The third cranial nerve, or oculomotor nerve (CN III), is key for eye movements, opening eyelids, and narrowing pupils. It has motor, parasympathetic, and sympathetic fibers. This makes it essential for our vision. Wondering what does cranial nerve 3 do? Our amazing guide explains its 2 critical functions and the alarming “down and out” palsy sign.
Damage to cranial nerve 3 can cause big vision issues. These include seeing double and eyelids that droop. Knowing how this nerve works is key to diagnosing and treating problems.
Key Takeaways
- The oculomotor nerve controls eye movements and pupil constriction.
- Damage to cranial nerve 3 can cause double vision and ptosis.
- Understanding the nerve’s functions is vital for diagnosis and treatment.
- Cranial mononeuropathy III affects the third cranial nerve’s function.
- Early detection is vital for managing related disorders.
Overview of the Oculomotor Nerve (CN III)

The oculomotor nerve (CN III) is one of the twelve cranial nerves. It plays a key role in vision and eye movement. This nerve controls important eye functions, making it essential for our sight.
Definition and Basic Function
The oculomotor nerve, or the third cranial nerve, controls the movement of extraocular muscles. It works with the superior, medial, inferior rectus, and inferior oblique muscles. These muscles help us move our eyes in different ways.
It also helps control the lens and pupil. This is done through parasympathetic innervation. This function is vital for focusing and adjusting to light.
The oculomotor nerve has three main functions: 1. It helps us focus and track with our eyes. 2. It controls the lens and pupil for focusing and light adjustment. 3. It helps coordinate eye movements during various activities.
- Innervation of extraocular muscles for eye movement.
- Parasympathetic control for lens accommodation and pupil constriction.
- Coordination of eye movements for tracking and gaze fixation.
Position Among Cranial Nerves
The oculomotor nerve is the third cranial nerve. It is vital for eye movement and control. It starts in the midbrain and goes through the skull to reach its muscles.
It works with other nerves like the trochlear and abducens nerves for smooth eye movements. Damage to this nerve can cause serious vision problems. This can happen due to many reasons, like blood vessel issues, injuries, or pressure on the nerve.
Anatomy and Path of Cranial Nerve 3
Knowing how Cranial Nerve 3 works is key to treating its problems. This nerve, also called the oculomotor nerve, has a complex path. It’s important for its role in our body.
Origin in the Midbrain
Cranial Nerve 3 starts in the midbrain. It comes from two parts: the oculomotor nucleus and the Edinger-Westphal nucleus. The oculomotor nucleus handles the nerve’s motor functions. The Edinger-Westphal nucleus deals with its parasympathetic functions.
The nerve fibers leave the brainstem near the midline. They are just below the mammillary bodies.
Course Through the Skull
After leaving the brainstem, Cranial Nerve 3 goes between two arteries. It then goes through the dura mater and into the cavernous sinus. Inside the cavernous sinus, it’s near the internal carotid artery and other nerves.
It goes through the supraorbital fissure to get to the eye’s orbit.
Problems at different points in the nerve’s path can cause different symptoms. For example, a problem in the cavernous sinus can affect other nerves, leading to complex symptoms.
Terminal Branches
When it reaches the orbit, Cranial Nerve 3 splits into two parts. The superior division goes to the superior rectus and levator palpebrae superioris muscles. The inferior division goes to the medial, inferior rectus, and inferior oblique muscles. It also sends parasympathetic fibers to the ciliary ganglion for eye functions.
Branch | Muscle Innervated | Function |
Superior Division | Superior Rectus | Elevation of the eyeball |
Superior Division | Levator Palpebrae Superioris | Elevation of the eyelid |
Inferior Division | Medial Rectus | Adduction of the eyeball |
Inferior Division | Inferior Rectus | Depression of the eyeball |
Inferior Division | Inferior Oblique | Elevation and extorsion of the eyeball |
Damage to Cranial Nerve 3 can cause serious eye problems. This includes cranial nerve iii palsy or cranial nerve 3 paralysis. It can lead to ptosis, diplopia, and pupillary dilation. Knowing the nerve’s anatomy and path is key for diagnosis and treatment.
