Ever wondered how your eyes move so smoothly in all directions? The oculomotor, trochlear, and abducens nerves work together. They control every eye movement and reflex. At Liv Hospital, we know how vital it is to understand these nerves. The best guide to the oculomotor trochlear and abducens nerves. Learn how these 3 amazing nerves (CN 3, 4, 6) control your eyes.
These nerves are key to diagnosing and treating eye problems. We’ll look at how they help the extraocular muscles move the eyes precisely.
Key Takeaways
- The oculomotor, trochlear, and abducens nerves control the extraocular muscles.
- Damage to these nerves can cause double vision and eye movement dysfunction.
- Understanding their anatomy and function is essential for diagnosis and treatment.
- These nerves start from different parts of the brainstem.
- Precise eye movements are made possible by the teamwork of these three cranial nerves.
The Fundamentals of Cranial Nerves Controlling Eye Movement
The oculomotor, trochlear, and abducens nerves are key for eye movement. They work together to let our eyes move, track objects, and stay focused. Knowing how they work helps us understand the eye’s complex movements.
Classification of Cranial Nerves
Cranial nerves are divided into sensory, motor, or mixed types. The oculomotor (CN III), trochlear (CN IV), and abducens (CN VI) nerves are motor nerves. They control the muscles that move the eye.
Significance of Pure Motor Nerves in Ocular Function
The oculomotor, trochlear, and abducens nerves are essential for eye movement. The oculomotor nerve (CN III) controls four muscles. The trochlear nerve (CN IV) and abducens nerve (CN VI) control the other two. They work together for precise eye movements.
Embryological Development of Eye Movement Nerves
The development of eye movement nerves is tied to the eye’s formation. During growth, the nerves and muscles form together. This is key for eye movement to work right. Problems during this time can cause eye movement issues.
The Oculomotor Nerve (CN III): Anatomy and Origin
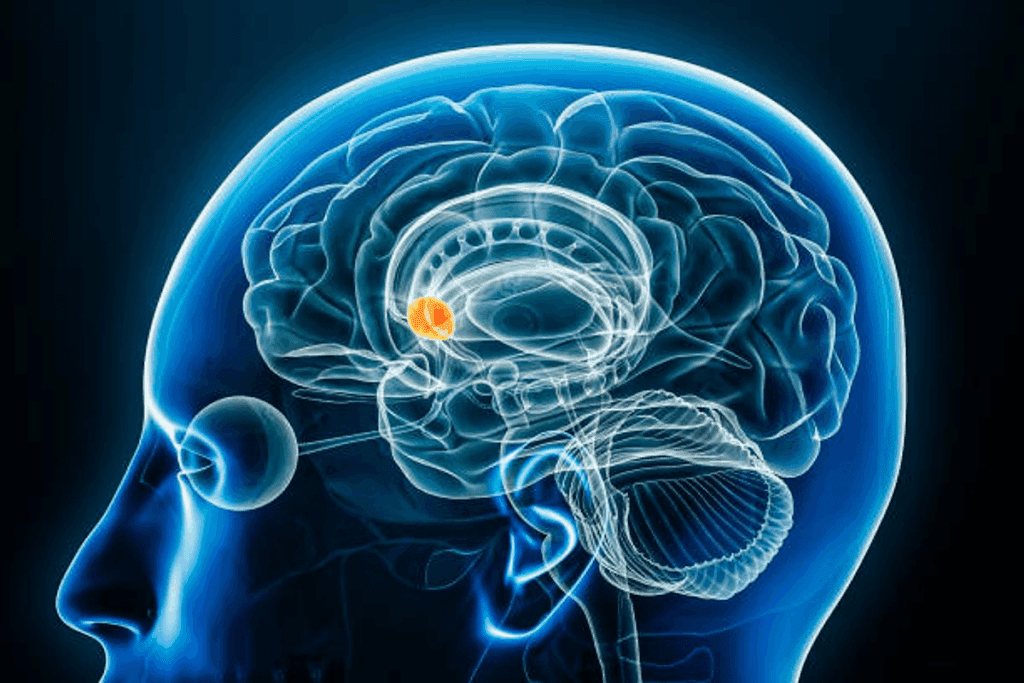
The oculomotor nerve, or CN III, starts in the midbrain. It plays a key role in controlling eye muscles and how the pupils open and close. Knowing its anatomy helps doctors diagnose and treat eye problems.
