Our brain talks to our head, neck, and body through 12 specialized nerve pairs called cranial nerves. These nerves do important jobs, like helping us see and hear. They also control how our body works.what are the 12 cranial nerves and functionsWhat Are the Symptoms and Treatments for Trigeminal Neuralgia Type 2?
At Liv Hospital, we focus on checking the brain and teaching about it. Cranial nerves are key for the brain to talk to different parts of our body.
Knowing about these nerves helps us find and treat brain problems. We have a detailed guide on cranial nerves and their jobs. It covers where they start, how they’re grouped, and why they’re important.
Key Takeaways
- Cranial nerves are 12 paired nerves that arise directly from the brain.
- They control various bodily functions, including senses and facial expressions.
- Understanding cranial nerves is essential for diagnosing neurological conditions.
- Comprehensive neurological assessment is key for good treatment.
- Liv Hospital offers care and education on cranial nerves for patients.
The Cranial Nervous System: Overview and Importance
The cranial nerves are key to understanding human anatomy and neurology. They make up 12 pairs of nerves. These nerves control many bodily functions, from sensing the world to moving our bodies.
Organization and Classification of Cranial Nerves
The cranial nerves are numbered I through XII. This helps us understand their order and types. They are sorted by their functions, which can be sensory, motor, or both.
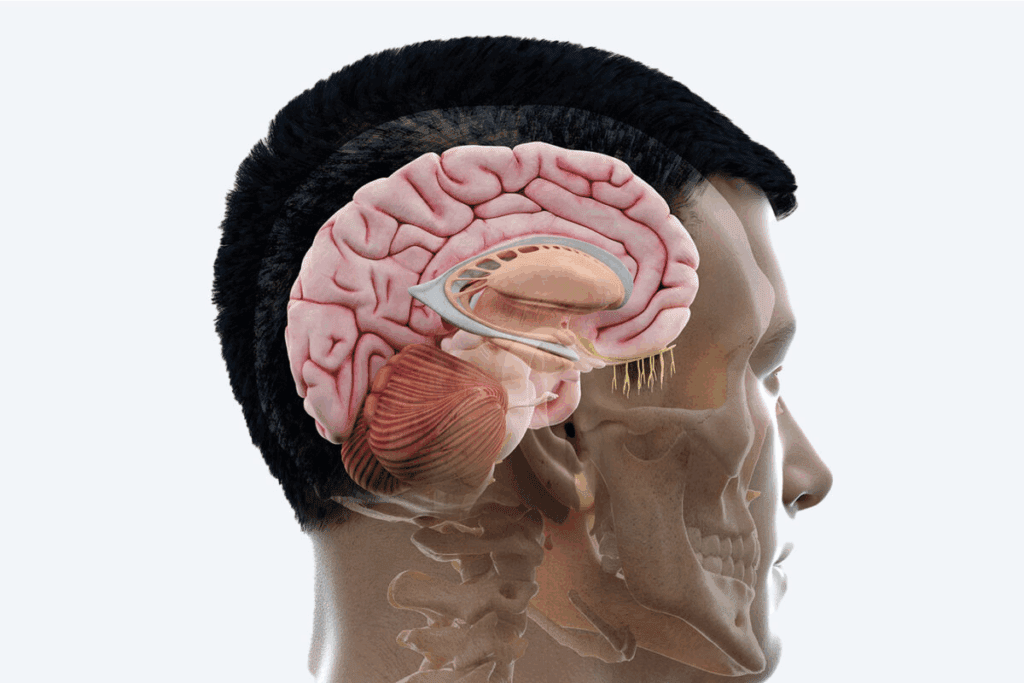
Anatomical Origins from Brain and Brainstem
The first two nerves, the olfactory and optic, start in the cerebrum. The other ten come from the brainstem. Knowing where they start is important for understanding their roles.
Functional Categories: Sensory, Motor, and Mixed
Cranial nerves fall into three groups: sensory, motor, and mixed. Sensory nerves send information to our brains. Motor nerves control our muscles. Mixed nerves do both, showing the system’s complexity.
