Idiopathic intracranial hypertension (IIH) is a condition where the pressure inside the brain is too high. But, there’s no clear reason why it happens. At Liv Hospital, we understand the complexities of diagnosing IIH and how important it is to get it right.
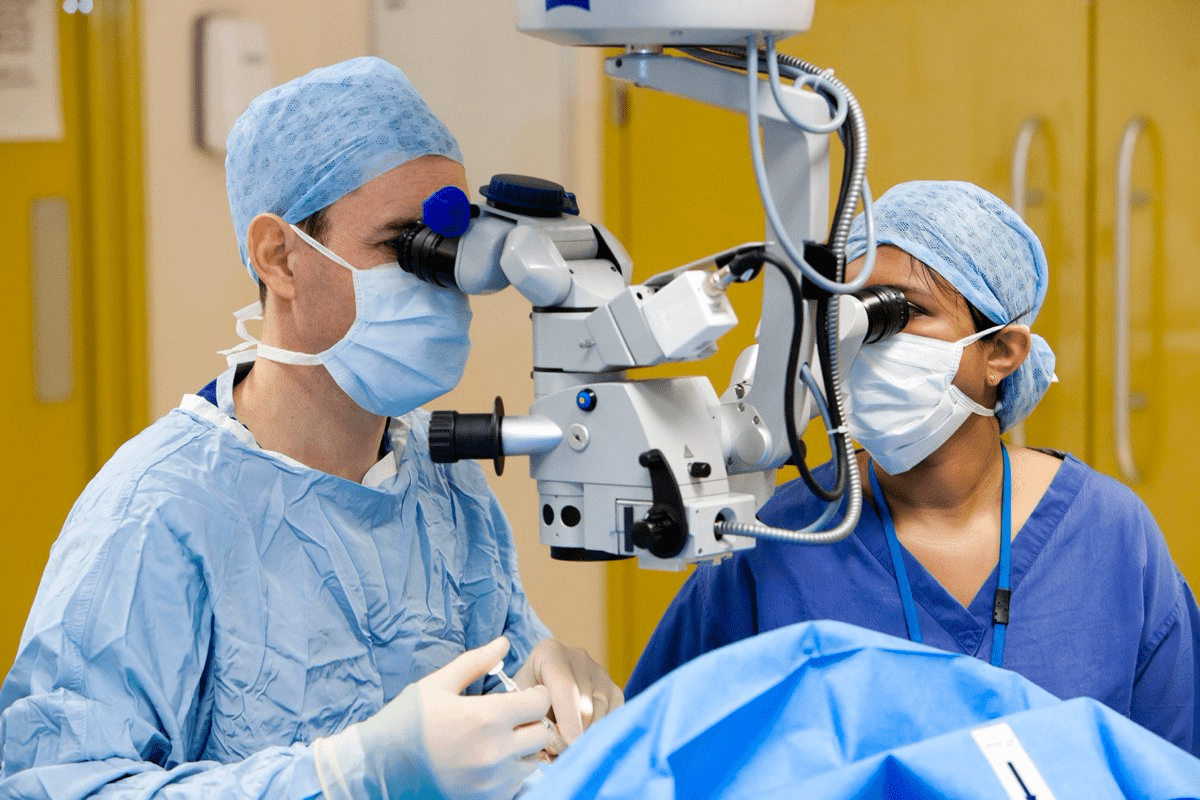
To diagnose IIH, we use a few different methods. These include checking the patient’s health, using special brain scans, and looking at the fluid in the brain. Our team uses the latest technology and works together to make sure we get it right.
We start by looking at the patient’s medical history and doing a physical check-up. Then, we do eye exams, brain scans, and a procedure called a lumbar puncture. This helps us figure out if it’s IIH or something else. It also helps us stop vision problems from getting worse.
Understand the diagnostic criteria for idiopathic intracranial hypertension. Our guide covers the modified Dandy criteria.
Key Takeaways
- IIH diagnosis involves a combination of clinical assessment, neuroimaging, and CSF analysis.
- Accurate diagnosis is key to managing IIH and stopping vision loss.
- Liv Hospital uses advanced diagnostic imaging technology and multidisciplinary evaluation.
- The diagnostic process includes medical history, physical examination, ophthalmologic examination, and lumbar puncture.
- Our team is dedicated to providing complete care for international patients.
Understanding Idiopathic Intracranial Hypertension
Idiopathic intracranial hypertension (IIH) is a condition where the pressure inside the skull goes up without a known reason. It’s also known as pseudotumor cerebri or benign intracranial hypertension. This condition is different because it doesn’t have a clear cause.
Definition and Terminology
IIH is when the pressure in the skull goes up without a clear reason. This is different from other causes of high pressure in the skull. The term “idiopathic” means we don’t know the cause.
The term pseudotumor cerebri is used because IIH can seem like a brain tumor. But, there’s no actual tumor. This makes diagnosing IIH tricky because its symptoms can be like other serious brain conditions.
Epidemiology and Risk Factors
IIH is not very common. It mostly affects women who are overweight or obese. Studies show that most people with IIH are overweight or obese.
Risk Factor | Description |
Obesity | Strongly associated with an increased risk of developing IIH. |
Female Gender | IIH predominantly affects women, specially those of childbearing age. |
Age | Typically affects individuals between the ages of 20 and 50. |
A leading researcher said,
“The link between obesity and IIH is significant, suggesting that weight management could be a key part of managing the condition.”