Nuclei in the Midbrain
The oculomotor nerve comes from the oculomotor nucleus in the midbrain. This nucleus controls most of the eye’s muscles. These include the medial rectus, superior rectus, inferior rectus, and inferior oblique muscles.
Course from Brainstem to Orbit
After starting in the oculomotor nucleus, the nerve fibers move through the midbrain. They come out between the cerebral peduncles. Then, they pass between two arteries before reaching the cavernous sinus.
Passage Through the Cavernous Sinus
In the cavernous sinus, the oculomotor nerve is near other nerves. It’s close to the trochlear nerve and the ophthalmic division of the trigeminal nerve. It then goes into the orbit through the superior orbital fissure.
Characteristics | Description |
Origin | Midbrain |
Course | Between cerebral peduncles, through cavernous sinus, into orbit via superior orbital fissure |
Functions | Controls medial rectus, superior rectus, inferior rectus, inferior oblique muscles, and pupillary constriction |
Functions of the Oculomotor Nerve
The oculomotor nerve is key for eye movements, making pupils smaller, and focusing on close objects. It controls important functions that help us see and interact with our world.
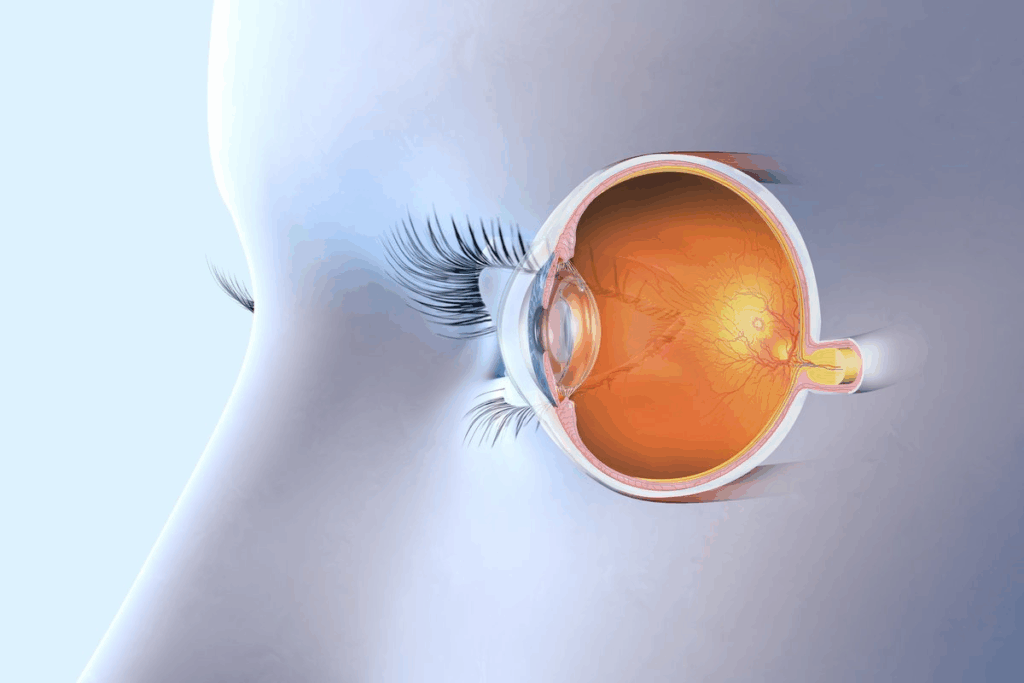
Innervation of Four Extraocular Muscles
The oculomotor nerve helps four of the six muscles that move the eyeball. These are the medial rectus, superior rectus, inferior rectus, and inferior oblique muscles. The medial rectus pulls the eye inward. The superior and inferior rectus muscles move the eye up and down. The inferior oblique helps the eye move up and out.
