Cranial nerve 3, or the oculomotor nerve (CN III), is key for most eye movements. Damage to it can lead to eye movement paralysis, known as oculomotor nerve palsy. We’ll look into CN III’s important roles and symptoms when it’s harmed. Our best guide to the cranial nerves responsible for eye movement (CN III, IV, VI). Learn their amazing, critical jobs.
The oculomotor nerve controls four of the six eye muscles and the levator palpebrae superioris. Knowing about CN III’s anatomy and functions helps in diagnosing and treating related issues.
Key Takeaways
- Cranial nerve 3, or the oculomotor nerve, controls most eye movements.
- Damage to CN III can cause complete paralysis of eye movement.
- Oculomotor nerve palsy can be congenital or acquired.
- CN III innervates four extraocular muscles and the levator palpebrae superioris.
- Understanding CN III’s functions is key for diagnosis and management.
Understanding Cranial Nerve 3: The Oculomotor Nerve

Learning about the oculomotor nerve, or CN III, helps us understand how our eyes move. This nerve is the third cranial nerve. It’s key in controlling our eye movements.
Definition and Basic Functions
The oculomotor nerve, or CN III, is a complex nerve. It controls several muscles that move our eyes. It also helps our eyelid lift and controls how our pupils and lenses adjust for close-up vision.
Location and Origin in the Brain
The oculomotor nerve starts in the midbrain of the brainstem. It comes out from the front of the midbrain. Knowing where it starts and ends is important for treating nerve problems.
Characteristics | Description |
Origin | Oculomotor nucleus in the midbrain |
Function | Controls 4 extraocular muscles, levator palpebrae superioris, and provides parasympathetic innervation to the pupil and lens |
Location | Emerges between posterior cerebral artery and superior cerebellar artery |
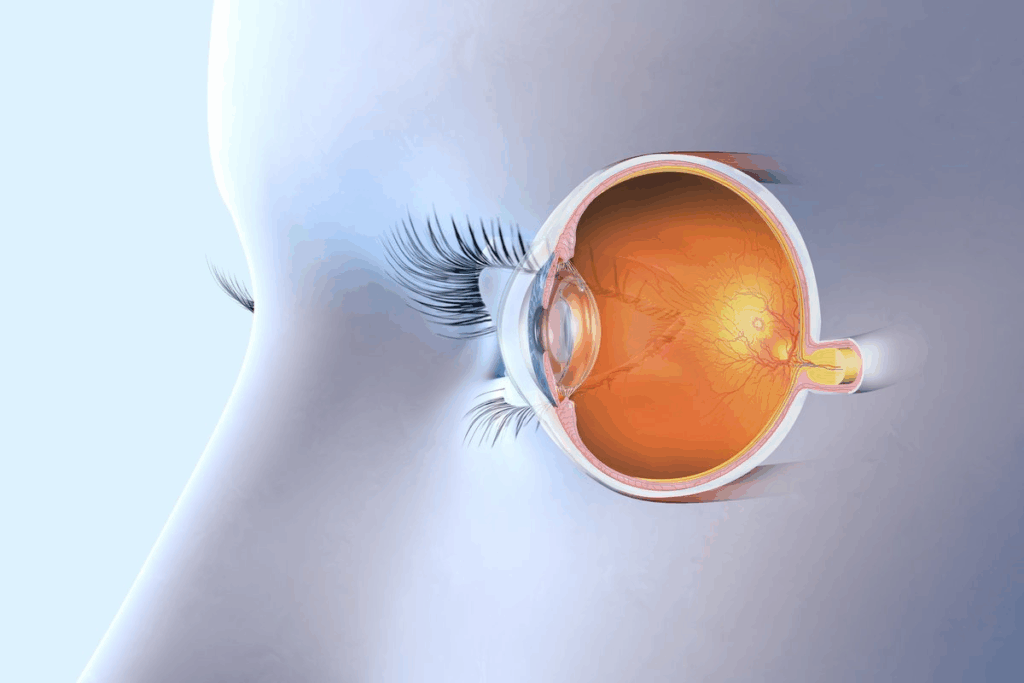
Anatomy of the Oculomotor Nerve
The oculomotor nerve’s anatomy is complex. It involves many nuclei and pathways that control eye movements. Knowing this complexity helps us understand how the nerve works and how damage can cause problems.