What Does Cranial Nerve 3 Do?
Cranial Nerve 3, or the oculomotor nerve, controls eye movements, pupil size, and lens focus. It plays a key role in how we see and interact with the world.
Motor Functions
The oculomotor nerve controls five eye muscles. These include the superior rectus, medial rectus, inferior rectus, inferior oblique, and levator palpebrae superioris. These muscles help us move our eyes precisely.
For example, the superior rectus lifts the eye. The medial rectus moves the eye inward.
The oculomotor nerve’s motor functions include:
- Innervation of extraocular muscles for eye movement
- Control of the levator palpebrae superioris for eyelid elevation
- Coordination of eye movements for tracking objects
Parasympathetic Functions
The oculomotor nerve also controls pupil size and lens focus. It does this through parasympathetic fibers. These fibers affect the sphincter pupillae muscle and the ciliary muscles.
Damage to this nerve can cause large pupils and trouble with light reflexes. This shows how vital its parasympathetic functions are.
Sympathetic Components
The oculomotor nerve mainly has parasympathetic fibers. But it also works with sympathetic components. This teamwork helps the eye adjust to light changes and focus on objects.
This complex control is key for normal vision and adapting to the environment.
Extraocular Muscles Innervated by CN III
It’s important to know about the extraocular muscles controlled by CN III. This knowledge helps in diagnosing and treating eye movement problems. The oculomotor nerve, or Cranial Nerve 3, controls several key muscles for eye movement.
Superior Rectus
The superior rectus muscle is controlled by CN III. It mainly helps in lifting the eye, which is important for looking up. If this muscle is weak, it can be hard to look up.
Medial Rectus
The medial rectus muscle is also controlled by CN III. It helps move the eye towards the body’s center. This muscle is essential for smooth eye movements and focusing.
Inferior Rectus
The inferior rectus muscle is controlled by CN III. It helps lower the eye, making it easier to look down. If this muscle doesn’t work right, it can be hard to look down.
Inferior Oblique
The inferior oblique muscle is controlled by CN III. It helps rotate the eye outward, lift it, and move it away from the nose. Its actions are important for precise eye movements.
Problems with CN III can cause muscle weakness or paralysis. This can lead to double vision and other eye movement issues. Knowing which muscles CN III controls is key for diagnosing and treating these problems.
Pupillary and Accommodation Control
The oculomotor nerve is key in controlling how our eyes work. It helps our pupils adjust to light and focuses on close objects. This is done through its parasympathetic fibers.
Pupillary Light Reflex
The pupillary light reflex is how our pupils get smaller in bright light. This reflex is controlled by the oculomotor nerve. It sends signals from the Edinger-Westphal nucleus to the ciliary ganglion and then to the sphincter pupillae muscle.
When light hits our eyes, it sends signals to the midbrain. The midbrain then tells the oculomotor nerve to make the pupil smaller.
Damage to cranial nerve 3 can make the pupil stay big and not react to light. This is a sign of oculomotor nerve palsy. It can be caused by many things, like blood vessel problems, injuries, or tumors.
Component | Function | Effect of Damage to CN III |
Parasympathetic Fibers | Control pupil constriction and lens accommodation | Impaired pupillary light reflex, dilated pupil |
Oculomotor Nerve | Transmits signals for pupillary constriction and lens accommodation | Pupillary dysfunction, impaired near vision |
Lens Accommodation
Lens accommodation is how our eyes adjust to focus on objects at different distances. The oculomotor nerve helps by controlling the ciliary muscles. These muscles contract to make the lens rounder for near vision.
Damage to the oculomotor nerve can make it hard to focus on close objects. This can cause blurry vision and eye strain, like when reading or using a computer.
Knowing how the oculomotor nerve works is important for diagnosing and treating eye problems. Recognizing signs of damage, like trouble with the pupillary light reflex and lens accommodation, helps doctors help their patients.
Oculomotor Nerve Palsy: Types and Presentation
Oculomotor nerve palsy is a complex condition. It can show up in different ways, based on the damage to the third cranial nerve. This nerve controls many eye movements, pupil constriction, and eyelid opening.