Pupillary Constriction Mechanism
The oculomotor nerve also makes the pupil smaller. This happens when light hits the eye. The nerve’s parasympathetic fibers make the sphincter pupillae muscle contract. This is called the pupillary light reflex and helps control how much light gets in.
Accommodation for Near Vision
The oculomotor nerve is also important for focusing on close objects. When we look at something near, it makes the ciliary muscles contract. This makes the lens rounder, helping us see clearly at different distances.
The Trochlear Nerve (CN IV): Anatomy and Origin
The trochlear nerve is unique among cranial nerves. It controls eye movements and is the fourth cranial nerve. We’ll look at its origins in the midbrain, its special path, and how it reaches the eye.
Nuclei in the Midbrain
The trochlear nerve starts in the midbrain, near the inferior colliculus. It controls the superior oblique muscle. Its nucleus is special because it’s near the midline and its axons cross over before leaving the brainstem.
Unique Decussation and Dorsal Exit
The trochlear nerve’s path is unique. Its axons cross over to the opposite side before leaving the midbrain. This means it controls the superior oblique muscle on the opposite side. It’s the only cranial nerve to exit the brainstem from the top.
Path Through the Cavernous Sinus to Superior Orbital Fissure
After leaving the brainstem, the trochlear nerve goes through the subarachnoid space. It then goes through the dura mater to enter the cavernous sinus. Inside, it runs with other nerves. It then goes through the superior orbital fissure to get to the orbit.
There, it connects with the superior oblique muscle. This muscle helps rotate the eye downward and inward. The nerve’s long path makes it prone to injury. Knowing its anatomy helps in diagnosing and treating nerve problems.
Key Points:
- The trochlear nerve originates from the trochlear nucleus in the midbrain.
- It decussates before exiting the brainstem dorsally.
- The nerve passes through the cavernous sinus and superior orbital fissure to innervate the superior oblique muscle.
Functions of the Trochlear Nerve
It’s important to know how the trochlear nerve works. This nerve, or cranial nerve IV, helps our eyes move together. It controls the eye’s movements.
Superior Oblique Muscle Innervation
The trochlear nerve is special because it controls a muscle on the opposite side of the body. It works with the superior oblique muscle. This muscle helps us look down and in, which we need for reading or going down stairs.
The nerve’s connection to the superior oblique muscle is complex. It starts in the midbrain and crosses over before leaving the brainstem. This unique crossing ensures each eye is controlled by the opposite side of the brain.
Role in Downward and Inward Gaze
The trochlear nerve mainly helps us look down and in. This is key for reading or walking down stairs. The superior oblique muscle makes these movements smooth and coordinated.
- The trochlear nerve enables precise control over the superior oblique muscle, facilitating complex eye movements.
- The downward and inward gaze controlled by the trochlear nerve is essential for daily activities that require visual coordination.
- Dysfunction of the trochlear nerve can lead to difficulties in performing tasks that require coordinated eye movements.
In summary, the trochlear nerve is key for controlling the superior oblique muscle. This muscle is vital for looking down and in. Knowing how the trochlear nerve works helps us understand eye movement and coordination better.
The Abducens Nerve (CN VI): Anatomy and Origin
The abducens nerve starts in the pons. It has a complex path that’s key for eye movement. We’ll dive into its detailed anatomy and where it begins.
Nuclei in the Pons
The abducens nucleus in the pons is where the nerve begins. This nucleus controls the lateral rectus muscle.