Nuclei and Brainstem Connections
The oculomotor nerve starts from several nuclei in the brainstem. The oculomotor nucleus and the Edinger-Westphal nucleus handle its motor and parasympathetic functions. The oculomotor nucleus is in the midbrain. Its connections with other brainstem nuclei are key for smooth eye movements.
Course Through the Skull
The nerve begins in the brainstem and travels through the subarachnoid space. It goes between the superior cerebellar artery and the posterior cerebral artery. Then, it moves forward through the cavernous sinus and enters the orbit through the superior orbital fissure.
Branches and Innervation Patterns
Once in the orbit, the oculomotor nerve splits into superior and inferior branches. The superior branch controls the superior rectus and levator palpebrae superioris muscles. The inferior branch controls the medial, inferior rectus, and inferior oblique muscles. This pattern is vital for precise eye movement control.
The detailed anatomy of the oculomotor nerve is key. It shows how the nerve controls eye movements and what happens when it’s damaged.
Cranial Nerves Responsible for Eye Movement: The Complete Picture
Eye movements are controlled by three cranial nerves working together. It’s important to know how CN III, CN IV, and CN VI work together. This knowledge helps in diagnosing and treating eye movement problems.
CN III: The Oculomotor Nerve
The oculomotor nerve, or CN III, controls several muscles for eye movement. It helps the medial rectus, superior rectus, inferior rectus, and inferior oblique muscles. These muscles help the eye move in different ways, like moving it up, down, and side to side.
CN IV: The Trochlear Nerve
The trochlear nerve, or CN IV, is the thinnest cranial nerve. It controls the superior oblique muscle. This muscle helps rotate the eye and also aids in moving it down and out. The trochlear nerve is key for smooth eye movements, mainly when looking down.
CN VI: The Abducens Nerve
The abducens nerve, or CN VI, controls the lateral rectus muscle. This muscle is responsible for moving the eye outward. It’s important for moving the eye side to side and helps with overall eye movement coordination.
These three cranial nerves work together for normal eye movement. Any problem with these nerves can cause eye movement disorders. These disorders can include double vision or crossed eyes.
Cranial Nerve | Muscle Innervated | Primary Function |
CN III (Oculomotor) | Medial Rectus, Superior Rectus, Inferior Rectus, Inferior Oblique | Adduction, Elevation, Depression, Rotation |
CN IV (Trochlear) | Superior Oblique | Intorsion, Depression, Abduction |
CN VI (Abducens) | Lateral Rectus | Abduction |
Functions of Cranial Nerve 3
Knowing what Cranial Nerve 3 does is key for treating eye problems. This nerve, also known as the oculomotor nerve, handles important eye tasks.
Motor Functions: Controlling Extraocular Muscles
The oculomotor nerve controls several muscles that help us move our eyes. Four of the six extraocular muscles are controlled by CN III. These muscles help us move our eyes in different ways.
“The precise control of eye movements is a complex process that involves the coordinated action of multiple cranial nerves,” as noted by experts in the field of neuro-ophthalmology.
Parasympathetic Functions: Pupil and Lens Control
CN III also controls the muscles that make our pupils smaller and our lens focus better. This is important for letting the right amount of light in and for seeing things up close.
This dual function is key for controlling light and focusing on objects at different distances.
Role in Coordinated Eye Movements
Cranial Nerve 3 is essential for coordinated eye movements. These movements are needed for activities like reading and driving. The oculomotor nerve works with other nerves to make sure both eyes move together.
As highlighted by a study on oculomotor control, “the harmonious functioning of these nerves is critical for preventing diplopia and ensuring clear vision.”
