ways to help patients feel better and get better results.
Clinical Assessment and Classification
Starting with a good clinical check is key. This includes talking to the patient, doing a physical exam, and sometimes, imaging tests. Getting the right diagnosis helps decide the best treatment.
“The way patients show symptoms can be different, so we need to be flexible with treatment,” say experts.
Conservative Management Strategies
First, we try non-surgical methods. This includes teaching patients, doing jaw exercises, and using mouthpieces. Teaching patients how to manage their condition is very important.
- Teaching about jaw mechanics and pain control
- Physical therapy to help jaw movement
- Mouthpieces to adjust jaw position
Surgical Approaches and Patient Selection
If non-surgical methods don’t work, surgery might be needed. This could be arthrocentesis, arthroscopy, or open surgery. Picking the right patients for surgery is very important.
Long-term Maintenance and Follow-up
Keeping up with treatment long-term is important to avoid symptoms coming back. Regular check-ups and sticking to the treatment plan are essential. Watching for changes and adjusting treatment as needed is important for long-term success.
In conclusion, managing temporomandibular joint anterior disc displacement needs a full approach. By using clinical checks, non-surgical methods, and sometimes surgery, we can greatly improve patient results.
Multidisciplinary Team Approach to Anterior Disease
Managing anterior disease is better with a team of experts from different fields. At Liv Hospital, we work together to give our patients the best care. This team effort brings together many specialties for a complete approach.
Core Team Composition
Our team includes orthopedic surgeons, cardiologists, neurologists, and physical therapists. Working together is key to creating a solid treatment plan.
Specialty | Role in Anterior Disease Management |
Orthopedic Surgeon | Surgical interventions for musculoskeletal conditions |
Cardiologist | Management of cardiovascular aspects, including myocardial infarction |
Neurologist | Diagnosis and treatment of neurological conditions affecting the anterior visual pathway |
Physical Therapist | Rehabilitation and physical therapy protocols |
Coordinated Care Pathways
Coordinated care is key for seamless and complete care. We create a detailed plan for each patient. This plan covers everything from diagnosis to follow-up care.
- Initial assessment and diagnosis
- Treatment planning and implementation
- Regular follow-up and monitoring
- Adjustments to the treatment plan as necessary
Patient-Centered Decision Making
We put patients at the center of our care. We make sure their wishes and values are heard. This teamwork leads to better treatment results.
Communication Strategies Among Specialists
Good communication among team members is essential. We use team meetings and secure messages to keep everyone on the same page. This helps us work better together for our patients.
Our team approach leads to better care for patients with anterior disease. We see better results and happier patients.
Personalized Treatment Plans for Anterior Disease
Managing anterior disease well means having a plan made just for you. We know every patient is different. So, we tailor our approach to get the best results.
Risk Stratification Models
Risk stratification is key in making treatment plans. It helps us find out who is at higher risk. This way, we can focus on those who need it most.
Important things to look at include:
- Patient history: Past health, allergies, and how they’ve reacted to treatments.
- Genetic predisposition: Family health history and genes linked to the disease.
- Lifestyle factors: Smoking, exercise, and diet.
Tailoring Interventions to Patient Profiles
After figuring out the risk, we tailor treatments to fit each patient. This might include non-surgical methods, surgery, and rehab.
For example, those with ACL injuries might get:
- First, a check-up and diagnosis.
- Then, non-surgical care like physical therapy and bracing.
- If needed, surgery to fix the ACL.
- After surgery, rehab and check-ups to make sure they’re healing right.
Monitoring Response and Treatment Adjustments
It’s important to keep an eye on how treatments are working. We use doctor visits, tests, and what patients tell us to adjust plans as needed.
Long-term Management Considerations
Managing anterior disease is a long-term job. It needs ongoing care to stop problems and keep the disease from getting worse. We help patients make a plan for the long haul. This includes lifestyle changes, sticking to medication, and regular check-ups.
By treating each patient as an individual, we can make their lives better. We also save money and improve health care overall.
Emerging Therapies and Future Directions
We’re making big strides in treating anterior disease. New therapies are changing how we approach treatment. These innovations aim to better patient care and life quality.