Long Intracranial Course
The abducens nerve’s path inside the skull is long. This makes it prone to damage. It goes up the base of the pons, then through the subarachnoid space. Next, it crosses the cavernous sinus.
Passage Through Cavernous Sinus to Superior Orbital Fissure
After the cavernous sinus, the nerve goes into the orbit. It enters through the superior orbital fissure. There, it helps the lateral rectus muscle move the eye outward.
Functions of the Abducens Nerve
It’s important to know how the Abducens nerve helps our eyes move together. This nerve, the sixth cranial nerve, controls a key action in eye movement.
Lateral Rectus Muscle Innervation
The Abducens nerve mainly works with the lateral rectus muscle. This muscle is part of the six muscles that move our eyes. It’s special because it moves the eye outward, or away from the nose.
Innervation Process: The nerve starts in the pons, goes through the brain, and ends at the lateral rectus muscle. This journey shows how vital the nerve is and how it can get hurt.
Horizontal Eye Abduction Mechanics
The Abducens nerve helps the lateral rectus muscle move the eye sideways. This is key for looking to the side without turning our head. The muscle works with another muscle to move the eye smoothly.
Muscle | Nerve Innervation | Primary Action |
Lateral Rectus | Abducens Nerve (CN VI) | Abduction |
Medial Rectus | Oculomotor Nerve (CN III) | Adduction |
The table shows the Abducens nerve’s big role in eye movement. If it doesn’t work right, we can’t move our eyes well. This shows how important it is for our vision.
In short, the Abducens nerve is key for moving the eye sideways. Knowing how it works helps us understand how we see and move our eyes.
Comparing the Oculomotor, Trochlear, and Abducens Nerves
It’s important to know how the oculomotor, trochlear, and abducens nerves are similar and different. They work together to help our eyes move smoothly. This knowledge helps doctors diagnose and treat eye problems.
Anatomical Similarities and Differences
The oculomotor, trochlear, and abducens nerves have some similarities but also key differences. They all start in the brainstem and control the eye muscles. But, they start from different parts of the brainstem and follow different paths to the eye.
- The oculomotor nerve (CN III) starts in the midbrain and controls four eye muscles and the eyelid muscle.
- The trochlear nerve (CN IV) also starts in the midbrain but has a special path. It controls the superior oblique muscle.
- The abducens nerve (CN VI) starts in the pons and has a long path to the eye. It controls the lateral rectus muscle.
Functional Integration in Eye Movement
Even though they are different, the oculomotor, trochlear, and abducens nerves work together. They help us track objects, read, and drive by controlling eye movements.
Their teamwork is essential for:
- Smooth pursuit movements
- Saccadic movements
- Vergence movements
Vulnerability to Injury Based on Anatomical Course
The path each nerve takes affects how likely it is to get hurt. For example, the abducens nerve is more at risk because of its long path through the brain.
Key factors influencing vulnerability include:
- Length of the intracranial course
- Proximity to possible compression sites
- Structural vulnerabilities along their paths
Knowing these factors helps doctors diagnose and treat nerve problems and related disorders.
Clinical Assessment of Eye Movement Nerves
To check the health of the oculomotor, trochlear, and abducens nerves, a detailed clinical assessment is key. This step is vital for diagnosing and treating disorders linked to these nerves.
Cardinal Positions of Gaze Testing
Testing the cardinal positions of gaze is a basic step in assessing these nerves. It involves asking the patient to look in various directions. This helps check the function of the extraocular muscles controlled by these nerves.
Key aspects of cardinal positions of gaze testing include:
- Evaluating the range of motion in each eye
- Assessing for any nystagmus or saccadic movements
- Identifying any weakness or paralysis of the extraocular muscles
Pupillary Light Reflex Examination
The pupillary light reflex examination is also a key part of the assessment. It involves shining a light into the patient’s eyes to see how their pupils react. The oculomotor nerve controls the pupils, so any odd reactions can point to nerve problems.