Oculomotor Nerve Palsy: Definition and Types
To understand oculomotor nerve palsy, we need to know its types and how it affects us. It’s also known as third nerve palsy. This nerve controls how our eyes move.
There are different kinds of oculomotor nerve palsy. They are based on how much damage there is and if the pupil is affected. The main types are complete and partial palsy, and whether the pupil is involved or not.
Complete vs. Partial Third Nerve Palsy
Complete third nerve palsy has severe symptoms. These include ptosis (drooping eyelid), eye misalignment, and a big pupil. On the other hand, partial third nerve palsy has milder symptoms. This depends on how much damage there is.
- Complete palsy causes big problems with vision.
- Partial palsy is harder to spot because its symptoms are not as clear.
Pupil-Involving vs. Pupil-Sparing Palsy
There’s also a difference between pupil-involving and pupil-sparing oculomotor nerve palsy. Pupil-involving palsy is usually caused by serious things like an aneurysm. Pupil-sparing palsy is often due to less serious issues, like diabetes or hypertension.
Knowing if the pupil is involved helps doctors figure out what’s wrong. If it is, it might mean the nerve is being squeezed by something, like an aneurysm. If it’s not, it could mean the nerve is just not getting enough blood.
It’s important to know the difference to get the right treatment. Doctors use tests and scans to find out what’s causing the problem. This helps them decide how to help you.
Causes of Cranial Nerve 3 Damage
Understanding why Cranial Nerve 3 gets damaged is key to treating it. Many things can harm this nerve. Knowing what causes the damage helps doctors find the right treatment.
Vascular Causes: Aneurysms and Diabetes
Vascular problems are a big reason for Cranial Nerve 3 damage. Aneurysms from the posterior communicating artery can press on the nerve. Diabetes is another cause, leading to diabetic third nerve palsy.
Diabetic third nerve palsy often hurts and makes it hard to move the eye. But it usually doesn’t affect the pupil. It’s thought to be caused by tiny blood vessel problems in the nerve.
Vascular Cause | Characteristics |
Aneurysms | Compression of CN III, potentially causing complete palsy |
Diabetes | Microvascular ischemia, often sparing the pupil |
Traumatic Injuries to the Head and Orbit
Head and orbital trauma are common causes of Cranial Nerve 3 damage. Head injuries can directly harm the nerve. Orbital trauma, with fractures or swelling, can also affect it.
The damage from trauma can vary. Sometimes, the nerve is stretched or compressed, causing temporary or permanent problems.
Compressive Lesions: Tumors and Mass Effects
Tumors and other mass effects can also harm Cranial Nerve 3. Tumors in the brainstem, cavernous sinus, or orbit can press on the nerve. This can cause different levels of palsy.
The symptoms depend on where and how big the lesion is. Finding it early is important to avoid more damage and improve treatment results.
Inflammatory and Infectious Causes
Inflammatory and infectious diseases can also harm Cranial Nerve 3. Conditions like multiple sclerosis, sarcoidosis, and meningitis can affect the nerve. So can infections like Lyme disease and syphilis.
Diagnosing these causes involves clinical checks, lab tests, and imaging. It’s a team effort to figure out what’s wrong.
Clinical Presentation and Symptoms
Understanding oculomotor nerve palsy is key for correct diagnosis and treatment. The symptoms can greatly affect a person’s life, impacting their vision and overall health.
Ptosis (Drooping Eyelid)
Ptosis, or drooping eyelid, is a major symptom of oculomotor nerve palsy. It happens because the levator palpebrae superioris muscle is weak or paralyzed. This muscle lifts the eyelid. The severity of ptosis can range from mild to severe, where the eyelid almost closes.
Diplopia (Double Vision)
Diplopia, or double vision, is common in oculomotor nerve palsy. It’s caused by the extraocular muscles not working together right. This makes people see two images instead of one, which is very hard to deal with. The direction of the double vision can help figure out which nerve or muscle is affected.
