A complete cranial nerve examination is key in checking the brain and nerves. It helps find problems and where they are. This test looks at the twelve pairs of cranial nerves. These nerves control senses and movements in the head and neck.Master the CN examination. This ultimate clinical guide provides a clear, step-by-step process for assessing all 12 cranial nerves.
Healthcare experts use this test to spot and treat brain and nerve issues. The neuro exam cranial nerves test is very useful in urgent cases. It’s also great for checking on patients with brain injuries or other serious brain problems.
Key Takeaways
- A complete cranial nerve examination is essential for brain checks.
- It helps find and pinpoint brain and nerve problems.
- The test is very important in emergency situations and for brain injury patients.
- Knowing how cranial nerves work helps in diagnosing brain and nerve issues.
- Good treatment of brain and nerve problems depends on accurate diagnosis.
The Fundamentals of Neurological Assessment

Understanding the basics of neurological assessment is key to diagnosing and treating neurological conditions. The cranial nerve examination is a critical part of this process. It checks the twelve pairs of cranial nerves that handle sensory and motor functions in the head and neck.
Cranial nerves start in the brain stem. Problems with them can show issues in the brain stem or along their path. Knowing how cranial nerves work is vital for finding and diagnosing problems.
Anatomical Basis of Cranial Nerves
The twelve cranial nerves manage many important functions. These include:
- Sensory tasks like smell, vision, hearing, and face sensation
- Motor tasks like eye movement, facial expressions, swallowing, and tongue actions
It’s important to know where each cranial nerve starts and goes. For example, the olfactory nerve (Cranial Nerve I) carries smell information from the nose to the brain.
Clinical Significance in Neurological Diagnosis
Problems with cranial nerves can point to various neurological issues. For instance:
- A third cranial nerve palsy can cause a droopy eyelid, a big pupil, and an eye that looks outward.
- A facial nerve palsy can lead to weakness or paralysis of facial muscles.
By using cranial nerve exam results in a bigger neurological assessment, doctors can make better diagnoses and treatment plans. The cranial nerve exams are essential for a complete neuro cranial nerve exam and overall neurological check-up.
Preparation and Equipment for CN Examination

To do a good cranial nerve exam, we need the right tools and a good setup. A well-prepared area helps us work fast and right, even in busy or urgent situations.
Essential Tools and Materials
We only need a few key items for a full cranial nerve check. These are:
- A 256-hertz or 512-hertz tuning fork for checking vibration and hearing.
- Ishihara or Hardy-Rand-Ritter plates for color vision tests.
- A fundoscope for looking at the retina and optic disc.
- Visual acuity charts to see how sharp a person’s vision is.
Having these tools ready makes the exam smoother. It helps us check all parts of the cranial nerves well.
Equipment | Purpose |
Tuning Fork (256 Hz or 512 Hz) | Assessing vibration sense and hearing |
Ishihara or Hardy-Rand-Ritter Plates | Testing color vision |
Fundoscope | Examining the retina and optic disc |
Visual Acuity Charts | Evaluating visual sharpness |
Patient Positioning and Environment Setup
It’s important to position the patient right and set up the room well for a good exam. The patient should be comfy and in a bright room. The room should be quiet for better hearing and sensory checks.
With the right setup and tools, we can do a detailed cranial nerve exam. This way, we get accurate results.
Cranial Nerve I: Olfactory Nerve Examination
Checking the olfactory nerve is key for a full brain check-up. The olfactory nerve, or Cranial Nerve I, carries smell info from the nose to the brain.
Technique for Testing Smell Function
We use different ways to see if someone can smell different smells. The main method is to give the person familiar, safe smells, like coffee or vanilla, and ask them to name it. We make sure to test each nostril alone to find out if one smells better than the other.
We make sure the person knows what to do and that there are no other smells around. They usually close their eyes to avoid seeing things that might confuse them.
Interpreting Olfactory Deficits
Problems with smell can mean many things are wrong in the brain. Not being able to smell, called anosmia, can happen if the nerve or brain paths get damaged. It might be from a head injury, infection, or diseases like Alzheimer’s or Parkinson’s.
We look at the person’s health history and how bad the smell problem is. This helps us figure out why they can’t smell well and what to do next.
