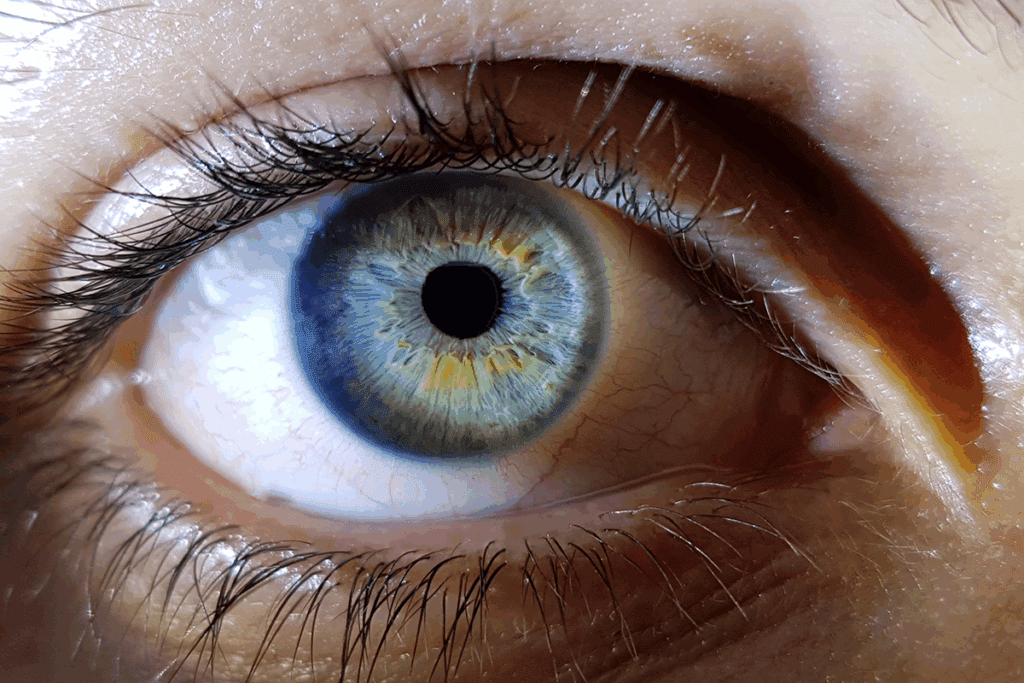
Red eye is a common problem in eye care, affecting people of all ages. It’s important to differential diagnosis to tell the difference between harmless and serious issues.Conjunctivitis uveitis: what’s the difference? One is simple pink eye, the other is an alarming threat to your vision. Learn the signs.
At Liv Hospital, we use the latest diagnostic tools and follow international standards. This helps us accurately identify and treat red eye conditions like conjunctivitis, uveitis, episcleritis, keratitis, scleritis, and angle-closure glaucoma.
It’s key to understand these conditions to treat them well and avoid serious problems. Our focus on patients ensures they get the best care, whether they’re from here or abroad.
Key Takeaways
- Red eye is a common complaint that can range from benign to sight-threatening conditions.
- Accurate diagnosis is key for good treatment and avoiding complications.
- Liv Hospital follows international medical protocols for complete care.
- Six major red eye conditions are evaluated, including conjunctivitis and uveitis.
- Advanced diagnostic techniques ensure precise identification of red eye conditions.
Understanding Red Eye: A Common Clinical Presentation
Red eye is a common issue that needs a detailed check to find out why it happens. It’s a big deal in both eye doctor offices and regular doctor visits. In Eastern Europe, it’s a big reason for visits to eye doctors and general practitioners.
Prevalence and Significance in Clinical Practice
Red eye is seen a lot in doctor’s offices. This means doctors need to know a lot about it. Red eye types can be simple or very serious. Knowing the difference is key to treating it right.
Red eye can be caused by many things, like conjunctivitis or uveitis. Each one has its own signs and what it means for the patient. For example, conjunctivitis is usually not serious, but uveitis can be very bad if not treated fast.
Red Flags: Distinguishing Benign from Sight-Threatening Conditions
It’s important for doctors to know the difference between mild and serious red eye. Some red flags like a lot of pain or vision problems mean something serious might be going on. For example, a ciliary flush could mean uveitis, which needs quick eye doctor attention.
