The abducens nerve, also known as the 6th cranial nerve, is key in eye movement control. We’ll dive into its role and why it’s important for diagnosing eye problems.An essential guide to abducens cranial nerve function. Learn what this critical motor nerve does and how it controls your eye movement.
This nerve is a motor nerve, focusing on the lateral rectus muscle. It helps move the eye sideways. Knowing this is vital for doctors to treat eye movement issues well.
It’s important for both doctors and patients to understand CN VI’s role. This helps spot signs of nerve problems and find the right treatment.
Key Takeaways
- The abducens nerve is a purely motor nerve.
- It innervates the lateral rectus muscle, enabling lateral eye movement.
- Understanding CN VI function is vital for diagnosing eye movement disorders.
- CN VI dysfunction can lead to significant eye movement issues.
- Accurate diagnosis is essential for effective management of related disorders.
The Abducens Nerve: A Fundamental Overview
Understanding the abducens nerve is key to knowing how our eyes move. The abducens nerve, also known as cranial nerve VI (CN VI), is a special nerve. It helps control how our eyes move.
Definition and Basic Classification
The abducens nerve is the sixth cranial nerve. It is a motor nerve, meaning it only controls muscles. It works with the lateral rectus muscle to help our eyes move outward.
Historical Context and Naming
For centuries, the abducens nerve has been studied in medicine. It was named based on its function and where it is located among cranial nerves. The name “abducens” comes from the Latin word for “to draw away,” showing its role in eye movement.
Significance in Ocular Motility
The abducens nerve is vital for eye movement. It helps our eyes move laterally, which is important for tracking and reading. This nerve is key for coordinated eye movements.
Cranial Nerve | Primary Function | Muscle Innervated |
CN III (Oculomotor) | Multiple eye movements | Medial rectus, superior rectus, inferior rectus, inferior oblique |
CN IV (Trochlear) | Superior oblique muscle control | Superior oblique |
CN VI (Abducens) | Lateral rectus muscle control | Lateral rectus |
This table shows how different cranial nerves control eye movements. It highlights the abducens nerve’s role in eye movement.
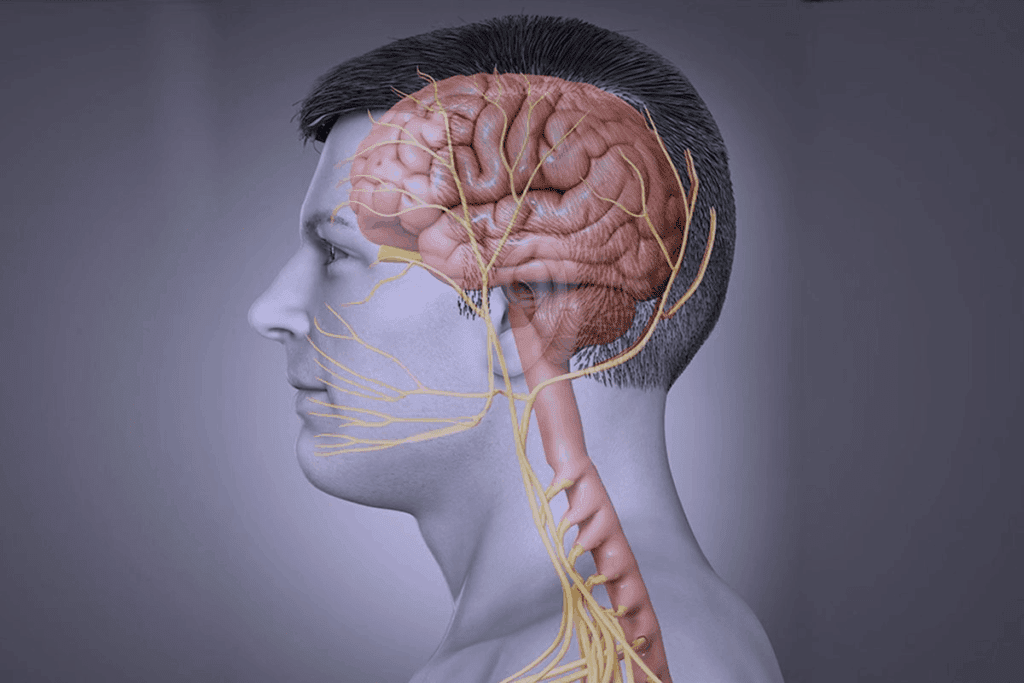
Anatomy of the Abducens Nerve (CN VI)
The Abducens nerve has a unique path inside the brain. It is the sixth cranial nerve and controls eye movements. Knowing its anatomy helps us understand its importance.