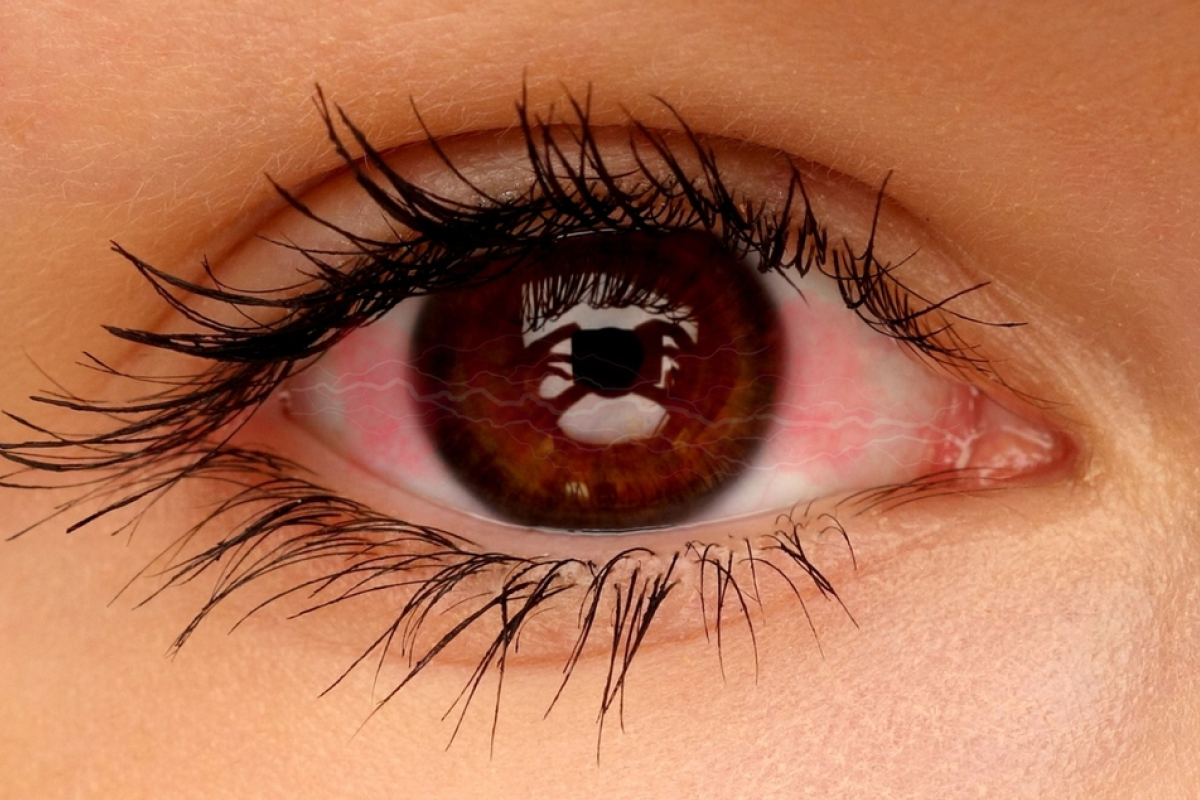
Cranial Nerve II: Optic Nerve Examination
The optic nerve, or Cranial Nerve II, is key to our vision. Its check-up is a big part of checking our brain health. Finding problems here can mean serious issues.
Visual Acuity Assessment Methods
Checking how well we see is a big part of the optic nerve test. We use charts like the Snellen chart to see how sharp our vision is. This test finds if our vision is not clear, which could mean a problem with the optic nerve.
Key steps in visual acuity assessment include:
- Using a well-lit Snellen chart at a standard distance
- Testing each eye separately, starting with the right eye
- Recording the smallest line of text that the patient can read accurately
Visual Field Testing Techniques
Testing our side vision is also important. It checks if we can see things on the sides. We use quick tests to see if there are any problems.
Confrontation visual field testing involves:
- The examiner sitting opposite the patient
- The patient covering one eye while fixating on the examiner’s nose
- The examiner bringing their hand or a target into the patient’s field of vision from the periphery
Fundoscopic Examination Procedure
Looking directly at the optic disc and retina is another part of the test. We use an ophthalmoscope to see the optic nerve head. This helps us find any problems, like swelling or damage.
Steps for fundoscopic examination include:
- Dilating the pupils if necessary
- Using an ophthalmoscope to examine the optic disc and surrounding retina
- Assessing for any abnormalities, such as hemorrhage or exudates
By checking how well we see, our side vision, and looking at the optic disc, we can really understand how well our optic nerve is working. This helps us find and treat problems with our vision.
Cranial Nerves III, IV, and VI: Ocular Motility Assessment
Cranial nerves III, IV, and VI control our eye movements. They are key for diagnosing neurological issues. These nerves help our eyes move in different directions. Checking them is essential to spot any problems with eye movement.
Pupillary Light Reflex Testing
The pupillary light reflex is a key part of a neurological exam. It shows how well cranial nerves II and III are working. We use a light to test this reflex by shining it in one eye and watching both pupils.