We must watch for these warning signs to make sure patients get the right care. A good history and check-up are key to figuring out what to do next.
Conjunctivitis: The Most Common Red Eye Condition
Conjunctivitis is the most common cause of red eye. It has different types, each with its own symptoms. We will look at the types, their symptoms, and how to treat them.
Types of Conjunctivitis
There are three main types of conjunctivitis: viral, bacterial, and allergic. Each type needs a different treatment plan.
- Viral Conjunctivitis: Often linked to a cold, it’s very contagious and can be quite uncomfortable.
- Bacterial Conjunctivitis: This is caused by bacteria and has a thick, yellowish discharge. It can be treated with antibiotics.
- Allergic Conjunctivitis: It’s caused by allergens like pollen or dust. It makes your eyes itch and have watery discharge.
Clinical Presentation and Diagnostic Features
The symptoms of conjunctivitis depend on its type. Knowing these differences is key to diagnosing and treating it correctly. It’s important to tell conjunctivitis apart from other red eye causes like uveitis.
Type of Conjunctivitis | Common Symptoms | Diagnostic Features |
Viral | Watery discharge, redness, irritation | Presence of viral infection, highly contagious |
Bacterial | Purulent discharge, redness | Purulent discharge, positive bacterial culture |
Allergic | Itching, watery discharge, redness | History of allergies, presence of allergens |
Treatment Approaches and Management
The treatment for conjunctivitis varies by cause. Viral conjunctivitis is treated with symptoms relief. Bacterial conjunctivitis may need antibiotics. Allergic conjunctivitis is treated with anti-allergic meds.
In conclusion, conjunctivitis is a common issue that needs careful diagnosis and treatment. Knowing the differences between its types and other red eye causes is key to good patient care.
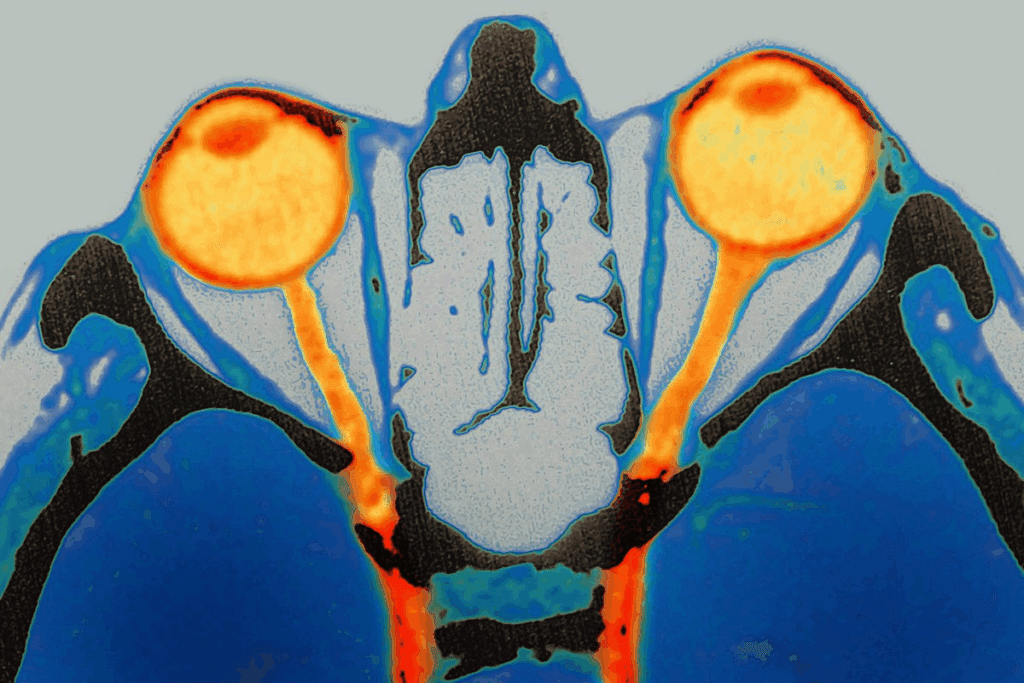
Uveitis: Inflammation of the Uveal Tract
The uveal tract is a key part of the eye. It can get inflamed, causing uveitis. This is a serious condition that affects the iris, ciliary body, and choroid.