For example, the olfactory nerve (CN I) deals with smell. The oculomotor nerve (CN III) controls eye movements. The trigeminal nerve (CN V) does both, showing the system’s complexity.
What Are the 12 Cranial Nerves and Functions

Knowing the 12 cranial nerves and their roles is key for diagnosing and treating brain disorders. These nerves come straight from the brain. They handle important tasks like sensing the world, controlling movements, and managing body functions.
Numbering System (I-XII) and Nomenclature
The 12 cranial nerves are named with Roman numerals (I-XII). This order shows how they attach to the brain from front to back. It makes it easier to remember and identify each nerve’s role. Their names reflect what they do or where they are located.
Cranial Nerve Number | Name | Primary Function |
I | Olfactory | Sensory (Smell) |
II | Optic | Sensory (Vision) |
III | Oculomotor | Motor (Eye Movement) |
XII | Hypoglossal | Motor (Tongue Movement) |
General Distribution and Pathways
The 12 cranial nerves spread out in different ways. Some are just for sensing, others for moving, and some do both. Knowing where they go is vital for finding problems.
Clinical Significance in Neurological Examination
Problems with cranial nerves can show where in the brain something is wrong. Checking these nerves is a big part of brain exams. It helps find where issues are and what they might be.
Understanding the 12 cranial nerves and their jobs is very important. It’s a basic part of brain care. It helps doctors find and treat many brain problems well.
Olfactory Nerve (CN I): The Sense of Smell
The olfactory nerve is key to how we smell things. It picks up odor molecules in the air and sends this info to our brain. There, it’s turned into specific smells we can recognize.
Functional Anatomy and Olfactory Pathway
The olfactory nerve is made up of special nerve fibers for smell. These fibers start in the nasal cavity’s olfactory epithelium. The smell pathway goes from the olfactory receptors to the olfactory bulb and then to the brain.
This process is quite complex:
- Odor molecules bind to olfactory receptors.
- Signals are sent to the olfactory bulb.
- The olfactory bulb processes these signals and sends them to the brain.
- The brain interprets these signals as specific smells.
Clinical Testing and Common Disorders
Testing the olfactory nerve checks how well a person can smell different things. This is done with smell tests. Disorders like anosmia (loss of smell), hyposmia (reduced smell), and dysosmia (distorted smell) can affect this nerve.
Disorder | Description | Causes |
Anosmia | Loss of smell | Trauma, infections, neurological disorders |
Hyposmia | Reduced sense of smell | Aging, nasal congestion, certain medications |
Dysosmia | Distorted sense of smell | Infections, neurological conditions, unknown causes |
Evolutionary Significance
The sense of smell is very important for survival. It helps us find food, avoid dangers, and is linked to memory and emotions. The ability to smell a wide range of odors has been vital for humans.
“The sense of smell is closely linked to memory, which is why smells often evoke strong emotional responses.”
Learning about the olfactory nerve helps us understand our sense of smell better. It shows how important smell is for our health and happiness.
Optic Nerve (CN II): Vision Pathway
The Optic nerve, or CN II, is key for sending visual info from the eye to the brain. It’s the second cranial nerve and is vital for seeing and understanding what we see.
Structure and Visual Processing
The Optic nerve is made of axons from ganglion cells in the retina. These axons meet at the optic disc, forming the Optic nerve. Its structure is complex, carrying visual signals from the retina to the brain.
Visual processing starts with photoreception in the retina and ends with interpreting visual data in the brain. The Optic nerve is essential for this, carrying electrical signals from light exposure to the brain.
Visual Field Defects
Visual field defects happen when the visual pathway is damaged, including the Optic nerve. Common issues include:
- Blind spots (scotomas)
- Loss of peripheral vision
- Homonymous hemianopia (loss of half the visual field on the same side in both eyes)
These problems can come from trauma, tumors, or vascular disorders affecting the Optic nerve or other parts of the visual pathway.