Mydriasis (Pupil Dilation)
Mydriasis, or pupil dilation, is another symptom of oculomotor nerve palsy. The oculomotor nerve helps control the pupil’s size. Damage to this nerve means the pupil can’t get smaller, leading to a bigger pupil on the affected side.
Eye Misalignment and “Down and Out” Position
The eye on the affected side often looks “down and out” because of the other muscles’ action. This causes eye misalignment, where the eyes don’t line up right. This makes diplopia worse.
Spotting these symptoms is vital for diagnosing oculomotor nerve palsy and starting the right treatment. We’ll look at how to diagnose it next.
Diagnosing Oculomotor Nerve Palsy
To find out if someone has oculomotor nerve palsy, doctors use many tools. They do clinical exams and use advanced imaging. This helps them find the cause and plan the best treatment.
Clinical Examination Techniques
Checking the eyes is key to diagnosing oculomotor nerve palsy. Doctors look at how the eyes move, how pupils react, and eyelid position. They use:
- Evaluation of extraocular muscle function
- Assessment of pupil size and reactivity
- Examination of eyelid position and movement
These steps help doctors see how bad the nerve problem is. They then decide what tests to do next.
Neuroimaging Studies: MRI, CT, and Angiography
Imaging is very important for diagnosing oculomotor nerve palsy. It helps find things like aneurysms or tumors. Doctors use:
Imaging Modality | Primary Use | Key Benefits |
MRI | Soft tissue evaluation | High-resolution images of brain structures |
CT Angiography | Vascular assessment | Detailed visualization of blood vessels |
CT Scan | Initial assessment of head trauma or acute hemorrhage | Rapid imaging in emergency situations |
Laboratory Tests and Other Diagnostic Procedures
Doctors also do blood tests to help diagnose oculomotor nerve palsy. They check for things like diabetes or infections. Tests might include:
- Blood glucose tests
- Infectious disease screening
- Inflammatory marker tests
By looking at all the results, doctors can accurately diagnose oculomotor nerve palsy. Then, they can make a good treatment plan.
Differential Diagnosis: Distinguishing Third Nerve Palsy
When a patient might have third nerve palsy, doctors need to look at other possible causes. This is key to giving the right treatment.
Other Cranial Nerve Palsies
Other nerve palsies can look like third nerve palsy. Trochlear nerve palsy (CN IV) and abducens nerve palsy (CN VI) are two to consider.
Trochlear nerve palsy affects the superior oblique muscle. This makes it hard to move the eye down and in. Abducens nerve palsy, on the other hand, affects the lateral rectus muscle. It makes it hard to move the eye out.
Cranial Nerve Palsy | Affected Muscle | Primary Symptom |
Third Nerve Palsy (CN III) | Multiple extraocular muscles | Ptosis, diplopia, pupil dilation |
Trochlear Nerve Palsy (CN IV) | Superior oblique | Difficulty with downward and inward gaze |
Abducens Nerve Palsy (CN VI) | Lateral rectus | Impaired outward eye movement |
Myasthenia Gravis and Other Neuromuscular Disorders
Myasthenia gravis is an autoimmune disorder that can look like third nerve palsy. It causes symptoms like ptosis and diplopia. Other conditions, like muscular dystrophy and thyroid eye disease, can also cause similar eye problems.
To tell these conditions apart, doctors need to do a detailed check-up. Sometimes, they might need to do tests like electromyography or blood tests for antibodies.
Getting the right diagnosis is very important. It helps doctors treat third nerve palsy and other related conditions better. By looking at all possible causes, doctors can give better care.
Treatment Approaches for Third Nerve Palsy
Managing third nerve palsy needs a detailed plan. It focuses on the cause and easing symptoms. The condition affects eye movement and other functions, so a custom treatment is key.
Medical Management of Underlying Causes
The first step is to find and treat the cause. Vascular causes like diabetes and high blood pressure are managed by controlling them. For example, keeping blood sugar in check can help symptoms and prevent nerve damage.