Forms of Uveitis
Uveitis is divided into three types: anterior, intermediate, and posterior. Each type affects different parts of the eye and has its own symptoms.
- Anterior Uveitis: This type affects the iris and ciliary body. It causes pain, sensitivity to light, and blurry vision. It also leads to a red eye.
- Intermediate Uveitis: This type affects the vitreous and retina. People may see floaters and have blurry vision.
- Posterior Uveitis: This type affects the choroid and retina. It causes vision problems and blind spots.
Recognizing Uveitis: Ciliary Flush and Associated Symptoms
It’s important to recognize uveitis early. Anterior uveitis causes redness, pain, and sensitivity to light. These symptoms need quick attention from an eye doctor to avoid serious problems.
“Uveitis is a significant cause of visual morbidity, and its diagnosis requires a high index of suspicion and thorough examination.”
Management and Possible Complications
Managing uveitis means treating the cause and controlling inflammation. Doctors may use eye drops or pills to help. If not treated, uveitis can cause cataracts, glaucoma, and retinal detachment.
It’s key to know the difference between uveitis and other eye problems like episcleritis, keratitis, and conjunctivitis. Uveitis can cause serious vision loss if not treated right away.
Conjunctivitis and Uveitis: Comparative Analysis and Differential Diagnosis
It’s important to know the difference between conjunctivitis and uveitis to treat them right. Both can make your eyes red, but they affect your eyes differently.
Pain Levels and Visual Acuity Changes
Conjunctivitis usually feels mildly uncomfortable or like something is in your eye. Uveitis, on the other hand, hurts a lot and can make your vision blurry or worse.
Here’s a quick look at how they compare:
Condition | Pain Level | Visual Acuity Changes |
Conjunctivitis | Mild discomfort | Minimal or none |
Uveitis | Significant pain | Blurred vision or decreased visual acuity |
Pupillary Responses and Corneal Involvement
The way your pupils react can tell you which condition you might have. Uveitis can make your pupils small or irregular. Conjunctivitis usually doesn’t affect them.
Corneal involvement is another key difference. Uveitis can cause serious inflammation on the cornea. Conjunctivitis might cause some minor irritation, but it’s not as bad.
To tell conjunctivitis from uveitis, doctors need to check your eye carefully. They look at pain, vision, pupil reactions, and corneal health. Getting it right is key to treating your eyes properly.
Episcleritis: Inflammation of the Episcleral Tissue
The episclera is a thin layer on top of the sclera. It can get inflamed, causing episcleritis. This condition often looks like other red eye issues, like conjunctivitis or scleritis. Knowing about episcleritis is key for the right treatment.
Simple vs. Nodular Episcleritis
There are two main types of episcleritis: simple and nodular. Simple episcleritis makes the eye look red or pink. Nodular episcleritis has a distinct nodule and hurts more.
It’s important to know the difference. Simple episcleritis is more common and usually goes away on its own. But nodular episcleritis needs special treatment because it hurts more.
Clinical Features and Diagnostic Approach
Episcleritis makes the eye red, hurts a bit, and might have watery discharge. It doesn’t usually hurt a lot or affect vision. Doctors use a slit-lamp to check the inflammation and rule out other problems.
It’s important to tell episcleritis apart from other red eye issues. A ciliary flush or corneal involvement helps doctors make the right diagnosis.
Association with Systemic Autoimmune Diseases
Episcleritis is linked to autoimmune diseases in up to one-third of cases. It’s important to think about these diseases when someone has episcleritis. People with severe or recurring episcleritis might need a full check-up for other diseases.
Knowing about the connection between episcleritis and autoimmune diseases helps doctors treat the whole person. This way, they can help with both the eye symptoms and any underlying diseases.
Scleritis: A Potentially Sight-Threatening Condition
Scleritis is an inflammation of the sclera that can threaten your sight. It causes severe pain, redness, and sensitivity to light. Unlike less serious conditions like conjunctivitis or episcleritis, scleritis affects deeper eye layers. This makes it a serious issue that needs quick medical help.
Forms of Scleritis
Scleritis can be divided into two types: anterior and posterior. Anterior scleritis is more common and can be further split into non-necrotizing and necrotizing types. Posterior scleritis is rarer but harder to diagnose because of its location.
Anterior vs. Posterior Scleritis: Knowing the difference between these forms is key for proper treatment. The table below shows the main differences.