Clinical Assessment Techniques
Several clinical methods are used to assess the Optic nerve:
Technique | Description | Clinical Significance |
Visual Acuity Testing | Measures the sharpness of vision | Helps diagnose conditions affecting the Optic nerve |
Visual Field Testing | Assesses the extent of the visual field | Detects defects in the visual pathway |
Ophthalmoscopy | Examines the retina and optic disc | Reveals abnormalities in the Optic nerve |
These methods are vital for diagnosing and managing Optic nerve conditions and vision problems.
Oculomotor Nerve (CN III): Eye Movement and Pupillary Control
The oculomotor nerve, or cranial nerve III, is key in eye movement and light adjustment. It’s vital for our eye control and light response.
Motor Functions for Eye Muscles
The oculomotor nerve controls several eye muscles. These include the superior, inferior, and medial recti, plus the inferior oblique. Together, they help us move our eyes and see clearly.
Extraocular Muscles Innervated by CN III:
Muscle | Function |
Superior Rectus | Elevation |
Inferior Rectus | Depression |
Medial Rectus | Adduction |
Inferior Oblique | Extorsion, Elevation |
Parasympathetic Functions for Pupil Constriction
The oculomotor nerve also controls pupil size. This is important for light control and eye health.
“The parasympathetic innervation of the iris sphincter muscle and the ciliary muscle is mediated by the oculomotor nerve, playing a vital role in the pupillary light reflex.” –
Neurology Textbook
Oculomotor Nerve Palsy
Oculomotor nerve palsy, or third nerve palsy, happens when the nerve is damaged. Symptoms include a drooping eyelid, double vision, and uneven pupil sizes.
Knowing about the oculomotor nerve’s role is key for diagnosing and treating related conditions. We’ll look into the effects of oculomotor nerve palsy next.
Trochlear Nerve (CN IV): Superior Oblique Muscle Control
The trochlear nerve controls the superior oblique muscle, which is key for eye movement. It is the fourth cranial nerve and plays a big role in eye control. We will look at its anatomy, function, special traits, and its importance in medicine.
Anatomy and Function
The trochlear nerve starts in the midbrain and is unique because it comes out of the back of the brainstem. It connects to the superior oblique muscle. This muscle is important for eye rotation.
The muscle helps the eye move down and to the side, mainly when the eye is pulled towards the nose.
Unique Characteristics
The trochlear nerve stands out in several ways. It is the smallest cranial nerve by the number of axons. It also has the longest path inside the skull, making it more likely to get hurt.
Its special way of crossing over at the superior medullary velum is another unique trait.
Clinical Testing and Disorders
Doctors test the trochlear nerve by checking how well the superior oblique muscle works. They ask patients to follow a target with their eyes, focusing on movements that need the superior oblique muscle.
Problems with the trochlear nerve can cause the muscle to weaken or not work at all. This can lead to diplopia (double vision), mostly when looking down.
There are many reasons why the trochlear nerve can get damaged, like injuries, lack of blood, or being pressed by tumors or aneurysms. Knowing how to spot these problems and using the right tests is key to treating trochlear nerve palsy.
Trigeminal Nerve (CN V): Facial Sensation and Mastication
The trigeminal nerve is key to the cranial nervous system. It handles sensory input from the face and motor output for chewing. As the fifth cranial nerve, it has two main roles. It provides sensory innervation to the face and motor innervation to chewing muscles.
Three Major Branches: Ophthalmic, Maxillary, and Mandibular
The trigeminal nerve splits into three main branches: ophthalmic, maxillary, and mandibular. Each branch covers different areas and functions. The ophthalmic division handles the eye and surrounding areas. The maxillary division covers the mid-face, like the cheeks and upper lip. The mandibular division does both sensory and motor functions, covering the lower face and controlling chewing muscles.
Sensory Distribution of the Face
The trigeminal nerve is in charge of the face’s general sensory function. Its three divisions cover various areas, providing vital sensation. This sensation is key for touch, temperature, and pain detection. It’s essential for face protection and functions like eating and speaking.
Motor Functions for Chewing
The trigeminal nerve also has a motor function. The mandibular division controls the chewing muscles. These muscles work together for chewing. This makes the trigeminal nerve vital for mastication.