A normal response is when the pupil in the lighted eye gets smaller and the other eye’s pupil also gets smaller. But, if a pupil doesn’t get smaller when light hits it, it could mean a problem with the nerve or brain.
Extraocular Movement Examination
Checking how our eyes move involves looking at nerves III, IV, and VI. We ask the patient to follow a moving target with their eyes. This helps us see if there are any issues with eye movement.
- Check for smooth pursuit movements.
- Evaluate saccadic movements by asking the patient to quickly shift their gaze between two targets.
- Observe for nystagmus, which can be a sign of vestibular or neurological dysfunction.
Identifying Specific Nerve Palsies
By closely examining how our eyes move and react to light, we can spot specific nerve problems. For example:
- Third cranial nerve (oculomotor) palsy shows as a droopy eyelid, an eye that looks outward, and a pupil that doesn’t react to light.
- Fourth cranial nerve (trochlear) palsy causes a problem with moving the eye up and down, leading to double vision.
- Sixth cranial nerve (abducens) palsy makes it hard to move the eye outward and causes it to turn inward.
Checking these nerves is very important for patients who are unconscious or have head injuries. It helps us understand their brain’s condition.
Cranial Nerve V: Trigeminal Nerve Examination
Cranial Nerve V, or the trigeminal nerve, handles face sensation and controls chewing muscles. It has three parts: ophthalmic, maxillary, and mandibular. Each part deals with different face sensations.
Sensory Function Testing Across Three Divisions
We check the trigeminal nerve’s sensory function by testing light touch, temperature, and vibration. Light touch is tested with a cotton swab on the face. The patient’s eyes are closed to avoid seeing and guessing.
Temperature sensation is tested with cold and warm objects. This shows if there’s a problem with feeling temperature, which could mean a nerve issue.
Motor Function and Jaw Reflex Assessment
We check the motor part of the trigeminal nerve by looking at chewing muscles. We ask the patient to clench their jaw. Then, we feel these muscles to see if they’re strong and even.
The jaw reflex is tested by tapping the jaw with a hammer. This test checks if the nerve’s motor part is working right.
Cranial Nerve VII: Facial Nerve Examination
Checking the facial nerve is key in neurological exams. It’s important because it helps us smile and taste food. The facial nerve, or Cranial Nerve VII, controls our facial muscles and helps us taste food from the front part of our tongue.
Facial Muscle Strength and Symmetry Testing
We test facial muscle strength and symmetry by asking patients to move their face. They might smile, frown, show their teeth, or raise their eyebrows. It’s important to see if their face moves evenly and if there’s any weakness.
For example, if one side of the face is weak, smiling might not be even. Or, the corner of the mouth might droop. We also check if they can close their eyes tightly and resist us opening them. This tests the strength of the orbicularis oculi muscle.
Facial Movement | Normal Response | Abnormal Response |
Smiling | Symmetrical smile | Asymmetrical smile or drooping |
Frowning | Symmetrical frowning | Weakness or inability to frown on one side |
Showing teeth | Symmetrical display of teeth | Difficulty showing teeth on one side |
Distinguishing Central vs. Peripheral Lesions
It’s important to tell if a facial nerve problem is in the brain or in the nerve itself. Brain problems usually affect the lower face more. Nerve problems can affect the whole face, including the forehead.
To figure this out, we look at where the weakness is. If it’s mainly in the lower face, it might be a brain problem. But if it’s all over the face, it’s likely a nerve issue.
Knowing the difference between brain and nerve problems is key for the right treatment. By looking at how the face moves and where the weakness is, we can make a good diagnosis.
Cranial Nerve VIII: Vestibulocochlear Nerve Examination
Cranial Nerve VIII, or the vestibulocochlear nerve, handles two key senses: hearing and balance. Testing this nerve is key for spotting and treating problems with these senses.
Hearing Assessment Techniques
Testing hearing involves several steps to check how well a person can hear different sounds and volumes. We use methods like pure tone audiometry, speech audiometry, and tuning fork tests to find out the nature and degree of hearing loss.
Pure tone audiometry checks how well a person can hear tones of various frequencies. Speech audiometry looks at their ability to understand speech. Tuning fork tests, like the Weber and Rinne tests, help tell if the hearing loss is due to the middle ear or the inner ear.
Vestibular Function and Balance Testing
Testing the vestibular function looks at how well a person balances and stays steady. We do tests like the Romberg test, tandem walking, and the Dix-Hallpike maneuver to find any problems with balance.