Characteristics | Anterior Scleritis | Posterior Scleritis |
Location | Front part of the sclera | Back part of the sclera |
Symptoms | Severe eye pain, redness, photophobia | May have fewer symptoms initially; can present with decreased vision |
Diagnostic Challenges | Generally easier to diagnose due to visible symptoms | More challenging; may require imaging studies |
Clinical Presentation and Diagnostic Features
Scleritis symptoms include severe eye pain that feels deep and boring. It can also cause tenderness, photophobia, and decreased vision. Doctors can confirm scleral edema and inflammation through a slit-lamp exam.
Management and Systemic Associations
Treating scleritis involves reducing inflammation and managing any underlying diseases. Doctors often use oral NSAIDs or corticosteroids. In severe cases, immunosuppressive therapy might be needed. It’s also important to treat any related systemic diseases, like rheumatoid arthritis, as they can affect treatment.
It’s important to know the differences between scleritis and other eye conditions like episcleritis, conjunctivitis, or uveitis. This helps in making the right diagnosis and treatment. The table below compares scleritis with these conditions.
Condition | Location | Severity | Associated Symptoms |
Scleritis | Sclera | High | Severe pain, photophobia, decreased vision |
Episcleritis | Episclera | Low to Moderate | Mild discomfort, redness |
Conjunctivitis | Conjunctiva | Variable | Discharge, redness, irritation |
Uveitis | Uvea | High | Pain, photophobia, vision disturbances |
Keratitis: Corneal Inflammation and Infection
Keratitis is a serious eye condition that can harm your vision. It happens when the cornea, the clear part of the eye, gets inflamed. This can be due to an infection or other reasons. We will look at the different kinds of keratitis, how to diagnose them, and how to treat them.
Infectious vs. Non-Infectious Keratitis
Keratitis can be caused by infections or other factors. Infections come from bacteria, viruses, fungi, or parasites. Non-infectious keratitis can be caused by injuries, dry eyes, or autoimmune diseases.
Infectious Keratitis: This type often happens in people who wear contact lenses or have eye injuries. Common culprits include Pseudomonas aeruginosa and Fusarium species.
Non-Infectious Keratitis: Dry eye, eye exposure, and diseases like rheumatoid arthritis can cause this type.
Clinical Features and Diagnostic Approach
Keratitis symptoms vary based on the cause. You might feel eye pain, see redness, have trouble with light, or see blurry.
- Slit-lamp exams help doctors see how bad the cornea is.
- Corneal scrapings or cultures can find the cause of infections.
- Imaging like corneal topography helps check for irregularities.
Treatment Strategies and Visual Outcomes
Treatment for keratitis depends on the cause. For infections, doctors use antibiotics. Non-infectious cases might get anti-inflammatory drugs or other support.
Type of Keratitis | Treatment Approach | Visual Outcome |
Infectious | Antimicrobial therapy | Variable, depends on promptness and effectiveness of treatment |
Non-Infectious | Anti-inflammatory agents, supportive care | Generally better than infectious, but depends on underlying cause |
Knowing the difference between keratitis and uveitis is key. Both can hurt your eyes, but they need different treatments.
“The distinction between keratitis and uveitis is critical, as the management strategies for these conditions are distinct and require a tailored approach to prevent complications and optimize visual outcomes.”
By correctly diagnosing and treating keratitis, we can save people’s vision. It’s important to know about the different types and treatments to give the best care.
Angle-Closure Glaucoma: An Ocular Emergency
We see angle-closure glaucoma as a serious condition that needs quick action. It’s an eye emergency caused by a sudden rise in eye pressure. This happens when the drainage angle of the eye gets blocked.
Pathophysiology and Risk Factors
Angle-closure glaucoma happens when the iris blocks the eye’s drainage angle. This stops the aqueous humor from draining, leading to a fast increase in eye pressure. This high pressure can damage the optic nerve.
Risk factors include a shallow anterior chamber, being farsighted, having a family history of glaucoma, and certain ethnic backgrounds.
Key risk factors for angle-closure glaucoma include:
- Shallow anterior chamber depth
- Hyperopia
- Family history of glaucoma
- East Asian or Inuit descent
Classic Presentation and Diagnostic Features
People with angle-closure glaucoma often have severe eye pain, headaches, nausea, vomiting, and blurry vision. They might also see halos around lights. Signs include a red eye, corneal edema, a mid-dilated pupil, and high eye pressure.