Trigeminal Neuralgia and Clinical Assessment
Trigeminal neuralgia causes intense, shock-like pain in the face. It’s often due to nerve compression or irritation. Doctors assess the nerve’s functions through tests. They check facial sensation, the corneal reflex, and chewing muscle strength and coordination.
Abducens Nerve (CN VI): Lateral Rectus Control
The Abducens nerve, or CN VI, is key in eye movement control. It works by innervating the lateral rectus muscle. This muscle helps the eye move outward. Knowing how the Abducens nerve works is vital for treating eye problems.
Anatomy and Function
The Abducens nerve starts in the pons of the brainstem. It goes through the subarachnoid space and the dura mater. Then, it passes through the cavernous sinus and the superior orbital fissure to reach the orbit.
Inside the orbit, it connects with the lateral rectus muscle. This muscle is one of six that control eye movements.
The main job of the Abducens nerve is to control the lateral rectus muscle. This lets the eye move outward. This movement is important for seeing things clearly and tracking objects.
Characteristics | Description |
Origin | Pons in the brainstem |
Function | Innervates lateral rectus muscle for outward eye movement |
Pathway | Subarachnoid space, dura mater, cavernous sinus, superior orbital fissure |
Clinical Significance of Abducens Palsy
Abducens nerve palsy makes the lateral rectus muscle weak or paralyzed. This leads to trouble moving the eye outward. It can cause the eye to turn inward and double vision.
Many things can cause Abducens palsy, like injuries, blood vessel problems, tumors, and inflammation.
“The diagnosis of Abducens nerve palsy involves a thorough clinical check-up. This includes looking at eye movements and might need imaging to find the cause.” –
A clinical expert
Relationship to Other Ocular Nerves
The Abducens nerve works with other nerves like the Oculomotor (CN III) and Trochlear (CN IV) nerves. Together, they help the eyes move smoothly. This is important for tracking objects and keeping vision clear.
It’s important to understand how these nerves work together. This helps in diagnosing and treating eye problems.
Facial Nerve (CN VII): Facial Expression and Taste
The facial nerve is key for facial movements and taste. It’s a complex nerve with motor, sensory, and autonomic fibers. This makes it very versatile.
Motor Innervation of Facial Muscles
The facial nerve controls facial muscles. This lets us show emotions like smiling and frowning. It’s important for talking without words.
Key Functions: Facial expression, including smiling and frowning; control of muscles around the eyes and mouth.
Taste Function to Anterior Two-Thirds of Tongue
The facial nerve also transmits taste from the tongue’s front part. It’s vital for tasting sweet, sour, salty, bitter, and umami. This nerve’s taste role is often overlooked but is key for enjoying food.
The connection between taste and smell is also important. Together, they help us fully enjoy food flavors.
Autonomic Functions for Lacrimal and Salivary Glands
The facial nerve also controls the lacrimal and salivary glands. The lacrimal gland makes tears, and the salivary glands produce saliva. This helps with digestion and keeps our mouth clean.
Gland | Function | Innervation by Facial Nerve |
Lacrimal Gland | Tear Production | Parasympathetic Innervation |
Submandibular Gland | Saliva Production | Parasympathetic Innervation |
Sublingual Gland | Saliva Production | Parasympathetic Innervation |
Bell’s Palsy and Clinical Assessment
Bell’s palsy is a condition that weakens facial muscles. It’s not fully understood but might be due to nerve inflammation or compression. Doctors check facial muscle strength and taste to diagnose it.
Understanding the facial nerve’s functions is key for diagnosing and treating nerve disorders. Recognizing symptoms helps doctors provide better care and improve patient outcomes.
Vestibulocochlear Nerve (CN VIII): Hearing and Balance
The Vestibulocochlear nerve, or CN VIII, is key for hearing and balance. It sends special sensory info from the inner ear to the brain. There, it helps us hear sounds and stay balanced.
Vestibular Component: Balance Mechanism
The vestibular part of CN VIII helps us keep our balance. It has three semicircular canals and the otolith organs. These are filled with fluid and have sensory hair cells.