Origin and Nucleus Location in the Dorsal Pons
The Abducens nerve starts from the Abducens nucleus in the dorsal pons. This nucleus controls the lateral rectus muscle, which CN VI innervates. The nucleus is surrounded by important neural structures, including the facial colliculus.
The Abducens nucleus gets signals from the medial longitudinal fasciculus. This helps coordinate eye movements. This complex interaction ensures the lateral rectus muscle works well.
Detailed Intracranial Pathway
After starting, CN VI exits the brainstem at the pons and medulla junction. It then goes into the subarachnoid space, moving up the pons base. The nerve pierces the dura mater to enter Dorello’s canal, a key landmark.
- The nerve goes through the subarachnoid space, where it can be compressed by nearby structures.
- It then goes through Dorello’s canal, a narrow passage that can cause problems.
- Next, it reaches the cavernous sinus.
Cavernous Sinus Traversal
CN VI goes through the cavernous sinus, a venous area near the sphenoid sinus. Inside, it’s close to the internal carotid artery, which can press on it.
The cavernous sinus is a complex area with many important structures. It contains nerves III, IV, V1, V2, and VI. This close relationship means problems here can affect multiple nerves.
Orbital Entry and Terminal Branches
After leaving the cavernous sinus, CN VI enters the orbit through the superior orbital fissure. Inside, it innervates the lateral rectus muscle, which moves the eye outward.
The nerve’s final branches are key for eye movement control. Damage here can cause Abducens nerve palsy, leading to eye movement issues.
Abducens Cranial Nerve Function: Motor Control Explained
The abducens nerve helps us move our eyes by controlling the lateral rectus muscle. This is key for moving our eyes to the side. It lets us track objects or change our gaze.
Primary Function: Lateral Rectus Innervation
The abducens nerve works with the lateral rectus muscle. This muscle is one of six around the eyeball. It helps the eyeball move outward, away from the face’s center.
Eye Abduction Mechanics
Eye abduction is a complex process. The abducens nerve and the lateral rectus muscle work together. When the nerve is active, the muscle contracts, moving the eyeball outward.
Role in Conjugate Gaze
The abducens nerve is vital for conjugate gaze. This means moving both eyes in the same direction. It works with other nerves to ensure both eyes move together, keeping our vision aligned.
Neurophysiology of Abduction
Abduction happens through signals from the abducens nucleus to the lateral rectus muscle. The abducens nerve sends motor fibers to control the muscle. This allows for smooth eye movements, helping us track objects or read.
Key aspects of the abducens nerve’s function include:
- Innervation of the lateral rectus muscle
- Control of eye abduction
- Coordination with other cranial nerves for conjugate gaze
- Transmission of motor signals for precise eye movements
Motor vs. Sensory: Why CN VI Is Purely Motor
Cranial nerves have different roles, but the abducens nerve is unique. It is purely motor, which is key for eye movement control. Let’s dive into why it’s classified this way and what it means.
Classification of Cranial Nerve Fibers
Cranial nerves are sorted by their fiber types. These include motor, sensory, and autonomic fibers. The abducens nerve is all about motor function.
Understanding cranial nerve fibers is important. Motor fibers send signals to muscles. Sensory fibers receive and send sensory info. The abducens nerve has general somatic efferent fibers for motor control.
General Somatic Efferent Fibers of CN VI
The abducens nerve only has fibers for the lateral rectus muscle. This lets it control eye movements with precision.
A neuroanatomist noted, “The abducens nerve controls the lateral rectus muscle alone.” This shows its unique role.
“The abducens nerve is a prime example of a cranial nerve with a single, dedicated function – the control of the lateral rectus muscle.”
Comparison with Mixed Cranial Nerves
The abducens nerve is different from nerves with both motor and sensory roles. For instance, the trigeminal nerve (CN V) has both, but the abducens is only motor.