To confirm the diagnosis, doctors measure eye pressure with tonometry. They also check the anterior chamber angle with gonioscopy.
Symptom | Description |
Severe Eye Pain | Sudden onset of pain in the eye |
Headache | Often accompanies eye pain |
Nausea and Vomiting | Can occur due to severe pain and increased IOP |
Blurred Vision | Vision disturbances due to corneal edema |
Halos Around Lights | Symptoms due to corneal edema |
Emergency Management and Long-Term Care
Emergency care aims to lower eye pressure quickly to prevent optic nerve damage. Doctors use medications like topical beta-blockers and prostaglandin analogs. They also use systemic acetazolamide. Laser peripheral iridotomy is often done to create a new drainage pathway.
Long-term care includes watching eye pressure, managing secondary conditions, and possibly more surgeries. This helps keep the drainage angle open.
Emergency treatment steps for angle-closure glaucoma:
- Administer topical and systemic medications to lower IOP
- Perform laser peripheral iridotomy
- Monitor IOP and adjust treatment as necessary
Conclusion: When to Seek Immediate Medical Attention for Red Eye
Red eye can mean many things, from minor to serious eye problems. We’ve looked at several eye issues, like conjunctivitis and glaucoma. It’s key to know what’s causing the redness to get the right treatment.
It’s important to see a doctor quickly if your red eye is severe. Look out for pain, vision changes, or light sensitivity. If you see these signs, get help fast to avoid serious eye damage.
In short, knowing about eye problems helps us treat them better. If your eyes are red and you see warning signs, see a doctor right away. Quick action can save your vision and prevent future problems.
FAQ
What are the main differences between conjunctivitis and uveitis?
Conjunctivitis and uveitis are both red eye conditions. But they show different signs and need different treatments. Conjunctivitis causes eye redness, discharge, and itching. Uveitis, on the other hand, leads to pain, light sensitivity, and vision changes.
How can I distinguish between episcleritis and scleritis?
Episcleritis and scleritis are eye inflammation issues. But they have different symptoms. Episcleritis causes eye redness and discomfort. Scleritis is more severe, with pain, tenderness, and vision loss risk.
What are the symptoms of keratitis, and how is it treated?
Keratitis is cornea inflammation. It causes eye pain, redness, and vision changes. Treatment depends on the cause. It might include antibiotics, anti-inflammatory drugs, or other methods.
What is angle-closure glaucoma, and why is it an emergency?
Angle-closure glaucoma is a sudden, severe eye condition. It causes eye pain, redness, and vision loss. Quick treatment is needed to avoid permanent vision damage.
How can I differentiate between conjunctivitis and keratitis?
Conjunctivitis and keratitis are both red eye issues. But they affect different parts of the eye. Conjunctivitis affects the conjunctiva, causing redness and itching. Keratitis affects the cornea, leading to pain and vision changes.
What is the difference between uveitis and episcleritis?
Uveitis and episcleritis are eye inflammation conditions. Uveitis affects the uveal tract, causing pain and vision changes. Episcleritis affects the episcleral tissue, leading to eye redness and discomfort.
Can conjunctivitis cause vision loss?
Conjunctivitis usually doesn’t cause permanent vision loss. But, it can lead to complications that might affect vision. Other conditions like uveitis, scleritis, or keratitis can cause vision loss if not treated properly.
How is scleritis associated with systemic diseases?
Scleritis is linked to autoimmune diseases like rheumatoid arthritis. Knowing this is important for treating scleritis effectively.
What are the risk factors for developing angle-closure glaucoma?
Angle-closure glaucoma risk factors include a shallow anterior chamber. Age and ethnicity also play a role.
What are the key differences between anterior uveitis and episcleritis?
Anterior uveitis and episcleritis are eye inflammation conditions. Anterior uveitis causes pain and vision changes. Episcleritis leads to eye redness and discomfort.
How can I tell if my red eye is caused by a benign or sight-threatening condition?
Look out for red flags like severe pain, vision changes, and light sensitivity. If you see these, get medical help right away.
References
Government Health Resource. Evidence-Based Medical Guidance. Retrieved from https://www.aafp.org/pubs/afp/issues/2010/0115/p137.html