When we move our head, the fluid in these canals and organs moves too. This movement bends the hair cells, sending nerve impulses to the brain. These impulses help us stay balanced and oriented in space.
Cochlear Component: Auditory Pathway
The cochlear part of CN VIII lets us hear. The cochlea, a spiral in the inner ear, turns sound vibrations into electrical signals. These signals go to the brain.
Sound waves make the fluid in the cochlea vibrate. This vibration stimulates the hair cells, creating nerve impulses. These impulses are sent to the brain for us to understand sounds.
Disorders Affecting Hearing and Equilibrium
Several disorders can harm CN VIII, causing hearing and balance problems. Some common ones include:
- Ménière’s disease, which causes vertigo, tinnitus, and hearing loss
- Vestibular neuritis, an inflammation of the vestibular nerve that can cause severe vertigo
- Cochlear damage due to noise exposure or ototoxic medications, leading to hearing loss
- Acoustic neuromas, benign tumors that can compress CN VIII and affect both hearing and balance
Disorder | Symptoms | Affected Component |
Ménière’s disease | Vertigo, tinnitus, hearing loss | Vestibular and cochlear |
Vestibular neuritis | Severe vertigo | Vestibular |
Cochlear damage | Hearing loss | Cochlear |
Acoustic neuroma | Hearing loss, balance problems | Both vestibular and cochlear |
Knowing about the Vestibulocochlear nerve’s functions and disorders is key. It helps in diagnosing and treating inner ear and balance issues. By understanding symptoms and affected areas, doctors can offer better care and management for CN VIII-related problems.
Glossopharyngeal and Vagus Nerves (CN IX, X): Throat, Taste, and Autonomic Functions
The Glossopharyngeal and Vagus nerves, or CN IX and X, are key for throat function, taste, and controlling the body. They help with swallowing, making saliva, and managing organs inside the body.
Glossopharyngeal Nerve: Throat and Posterior Tongue
The Glossopharyngeal nerve handles both sensory and motor tasks. It sends signals from the back of the tongue, throat, and middle ear. It also controls the stylopharyngeus muscle, which helps us swallow.
Sensory Functions: This nerve brings taste from the back of the tongue and feels sensations in the throat.
Function | Description |
Taste Sensation | Carries taste from the posterior one-third of the tongue |
General Sensation | Provides sensory innervation to the oropharynx |
Motor Innervation | Innervates the stylopharyngeus muscle for swallowing |
Vagus Nerve: The Wanderer’s Extensive Distribution
The Vagus nerve is very wide-reaching, covering the chest and belly. It helps control organs like the heart, lungs, and stomach.
Parasympathetic Functions: It helps control heart rate, aids digestion, and manages other body functions. It’s vital for keeping the body balanced and working right.
Parasympathetic Functions and Visceral Control
Both nerves help control the body’s parasympathetic functions. The Glossopharyngeal nerve helps with saliva, while the Vagus nerve affects the heart and stomach.
“The Vagus nerve is often referred to as the ‘wanderer’ due to its extensive distribution throughout the body, influencing various physiological processes.”
Clinical Testing and Common Disorders
Doctors test these nerves by checking gag reflex, swallowing, and body responses. Problems with these nerves can cause swallowing issues, voice changes, and body control problems.
Common Disorders: Issues like Vagus nerve palsy can cause voice loss, swallowing trouble, and body control issues. Knowing how these nerves work is key to diagnosing and treating these problems.
Accessory and Hypoglossal Nerves (CN XI, XII): Neck and Tongue Control
The Accessory and Hypoglossal nerves are key for neck and tongue movements. They help us perform daily tasks by controlling these areas.
Sternocleidomastoid and Trapezius Muscles
The Accessory nerve, or CN XI, controls the sternocleidomastoid and trapezius muscles. These muscles are vital for neck and shoulder movements. The sternocleidomastoid helps turn the head and tilt it, while the trapezius lifts and rotates the scapula.
Damage to the Accessory nerve can cause muscle weakness or paralysis. This makes it hard to move the neck and shoulders.