We will look at the different types of oculomotor nerve palsy and how they present. This is key for diagnosis and treatment. The types are based on how much of the nerve is affected and if the pupil works right.
Complete vs. Partial Palsy
Oculomotor nerve palsy can be either complete or partial. Complete oculomotor nerve palsy means the nerve is totally damaged. This leads to big problems with eye movement.
Partial oculomotor nerve palsy affects only some of the nerve’s functions. This results in less severe symptoms and variable eye movement issues.
Characteristics | Complete Palsy | Partial Palsy |
Eye Movement Limitation | Total paralysis of oculomotor innervated muscles | Variable duction limitations |
Pupillary Involvement | Often dilated pupil | May have pupillary dysfunction |
Ptosis | Typically present | May be present or absent |
Pupil-Involving vs. Pupil-Sparing Palsy
Another important difference is if the pupil is affected. Pupil-involving palsy means the pupil is not working right. This often makes the pupil dilate.
Pupil-sparing palsy means the pupil works fine. This suggests the damage is not as bad or only affects certain nerve fibers.
Knowing these differences helps doctors figure out what’s causing oculomotor nerve palsy. Pupil-involving palsy can mean a serious problem, like an aneurysm.
By accurately diagnosing and classifying oculomotor nerve palsy, doctors can create the right treatment plan for each patient.
Common Causes of Cranial Nerve 3 Damage
It’s important to know why the third cranial nerve gets damaged. This nerve controls eye movements and how pupils get smaller. Damage can come from many different problems.
Vascular Disorders
Vascular disorders are a big reason for nerve damage. Diabetes and hypertension can harm the nerve because they affect blood vessels. For example, diabetes can cause nerve damage, leading to palsy. High blood pressure can also damage the nerve through vascular changes.
- Diabetes mellitus
- Hypertension
- Atherosclerosis
Trauma
Head injuries can damage the oculomotor nerve. The force of the injury can compress or stretch the nerve, causing palsy. The extent of the injury determines the severity of the damage.
Common causes include:
- Head injuries from accidents
- Falls
- Sports-related injuries
Tumors and Space-Occupying Lesions
Tumors and other lesions can press on the nerve, causing damage. These can be benign or cancerous and come from nearby or spread from elsewhere.
Examples include:
- Pituitary tumors
- Meningiomas
- Metastatic tumors
Inflammatory and Infectious Causes
Inflammation and infections can also harm the nerve. Meningitis or encephalitis can cause inflammation. Infections like syphilis or tuberculosis can also affect the nerve.
Examples include:
- Meningitis
- Encephalitis
- Syphilis
- Tuberculosis
Knowing these causes helps doctors diagnose and treat nerve damage. Understanding the cause allows for the right treatment, helping patients get better.
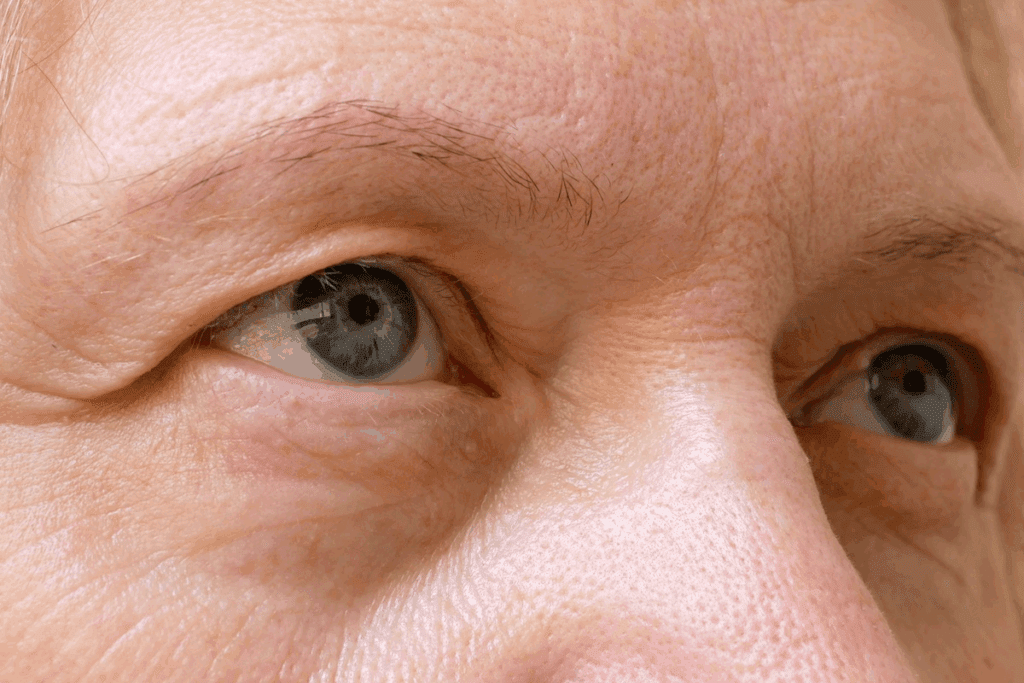
Clinical Symptoms of Oculomotor Nerve Damage
Damage to the oculomotor nerve can cause many symptoms that affect a person’s life. This nerve, or cranial nerve 3, controls eye movements and functions.