Diagnostic Imaging Techniques
Diagnostic imaging, like MRI and CT scans, is also important. These tools help spot any structural issues or lesions that might be affecting the nerves.
Imaging Modality | Advantages | Limitations |
MRI | High-resolution images of soft tissues, excellent for visualizing nerve anatomy | Contraindicated in patients with certain metal implants, claustrophobia |
CT Scan | Quick and widely available, good for detecting bony abnormalities | Less detailed for soft tissues, radiation exposure |
By combining the results of cardinal positions of gaze testing, pupillary light reflex examination, and diagnostic imaging, we can fully assess the oculomotor, trochlear, and abducens nerves.
Disorders of the Oculomotor, Trochlear, and Abducens Nerves
It’s important to know about the disorders of the oculomotor, trochlear, and abducens nerves. These nerves help control our eye movements. When they don’t work right, it can cause double vision and other vision problems.
These nerve disorders can lead to different eye movement problems. We’ll look at each nerve’s specific issues. This will help us understand their symptoms and what they mean for our health.
Oculomotor Nerve Palsy
Oculomotor nerve palsy, or third nerve palsy, affects the oculomotor nerve (CN III). It can be caused by diabetes, injuries, or aneurysms. Symptoms include:
- Ptosis (drooping eyelid)
- Dilated pupil
- Outward deviation of the eye (exotropia)
- Diplopia (double vision)
Diagnosis involves a detailed eye exam and imaging tests to find the cause.
Trochlear Nerve Palsy
Trochlear nerve palsy affects the trochlear nerve (CN IV), which controls the superior oblique muscle. This can cause:
- Vertical diplopia
- Head tilt to compensate for the diplopia
- Difficulty looking downward
The diagnosis involves checking eye movements and tests to find the affected muscle.
Abducens Nerve Palsy
Abducens nerve palsy affects the abducens nerve (CN VI), which controls the lateral rectus muscle. Symptoms include:
- Horizontal diplopia
- Esotropia (inward deviation of the eye)
- Difficulty abducting the eye
Management involves treating the cause. It may include prism glasses or other treatments to fix double vision.
Ocular Motility Dysfunction and Diplopia
The eyes move in a complex way, controlled by three nerves. When these nerves get disrupted, it can cause problems with eye movement. This leads to ocular motility dysfunction and diplopia.
Pathophysiology of Diplopia
Diplopia, or double vision, happens when the eyes can’t align right. This makes us see two images of one thing. It’s caused by issues with the nerves that control eye movement.
Nerve Damage and Diplopia: Damage to these nerves can weaken or paralyze the muscles that move the eyes. For example, damage to the oculomotor nerve can make it hard to move the eye in different directions.
Differentiating Nerve-Specific Diplopia Patterns
It’s important to know the different types of diplopia caused by nerve damage. Each nerve controls different muscles, leading to unique double vision patterns.
Nerve | Primary Function | Diplopia Pattern |
Oculomotor (CN III) | Controls most extraocular muscles | Horizontal and vertical diplopia |
Trochlear (CN IV) | Innervates superior oblique muscle | Vertical diplopia, worse on downward gaze |
Abducens (CN VI) | Controls lateral rectus muscle | Horizontal diplopia, worse on lateral gaze |
Compensatory Mechanisms and Adaptations
People with eye movement problems often find ways to cope. They might tilt their head or use special lenses to fix double vision.
“The ability of patients to adapt to diplopia varies widely, with some individuals developing remarkable compensatory strategies to maintain functional vision.”
— Clinical Observations in Neuro-Ophthalmology
It’s key to understand these coping strategies. This helps doctors find the right treatment for patients with eye movement issues.
Treatment Approaches for Eye Movement Disorders
Treating eye movement disorders requires different strategies. These range from simple management to surgery. The right treatment depends on the disorder’s cause, its severity, and the patient’s health.