Tongue Movement and Speech
The Hypoglossal nerve, or CN XII, controls tongue movements. It helps the tongue protrude, retract, and change shape. These actions are key for speaking, swallowing, and eating.
Problems with the Hypoglossal nerve can make it hard to speak and swallow. It also affects how we manage food in our mouths.
Clinical Assessment and Disorders
Doctors check the strength and function of the muscles these nerves control. For the Accessory nerve, they test the sternocleidomastoid and trapezius muscles. They look for weakness or atrophy.
For the Hypoglossal nerve, they assess tongue movements and strength. Disorders like trauma, infections, or tumors can harm these nerves. This leads to problems with neck and tongue functions.
Understanding these nerves is key for accurate diagnoses and treatment. This helps improve patient outcomes and quality of life.
Conclusion: Mastering Cranial Nerve Assessment in Clinical Practice
Learning about cranial nerve assessment is key for healthcare workers. It helps them diagnose and treat many neurological issues. We’ve looked at the 12 cranial nerves and their roles in our body’s functions.
Testing these nerves is a big part of checking a patient’s neurology. This knowledge lets us find and fix problems with the nerves. It helps us give better care and improve our patients’ lives.
We need to keep getting better at checking the nerves. This keeps us current with new ways to care for patients. By doing this, we make sure our patients get the best care for their needs.
FAQ
What are the 12 cranial nerves and their functions?
The 12 cranial nerves are key to our body’s functions. They include the Olfactory (CN I) for smell and the Optic (CN II) for vision. The Oculomotor (CN III) and Trochlear (CN IV) control eye movements and pupil size.
The Trigeminal (CN V) handles facial sensations and chewing. The Abducens (CN VI) controls the lateral rectus muscle. The Facial (CN VII) is for facial expressions and taste.The Vestibulocochlear (CN VIII) is vital for hearing and balance. The Glossopharyngeal (CN IX) and Vagus (CN X) manage throat functions and taste. The Accessory (CN XI) and Hypoglossal (CN XII) control neck and tongue movements.
What is the function of the Olfactory nerve (CN I)?
The Olfactory nerve transmits smell information from the nose to the brain. It’s key for us to sense different odors.
What is the role of the Optic nerve (CN II) in vision?
The Optic nerve carries visual information from the retina to the brain. It’s essential for us to see and interpret visual stimuli.
What are the functions of the Oculomotor nerve (CN III)?
The Oculomotor nerve controls most eye movements. It rotates the eyeball, constricts the pupil, and keeps the eyelid open. It’s vital for eye movement and controlling the pupil.
What is the Trigeminal nerve (CN V) responsible for?
The Trigeminal nerve handles facial sensations like pain, temperature, and touch. It also controls chewing. It’s important for both sensory and motor functions.
What is the clinical significance of cranial nerves?
Knowing about cranial nerves is key for diagnosing and treating neurological issues. Damage to these nerves can cause various symptoms and deficits.
How are cranial nerves classified?
Cranial nerves are divided into three main types. Sensory nerves transmit sensory info. Motor nerves control muscle movements. Mixed nerves do both.
What is the role of the Vestibulocochlear nerve (CN VIII) in hearing and balance?
The Vestibulocochlear nerve is vital for hearing and balance. The cochlear part handles hearing, while the vestibular part helps with balance and equilibrium.
What are the functions of the Glossopharyngeal and Vagus nerves?
The Glossopharyngeal nerve is involved in throat function and taste. The Vagus nerve controls various bodily functions through parasympathetic actions. They’re key for autonomic control and bodily functions.
What is the significance of the Accessory and Hypoglossal nerves?
The Accessory nerve controls neck muscles for movement. The Hypoglossal nerve is for tongue movement and speech. They’re important for motor functions of the neck and tongue.
How do cranial nerve disorders affect patients?
Cranial nerve disorders can cause symptoms like pain, numbness, weakness, or paralysis. They can greatly affect a patient’s quality of life.
What is the importance of understanding cranial nerve anatomy and function?
Knowing about cranial nerves is essential for diagnosing and treating neurological conditions. It’s vital for healthcare professionals to have a deep understanding.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC11523702/