Cranial Nerve | Motor Function | Sensory Function |
Abducens Nerve (CN VI) | Yes | No |
Trigeminal Nerve (CN V) | Yes | Yes |
Facial Nerve (CN VII) | Yes | Yes |
Absence of Sensory Components
The abducens nerve doesn’t have sensory parts. This makes it different from many other nerves. It’s focused on controlling the lateral rectus muscle.
Its lack of sensory fibers highlights its specialized function. This is key for precise eye movement control.
The Medial Longitudinal Fasciculus Connection
Understanding how the abducens nerve works with the medial longitudinal fasciculus is key. The medial longitudinal fasciculus (MLF) is a brainstem structure. It helps coordinate eye movements by linking cranial nerve nuclei.
Neuroanatomical Relationships
The abducens nerve, or CN VI, is closely linked to the MLF. This link is vital for eye movement coordination. The MLF is like a highway for signals between eye movement nuclei, making sure both eyes move together.
Coordination of Bilateral Eye Movements
Eye movement coordination is complex, needing precise nerve communication. The abducens nerve is key, controlling the lateral rectus muscle for outward gaze. The MLF ensures these signals are sent correctly for synchronized eye movements.
Contralateral Projections to Medial Rectus
About forty percent of the abducens nerve’s axons go to the contralateral medial rectus muscle through the MLF. This is essential for coordinated eye movement. The medial rectus muscle, controlled by CN III, works with the lateral rectus to move eyes together.
Internuclear Ophthalmoplegia Implications
Internuclear ophthalmoplegia (INO) happens when the MLF is damaged. It causes eye movement problems during horizontal gaze and nystagmus in the moving eye. Knowing how the MLF and abducens nerve work helps diagnose and treat INO, showing their critical role in eye movement.
Clinical Examination of the Abducens Nerve
Checking the abducens nerve is key to understanding eye movement problems. We look at how it works, focusing on its role in moving the eyes sideways.
Assessment Techniques
We check the abducens nerve with the oculomotor and trochlear nerves. We test eye movements. Assessment techniques include seeing if the patient can follow a target with their eyes. We also check for eye alignment and any eye movement issues.
The test starts with a vision check. Then, we look at how the eyes move in different directions. We see if the patient can keep their eyes on a target and check for double vision.
Normal and Abnormal Findings
Normal results show the eyes moving freely and staying aligned. Abnormal findings might mean the abducens nerve is not working right. This could cause the eye to turn inward or have trouble moving outward.
Differential Diagnosis Considerations
If we find something off, we think about what could be wrong. This might include abducens nerve palsy, thyroid eye disease, or myasthenia gravis. We need more tests, like imaging, to figure out the cause.
Documentation and Reporting
It’s important to write down what we find during the exam. We record the patient’s symptoms and the results of the eye tests. This helps us decide what to do next for the patient.
Abducens Nerve Palsy: Causes, Symptoms, and Management
The abducens nerve, or CN VI, controls eye movements. When it doesn’t work right, it can cause weakness or paralysis of the lateral rectus muscle. This is known as abducens nerve palsy.
Etiology of Abducens Nerve Dysfunction
Abducens nerve palsy can be caused by many things. Vascular causes include diabetic neuropathy, which damages the nerve. Traumatic injuries can also harm the nerve, like skull fractures or high pressure inside the skull.
Other causes include thrombophlebitis of the cavernous sinus and space-occupying lesions like tumors or aneurysms. These can press on the nerve. Knowing the cause helps decide how to treat it.
Clinical Presentation and Diagnostic Criteria
People with abducens nerve palsy often see double vision, worse when looking to the side of the problem. Doctors diagnose based on the patient’s history and physical exam, checking eye movements and alignment.
They look for esotropia, an inward eye deviation, and limited eye movement. More tests might be needed to find the cause.
Imaging and Laboratory Investigations
Imaging studies like MRI or CT scans are used to find the cause. They can spot tumors or aneurysms pressing on the nerve.
Laboratory tests check for diabetes or other conditions. Blood glucose tests can spot diabetic neuropathy.
Treatment Options and Prognosis
Treatment depends on the cause. For idiopathic or microvascular causes, managing risk factors like diabetes is key.