Ptosis (Drooping Eyelid)
Ptosis, or a drooping eyelid, is a common symptom. It happens because the oculomotor nerve helps the levator palpebrae superioris muscle lift the eyelid.
Diplopia (Double Vision)
Diplopia, or double vision, can also occur. Damage to the nerve weakens or paralyzes the extraocular muscles. This misalignment causes double vision.
Pupillary Dilation
Pupillary dilation, or mydriasis, is another symptom. Damage to the nerve’s parasympathetic fibers leads to a dilated pupil on the affected side.
“Down and Out” Eye Position
A “down and out” eye position is a sign of oculomotor nerve palsy. This happens because the muscles not controlled by the oculomotor nerve, like the superior oblique and lateral rectus, work alone.
The symptoms of oculomotor nerve damage vary based on the damage’s extent and location. Knowing these symptoms is key to proper care and management.
Symptom | Description | Cause |
Ptosis | Drooping or falling of the upper eyelid | Weakness of levator palpebrae superioris muscle |
Diplopia | Double vision | Misalignment of the eyes due to extraocular muscle weakness |
Pupillary Dilation | Dilated pupil | Damage to parasympathetic fibers controlling pupil constriction |
“Down and Out” Eye Position | Characteristic deviation of the eye | Unopposed action of superior oblique and lateral rectus muscles |
Diagnosis and Differential Diagnosis
Diagnosing oculomotor nerve palsy involves several steps. We start with a detailed clinical exam. This helps us see how much nerve damage there is and any other symptoms.
Clinical Examination
A thorough clinical exam is key to diagnosing oculomotor nerve damage. We look for signs like ptosis (drooping eyelid), diplopia (double vision), and pupillary dysfunction. These signs tell us how severe the damage is and what might have caused it.
Imaging Studies
Imaging studies are vital in finding the cause of oculomotor nerve palsy. We often use MRI or CT scans. They help us see if there are compressive lesions, vascular abnormalities, or other pathologies affecting the nerve.
Imaging Modality | Use in Diagnosing Oculomotor Nerve Palsy | Key Findings |
MRI | Detailed visualization of soft tissues, including nerves and surrounding structures | Compression by aneurysms, tumors, or inflammatory lesions |
CT Scan | Quick assessment of acute hemorrhage or bony abnormalities | Fractures, calcifications, or acute bleeding |
MRA | Visualization of blood vessels and detection of vascular abnormalities | Aneurysms, stenosis, or vascular malformations |
Distinguishing from Other Cranial Nerve Disorders
Differential diagnosis is key to tell oculomotor nerve palsy from other cranial nerve disorders. We must look at conditions affecting other nerves, like the trochlear or abducens nerves. We also need to rule out other causes of diplopia or ptosis.
By combining clinical findings with imaging studies, we can accurately diagnose oculomotor nerve damage. This helps us tell it apart from other conditions. A detailed approach is essential for a good treatment plan.