The Romberg test checks if a person can stay balanced with their eyes closed. Tandem walking tests their ability to walk in a straight line. The Dix-Hallpike maneuver helps diagnose benign paroxysmal positional vertigo (BPPV).
By combining the results of these tests, we can fully check the vestibulocochlear nerve’s function. This helps us decide on the best course of action or treatment.
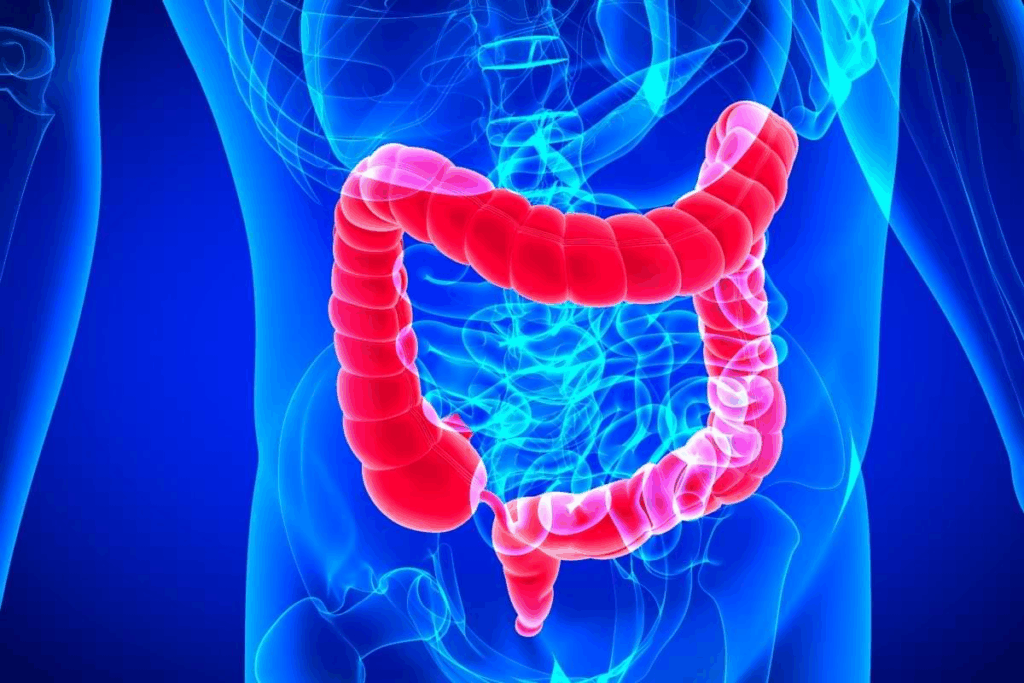
Cranial Nerves IX and X: Pharyngeal and Laryngeal Function
Cranial nerves IX and X are key in swallowing and voice production. Their examination is vital in neurological assessments. These nerves control muscles for swallowing and speaking. Their problems can cause serious issues like swallowing trouble and voice disorders.
Swallowing and Gag Reflex Evaluation
Testing cranial nerves IX and X starts with swallowing and gag reflex checks. We watch how a patient swallows water or food for any trouble. Then, we test the gag reflex by touching the back of the throat with a tongue depressor.
A weak or missing gag reflex might show a problem with cranial nerve IX. Trouble swallowing can point to issues with nerves IX or X, or both. They work together to help us swallow.
Voice Quality and Palatal Movement Assessment
Examining voice quality and palatal movement is also key. We ask patients to say “ah” and look at the soft palate and uvula. In a healthy response, the palate moves up evenly, and the uvula stays in the middle.
Voice quality tells us about the vagus nerve’s health. A hoarse or breathy voice might mean a problem with the vocal cords. We listen for any voice changes and check for signs of vocal cord weakness.
By looking at swallowing, gag reflex, voice, and palate movement, we learn a lot about cranial nerves IX and X. This helps us diagnose and treat related neurological problems.
Cranial Nerve XI: Accessory Nerve Examination
Checking the accessory nerve is key to seeing how well the sternocleidomastoid and trapezius muscles work. This nerve, or Cranial Nerve XI, helps control muscles in the neck and shoulder. If it doesn’t work right, it can cause big problems with moving these muscles.
Sternocleidomastoid and Trapezius Muscle Testing
To see how the accessory nerve is doing, we test the sternocleidomastoid and trapezius muscles. The sternocleidomastoid muscle helps turn the head to the other side and bend the neck. We check its strength by asking the patient to turn their head against resistance.
- Look for any muscle weakness or unevenness.
- Check the sternocleidomastoid muscle’s strength by pushing against the patient’s head as they turn it.
- See how well the trapezius muscle works by checking if the patient can shrug their shoulders against resistance.