If it’s due to a compressive lesion, surgical intervention might be needed. The outcome varies, with some cases getting better on their own and others needing ongoing care.
Relationship with Other Ocular Motor Nerves
The abducens nerve is part of a complex system. It works with CN III and CN IV to control eye movements. This system helps us track objects, read, and do daily activities.
Functional Integration with CN III and CN IV
The abducens nerve (CN VI) works with CN III and CN IV. CN VI controls the lateral rectus muscle. CN III controls most extraocular muscles. CN IV controls the superior oblique muscle.
Together, these nerves help us move our eyes in many ways. They make small adjustments and big saccades possible.
For example, when we look right, the right lateral rectus and the left medial rectus muscles work together. This is because of complex connections in the brainstem.
Comparative Anatomy and Function
CN III, CN IV, and CN VI are all cranial nerves. They come from the brainstem and control extraocular muscles. But, they differ in their anatomy and function.
CN III controls several muscles and the eyelid. CN IV is simpler, controlling only the superior oblique muscle. CN VI controls the lateral rectus muscle.
Synergistic Actions in Eye Movement
CN III, CN IV, and CN VI work together for precise eye movements. For example, looking down and laterally involves the inferior rectus and superior oblique muscles. Looking laterally involves the lateral rectus and medial rectus muscles.
These actions are possible due to complex neural circuits. Damage to these nerves can lead to impaired eye movements. This shows how important their coordination is.
Clinical Correlations of Multiple Cranial Nerve Palsies
Damage to multiple cranial nerves can cause complex symptoms. For example, palsies of CN III, CN IV, and CN VI can lead to double vision in many directions. Diagnosing these cases requires a deep understanding of the nerves and their interactions.
Identifying the cause of multiple cranial nerve palsies is key. This can be a tumor, aneurysm, or inflammation. Imaging studies like MRI or CT scans are often needed for diagnosis. Treatment depends on the cause and may involve medicine or surgery.
Conclusion: Understanding the Unique Role of the Abducens Nerve
The abducens nerve is key in controlling how our eyes move sideways. It’s a vital part of the eye movement system. Knowing about it helps doctors diagnose and treat related eye problems.
This nerve helps our eyes move outward. It works closely with other nerves to make sure our eyes move together smoothly. This is important for clear vision.
In short, the abducens nerve is very important in eye care. Doctors need to understand its role to help patients with eye movement issues. This knowledge helps them provide better care.
FAQ
Is the abducens nerve sensory or motor?
The abducens nerve, also known as CN VI, is a motor nerve. It doesn’t have sensory parts. It controls the lateral rectus muscle, which helps move the eye outward.
What is the primary function of the abducens nerve?
The main job of the abducens nerve is to control the lateral rectus muscle. This muscle helps move the eye outward.
What is the role of the abducens nerve in conjugate gaze?
The abducens nerve is key in conjugate gaze. It works with other muscles to move the eyes together.
What is the pathway of the abducens nerve?
The abducens nerve starts in the dorsal pons. It goes through the cavernous sinus and the superior orbital fissure. It ends by innervating the lateral rectus muscle.
What is the significance of the medial longitudinal fasciculus (MLF) in relation to the abducens nerve?
The MLF is vital for eye movement coordination. It connects the abducens nucleus with the oculomotor nucleus. This enables eyes to move together.
What are the clinical implications of abducens nerve palsy?
Abducens nerve palsy can cause double vision and eye deviation. It also limits eye movement outward. Quick diagnosis and treatment are needed.
How is the abducens nerve examined clinically?
Clinically, the abducens nerve is checked by looking at eye movements. It’s important to see if there’s weakness or paralysis.
What are the causes of abducens nerve dysfunction?
Dysfunction can be caused by trauma, vascular issues, tumors, and inflammation. These are just a few examples.
How does the abducens nerve interact with other ocular motor nerves?
The abducens nerve works with CN III and CN IV. Together, they control eye movements. This shows how they work together.
What is internuclear ophthalmoplegia, and how is it related to the abducens nerve?
Internuclear ophthalmoplegia is caused by MLF damage. It affects eye movement coordination. It’s linked to the abducens nerve’s role in eye movement.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK430711/