An aneurysm might need quick medical or surgery to avoid more problems. Infections or inflammation might need antibiotics or anti-inflammatory drugs.
Surgical Interventions: Strabismus Surgery and Ptosis Repair
Significant strabismus or ptosis might need surgery. Strabismus surgery corrects eye alignment by adjusting muscles. Ptosis repair lifts the eyelid by tightening the levator muscle.
These surgeries can greatly improve eye and eyelid alignment. They also enhance appearance and function.
Supportive Therapies: Patching, Prisms, and Botulinum Toxin
Supportive therapies also play a role. Patching one eye can stop diplopia. Prisms in glasses help align vision.
Botulinum toxin injections can weaken muscles, reducing strabismus. These treatments work together for full care.
By using medical, surgical, and supportive therapies, we can manage third nerve palsy well. This improves life quality for those affected.
Conclusion: Living with Oculomotor Nerve Dysfunction
Understanding oculomotor nerve dysfunction is key to managing it and improving life quality. Patients with this condition often need ongoing care and support. This helps address symptoms and related issues.
Living with third nerve palsy comes with challenges like ptosis, diplopia, and mydriasis. A good management plan includes medical, surgical, and supportive therapies. These are tailored to meet each person’s needs.
By tackling oculomotor nerve dysfunction with a detailed treatment plan, people can manage it better. Our healthcare team is dedicated to providing top-notch care and support to patients worldwide. We aim to help them manage their condition effectively.
FAQ
What is cranial nerve 3, and what are its primary functions?
Cranial nerve 3, also known as the oculomotor nerve, controls four extraocular muscles. These include the superior rectus, medial rectus, inferior rectus, and inferior oblique muscles. It also controls the levator palpebrae superioris muscle, which lifts the upper eyelid.
What is oculomotor nerve palsy, and what are its types?
Oculomotor nerve palsy is when the oculomotor nerve is paralyzed or weak. This leads to eye movement disorders. There are different types, like complete and partial third nerve palsy, and pupil-involving and pupil-sparing palsy.
What are the causes of damage to cranial nerve 3?
Damage to cranial nerve 3 can be caused by several factors. These include vascular issues like aneurysms and diabetes. Traumatic injuries to the head and orbit are also causes. Other causes include compressive lesions like tumors and mass effects, and inflammatory and infectious causes.
What are the symptoms of oculomotor nerve palsy?
Symptoms of oculomotor nerve palsy include ptosis (drooping eyelid) and diplopia (double vision). Mydriasis (pupil dilation) and eye misalignment are also symptoms. This often results in a “down and out” position of the eye.
How is oculomotor nerve palsy diagnosed?
Diagnosing oculomotor nerve palsy involves several steps. Clinical examination techniques are used. Neuroimaging studies like MRI, CT, and angiography are also used. Laboratory tests help determine the underlying cause.
What is the differential diagnosis for third nerve palsy?
When diagnosing third nerve palsy, other cranial nerve palsies are considered. This includes CN IV and CN VI. Myasthenia gravis and other neuromuscular disorders are also considered.
What are the treatment approaches for third nerve palsy?
Treatment for third nerve palsy varies. Medical management of underlying causes is used. Surgical interventions like strabismus surgery and ptosis repair are also options. Supportive therapies include patching, prisms, and botulinum toxin.
Can damage to cranial nerve 3 be recovered?
Recovery from damage to cranial nerve 3 depends on the cause and extent of damage. In some cases, the nerve can recover on its own. In others, treatment may be needed to manage the condition.
How does cranial nerve 3 damage affect eye movement?
Damage to cranial nerve 3 can impair eye movement. This leads to symptoms like diplopia and eye misalignment. The nerve’s role in controlling extraocular muscles is key.
References
National Center for Biotechnology Information. Oculomotor Nerve: Function and Consequences of Palsy. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK538321/