Regenerative Medicine Applications
Regenerative medicine is leading the way in treating anterior disease. It focuses on fixing or replacing damaged tissues. This could offer real cures for conditions that were once just managed.
- Stem Cell Therapy: Uses stem cells to grow new tissues, like ligaments and heart muscle.
- Tissue Engineering: Makes new tissues to replace or support damaged ones.
- Platelet-rich Plasma (PRP) Therapy: Uses PRP to help damaged tissues heal.
Novel Pharmacological Approaches
New medicines are being made to target specific disease pathways. These include:
- Biologics: Uses antibodies and other biologics to fight inflammation.
- Gene Therapy: Changes genes to prevent or treat disease.
- Personalized Medicine: Makes treatments fit each patient’s needs.
Technological Innovations in Treatment
New tech is changing how we treat anterior disease. Key advancements include:
- Robotic-assisted Surgery: Makes surgery more precise and effective.
- Advanced Imaging Techniques: Helps diagnose and guide treatment better.
- Wearable Devices: Tracks patient activity and health in real-time.
Promising Research Developments
Research into anterior disease is making progress. Some exciting developments are:
- Investigations into Disease Mechanisms: Helps understand disease causes for better treatments.
- Clinical Trials: Tests new therapies for safety and effectiveness.
- Collaborative Research Initiatives: Brings together experts to drive innovation.
These new therapies and research are very promising. They could greatly improve how we manage anterior disease. As we keep moving forward, we’ll see better patient outcomes and life quality.
Conclusion: Optimizing Outcomes in Anterior Disease Management
Improving outcomes in anterior disease management needs a full approach. This includes working together and using many care methods. We’ve talked about the different parts of anterior disease, like its range, signs, how to diagnose it, and how to treat it.
Healthcare teams can make a big difference by understanding the disease well. They can create a treatment plan that fits each patient. Getting support from many areas of care is key to the best results.
Our study shows how vital it is to focus on better outcomes in managing anterior disease. Using the newest research, tech, and treatments can make patient care better. Managing anterior disease well is a team effort. It needs the work of doctors, patients, and their families.
FAQ
What is anterior disease, and how common is it?
Anterior disease refers to conditions affecting the front parts of our bodies. It can happen in different areas, like the knees or eyes. The frequency of these conditions varies.
What are the symptoms of anterior disease, and how do they vary?
Symptoms can include pain, swelling, and vision issues. For example, eye pain and light sensitivity are signs of anterior uveitis. Knee instability is a symptom of anterior cruciate ligament injuries.
How are anterior diseases diagnosed?
Doctors use a combination of physical exams, imaging like MRI or CT scans, and lab tests. Special tests might be needed for certain conditions, like anterior uveitis.
What are the treatment options for anterior cruciate ligament conditions?
Treatment options include managing the acute phase, conservative treatments, surgery, and rehabilitation. The choice depends on the injury’s severity and the patient’s needs.
How is anterior myocardial infarction managed?
Management includes a quick response, revascularization, monitoring, and prevention. Quick action is key to better outcomes.
What is the approach to managing optic nerve disorders?
Management involves classifying the condition, diagnostic tests, medical treatments, and surgery. Quick diagnosis and proper treatment are vital for the best results.
How is temporomandibular joint anterior disc displacement treated?
Treatment includes assessing the condition, conservative treatments, surgery, and maintenance. Tailored plans are necessary for effective treatment.
Why is a multidisciplinary team important in managing anterior disease?
A team approach ensures complete care through coordinated efforts. It focuses on patient-centered decisions and effective communication among specialists.
How are personalized treatment plans developed for anterior disease?
Plans are tailored using risk models, individual patient profiles, monitoring, and long-term management. This approach improves treatment outcomes.
What emerging therapies are being explored for anterior disease?
New therapies include regenerative medicine, novel drugs, technology, and research. These innovations aim to enhance patient care.
What is the significance of optic nerve disorders and their management?
Optic nerve disorders need quick diagnosis and treatment to avoid vision loss. Proper management is essential for better outcomes.
How do ocular nerve disorders impact vision?
These disorders can cause vision problems like blurred or double vision. The severity of the condition affects the impact on vision.
What are the common issues with the optic nerve?
Common issues include optic nerve disorders and diseases. They can result from trauma, infection, or systemic conditions.