The trapezius muscle helps lift the shoulders and move the scapula. We test it by asking the patient to shrug their shoulders against resistance. This shows if the muscle is weak or paralyzed.
Recognizing Accessory Nerve Dysfunction
When the accessory nerve doesn’t work right, it can cause the sternocleidomastoid and trapezius muscles to be weak or paralyzed. Spotting these signs is important for diagnosing and treating related problems.
Key signs of accessory nerve dysfunction include:
- Weakness or trouble turning the head to the other side.
- Hard time lifting the shoulders or moving the scapula.
- Visible muscle wasting or unevenness in the sternocleidomastoid or trapezius muscles.
Finding these signs early helps start the right treatment and rehab. This can improve how well the patient does.
Cranial Nerve XII: Hypoglossal Nerve Examination
The examination of Cranial Nerve XII, the hypoglossal nerve, checks tongue function. It looks for signs of neurological problems. The hypoglossal nerve controls tongue movements, important for speaking and swallowing.
Tongue Movement, Strength, and Appearance
Testing the hypoglossal nerve looks at tongue movement, strength, and appearance. First, we ask the patient to stick out their tongue. We watch for any unevenness, which might show a nerve problem.
Then, we test tongue strength by having the patient push their tongue against their cheek. This is while we press against it with our finger.
The tongue’s look, like its size and any muscle twitches, also tells us about the nerve’s health.
Patterns of Hypoglossal Nerve Dysfunction
It’s key to know how the hypoglossal nerve acts when it’s not working right. If one side of the tongue is weak, it will lean towards the weak side when sticking out. Atrophy and fasciculations point to nerve problems closer to the nerve itself. But, problems higher up can cause trouble speaking and swallowing without showing in the tongue’s look.
Knowing these patterns helps us find where the problem is and what to do next.
Conclusion: Integrating and Documenting the Complete CN Examination
It’s key to document cranial nerve exams well for top-notch patient care. We stress the need to document every part of the cranial nerve exam. This helps track patient progress and guides clinical decisions.
Having a detailed neuro exam cranial nerves report lets healthcare teams see how a patient is doing. It helps spot any neurological issues early and plan the best treatment. Good documentation also makes sure everyone on the healthcare team is on the same page.
By following the steps in this article and keeping detailed records, healthcare pros can give the best care to patients with neurological issues. This method ensures top-notch healthcare services.
FAQ
What is the importance of a complete cranial nerve examination in neurological assessments?
A complete cranial nerve examination is key. It checks the twelve pairs of cranial nerves. These nerves control head and neck functions. This helps doctors diagnose and manage neurological conditions better.
How do I prepare for a cranial nerve examination?
To get ready, make sure you have the right tools like tuning forks and visual charts. Also, make sure the patient is comfortable. This helps get accurate results.
What is the role of the olfactory nerve in neurological diagnosis?
The olfactory nerve handles smell information. Problems with it can point to neurological issues. So, checking it is vital in diagnosing.
How is the optic nerve examined?
The optic nerve is tested through visual acuity, visual field tests, and eye exams. These help diagnose and manage eye problems.
What is the significance of assessing cranial nerves III, IV, and VI?
Checking nerves III, IV, and VI is important. They help diagnose eye movement disorders. This is because they control how our eyes move.
How do you test the trigeminal nerve?
The trigeminal nerve is tested by checking its sensory and motor functions. This includes jaw reflexes. It helps diagnose and manage related conditions.
What is the importance of examining the facial nerve?
Examining the facial nerve is vital. It helps diagnose facial weakness or paralysis. It tests facial muscle strength and symmetry.
How is the vestibulocochlear nerve assessed?
The vestibulocochlear nerve is tested through hearing and balance evaluations. This helps diagnose and manage related disorders.
What is the role of cranial nerves IX and X in pharyngeal and laryngeal function?
Cranial nerves IX and X are key for swallowing and voice functions. Their examination checks swallowing, gag reflex, and voice quality.
How do you examine the accessory nerve?
The accessory nerve is tested by checking the muscles it controls. This helps diagnose and manage shoulder and neck issues.
What is the significance of assessing the hypoglossal nerve?
Assessing the hypoglossal nerve is important. It helps diagnose tongue disorders. It checks tongue movement, strength, and appearance.
Why is documenting the complete cranial nerve examination important?
Documenting the cranial nerve examination is vital. It provides a detailed record of findings. This is important for patient care and decision-making.
What are the best practices for documenting cranial nerve examination findings?
For documenting, it’s important to be accurate and detailed. This is key for effective patient care and decision-making.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK585066/