Treatment and Management Options
Treating cranial nerve 3 damage involves several steps. It depends on the cause. A mix of medical treatments, surgeries, and supportive therapies is used. Each plan is made for the patient’s needs.
Medical Interventions
Medical treatments are key in managing cranial nerve 3 damage. This is true when the cause is related to health issues. For example, managing diabetes and high blood pressure can help recovery. Changing lifestyle and using medicine are often the first steps in treatment.
A leading medical journal says, “Managing vascular risk factors is key in treating oculomotor nerve palsy.”
“The importance of managing hypertension and diabetes cannot be overstated, as these conditions are often associated with cranial nerve III palsy.”
- Managing underlying conditions like diabetes and hypertension
- Using medications to alleviate symptoms or address the underlying cause
- Monitoring patient progress to adjust treatment plans as necessary
Surgical Approaches
Surgery is needed when cranial nerve 3 damage is caused by blockages or structural problems. Surgery can help by removing blockages or fixing damaged nerves.
Surgical Approach | Indications | Benefits |
Craniotomy | Compressive lesions, aneurysms | Relieves pressure on the nerve |
Nerve decompression | Nerve compression due to trauma or tumors | Improves nerve function |
Supportive Therapies and Rehabilitation
Supportive therapies help manage symptoms and improve life quality for patients. These include eye exercises, prism glasses, and ptosis crutches. They help with double vision and eyelid support.
Rehabilitation aims to use what nerve function is left and find ways to make up for lost function. A team of ophthalmology, neurology, and rehabilitation specialists is needed for full care.
Conclusion
Damage to cranial nerve 3 can cause serious symptoms like ptosis, diplopia, and pupillary dilation. This nerve issue affects the oculomotor nerve, leading to eye movement problems.
We’ve looked into the anatomy and functions of cranial nerve 3. It’s key for eye movements, pupil size, and lens adjustment. Knowing how to diagnose and treat damage is vital for patient care.
Managing cranial nerve palsy 3 needs a team effort. This includes medical treatments, surgery, and supportive therapies. By grasping the details of cranial nerve 3, we can better help patients and improve their lives.
FAQ
What is the primary function of cranial nerve 3?
Cranial nerve 3, also known as the oculomotor nerve, controls eye movements. It also controls pupil constriction and lens accommodation. It innervates multiple extraocular muscles and regulates pupil size.
What are the symptoms of oculomotor nerve damage?
Damage to the oculomotor nerve can cause double vision (diplopia) and a drooping eyelid (ptosis). It can also lead to pupillary dilation and impaired near vision.
What causes oculomotor nerve palsy?
Oculomotor nerve palsy can be caused by vascular disorders, trauma, tumors, and inflammatory or infectious conditions.
How is oculomotor nerve damage diagnosed?
Diagnosing oculomotor nerve damage requires a thorough clinical examination. It also needs imaging studies to assess nerve damage and rule out other disorders.
What are the treatment options for oculomotor nerve damage?
Treatment for oculomotor nerve damage involves a wide range of options. This includes medical interventions, surgical options, and supportive therapies. These aim to address symptoms and improve outcomes.
Can oculomotor nerve palsy be classified into different types?
Yes, oculomotor nerve palsy can be classified into different types. This classification is based on the extent of nerve involvement and the presence or absence of pupillary dysfunction.
What is the role of cranial nerve 3 in controlling pupil size?
Cranial nerve 3 controls pupil size through its parasympathetic functions. It regulates pupil constriction in response to light and near vision.
How does damage to cranial nerve 3 affect eye movements?
Damage to cranial nerve 3 can impair eye movements. This is because it innervates multiple extraocular muscles. Symptoms include double vision and “down and out” eye position.
What are the extraocular muscles innervated by cranial nerve 3?
Cranial nerve 3 innervates the superior rectus, medial rectus, inferior rectus, and inferior oblique muscles. These muscles control various eye movements.
What is the significance of understanding the anatomy of cranial nerve 3?
Understanding the anatomy of cranial nerve 3 is key for diagnosing and managing related disorders. Its origin, course, and terminal branches all play critical roles in its function.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1279674/