Conservative Management
Conservative management is often the first step. It includes:
- Eye exercises to improve eye movement
- Prism lenses to fix double vision
- Patching therapy to reduce double vision
- Watching and monitoring the disorder’s progress
Experts say, “Conservative management works well for mild to moderate disorders. It improves patients’ quality of life.”
“The goal of conservative management is to ease symptoms and improve eye alignment without surgery.”
Medical Expert, Ophthalmologist
Medical Interventions
When conservative methods fail, medical treatments are needed. These include:
- Botox injections to relax muscles
- Medications for conditions like myasthenia gravis
- Corticosteroids to reduce inflammation
A study in the Journal of Neuro-Ophthalmology showed Botox injections help some eye disorders. They provide significant symptom relief.
Surgical Corrections and Rehabilitation
When other treatments don’t work, surgery might be needed. Surgical options include:
Surgical Procedure | Indications | Benefits |
Strabismus surgery | Corrects eye misalignment | Improves eye alignment, reduces double vision |
Extraocular muscle surgery | Addresses muscle weakness or paralysis | Restores normal eye movement, improves binocular vision |
Rehabilitation is key in recovery. It helps patients adjust and use their vision better. “Surgery, with the right rehabilitation, greatly improves outcomes for eye movement disorders,” a top ophthalmologist says.
Conclusion
We’ve looked into the oculomotor, trochlear, and abducens nerves. They are key for eye movement control. These nerves help us move our eyes and see the world around us.
These nerves work together for smooth eye movements. Knowing how they function is important. It helps doctors diagnose and treat eye movement problems.
Doctors use their knowledge of these nerves to diagnose and treat eye issues. They look for signs of nerve problems to give the right treatment.
In short, these nerves are vital for our vision. Their importance in healthcare is huge. More research will help patients and improve our understanding of eye movement.
FAQ
What is the oculomotor nerve responsible for?
The oculomotor nerve, also known as the third cranial nerve (CN III), controls eye movements. It works with four extraocular muscles. It also helps with pupillary constriction and near vision.
What is the function of the trochlear nerve?
The trochlear nerve, or the fourth cranial nerve (CN IV), controls the superior oblique muscle. This muscle is key for downward and inward eye movement. It helps with eye movement coordination.
What does the abducens nerve control?
The abducens nerve, or the sixth cranial nerve (CN VI), controls the lateral rectus muscle. This muscle is responsible for the eye’s outward movement.
How do the oculomotor, trochlear, and abducens nerves work together?
These nerves work together for eye movements. The oculomotor nerve controls several muscles and pupillary constriction. The trochlear nerve controls the superior oblique muscle. The abducens nerve controls the lateral rectus muscle. Together, they enable precise eye movements.
What are the clinical implications of damage to these nerves?
Damage to these nerves can cause oculomotor, trochlear, or abducens nerve palsy. Symptoms include diplopia (double vision) and eye movement problems.
How are disorders of the oculomotor, trochlear, and abducens nerves diagnosed?
Diagnosis involves clinical assessment and testing. It includes examining the pupillary light reflex and using imaging techniques. This helps evaluate the nerves and their functions.
What are the treatment approaches for eye movement disorders caused by these nerves?
Treatment includes conservative management and medical interventions. Surgical corrections are also used. The goal is to manage the condition, alleviate symptoms, and improve outcomes.
What is the significance of understanding the anatomy and function of the oculomotor, trochlear, and abducens nerves?
Knowing about these nerves is key for diagnosing and treating disorders. It helps in controlling eye movements and visual processing.
Which cranial nerves are responsible for controlling eye movements?
The oculomotor (CN III), trochlear (CN IV), and abducens (CN VI) nerves control eye movements.
What is the role of the oculomotor nerve in pupillary constriction?
The oculomotor nerve is vital for pupillary constriction. It innervates the sphincter pupillae muscle. This muscle controls the pupil’s constriction in response to light.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK54102/

