Pathophysiology of Increased Intracranial Pressure
IIH happens when too much cerebrospinal fluid (CSF) builds up in the skull. This increases the pressure on the brain and optic nerve. It can cause vision problems and other brain symptoms.
We don’t fully understand why IIH happens. But, it’s thought that problems with CSF absorption and increased venous pressure might play a role.
Understanding how IIH works is key to finding better ways to diagnose and treat it. By studying the factors that cause IIH, we can improve care and outcomes for patients.
Clinical Presentation of IIH
Understanding IIH symptoms is key for correct diagnosis and treatment. IIH symptoms can vary and affect many areas of health.
Common Symptoms and Signs
People with IIH often have headaches, visual problems, and other neurological signs. These symptoms can greatly reduce quality of life and need quick medical care.
- Headaches are a common complaint, often described as severe and debilitating.
- Visual disturbances, such as blurred vision or double vision, are also frequently reported.
- Other neurological symptoms may include tinnitus, dizziness, and neck pain.
Headache Characteristics
The headaches of IIH are known for their severity and frequency. They are often described as:
- Worsening in the morning or when lying down
- Associated with nausea and vomiting
- Exacerbated by activities that increase intrathoracic pressure, such as coughing or straining
Visual Disturbances
Visual problems are a key symptom of IIH, caused by increased pressure on the optic nerves. Common complaints include:
- Blurred vision
- Double vision (diplopia)
- Transient visual obscurations
These visual issues can be short-term or long-lasting and can greatly affect daily life.
Other Neurological Manifestations
Besides headaches and visual issues, IIH patients may have other neurological symptoms. These can include:
- Tinnitus, often described as a pulsatile sound
- Dizziness or vertigo
- Neck pain or stiffness
Spotting these symptoms is vital for diagnosing IIH and telling it apart from other conditions.
Diagnostic Criteria for Idiopathic Intracranial Hypertension
To diagnose idiopathic intracranial hypertension, we use a detailed method. This method includes clinical signs, patient history, and tests. It helps us accurately identify IIH.
Modified Dandy Criteria
The Modified Dandy Criteria are key for diagnosing IIH. They look for symptoms like headache and papilledema. Also, they check for normal cerebrospinal fluid (CSF) and high CSF pressure.
Key components of the Modified Dandy Criteria:
- Symptoms of raised intracranial pressure
- No localizing neurological signs except for sixth nerve palsy
- Normal CSF composition
- Elevated CSF pressure
- Normal neuroimaging studies
Friedman Criteria (2013)
In 2013, the Friedman Criteria updated the IIH diagnosis. They focus on detailed neuroimaging and CSF pressure measurement.
The Friedman Criteria highlight the need for:
- Symptoms and signs of IIH
- Normal neurological examination except for papilledema and possible sixth nerve palsy
- Normal CSF composition
- Elevated lumbar CSF pressure
- Normal neuroimaging
Opening Pressure Thresholds
Opening pressure thresholds are vital for IIH diagnosis. A lumbar puncture showing an opening pressure over 25 cm CSF is key. It must have normal cerebrospinal fluid.
Understanding Opening Pressure:
The opening pressure is measured during a lumbar puncture. It’s important to have the patient relaxed and in the right position for an accurate reading.
Diagnostic Algorithm
We use a detailed algorithm for diagnosing IIH. It includes the Modified Dandy Criteria, Friedman Criteria, and opening pressure thresholds. This approach helps us accurately identify IIH patients.
By applying these criteria carefully, we ensure patients get the right diagnosis and treatment for IIH.
Neurological Examination in IIH Diagnosis
A detailed neurological examination is key for diagnosing Idiopathic Intracranial Hypertension (IIH). It helps doctors spot important signs of IIH. This leads to more tests and treatment plans.
Fundoscopic Examination and Papilledema
The fundoscopic examination is vital for IIH diagnosis. Papilledema, or swelling of the optic disc, is a key sign of increased pressure inside the skull. It’s found in most IIH patients.
We do fundoscopy to look for papilledema and other eye problems that might show IIH. Finding papilledema is a big help in diagnosing IIH.
In the fundoscopic exam, we search for papilledema signs like swelling, hemorrhages, or exudates. The severity of papilledema shows how bad the pressure is.
Visual Field Testing
Visual field testing is also key in diagnosing IIH. It checks the patient’s vision, looking for any defects or blind spots caused by high pressure. Visual field defects can happen because of papilledema or other IIH-related issues.
We use different methods for visual field tests, like confrontation tests or automated perimetry. These tests measure vision loss and track changes.
Cranial Nerve Assessment
Cranial nerve assessment is important for IIH patients. We check the function of nerves controlling eye movements (cranial nerves III, IV, and VI). This helps find any problems.
Abducens nerve palsy, for example, can cause double vision in IIH patients. A detailed nerve check helps find any IIH-related deficits, guiding treatment.
Neuropsychological Evaluation
Neuropsychological evaluation might also be part of the IIH assessment. It checks cognitive functions like attention, memory, and executive functions. This helps find any cognitive problems linked to IIH.
Even though IIH mainly affects vision and nerves, some patients might have cognitive symptoms. Neuropsychological tests help understand how IIH affects the brain.
Neuroimaging Studies
Neuroimaging studies are key in diagnosing IIH. They help find or rule out structural causes and venous sinus thrombosis. MRI and CT scans are vital in this process.
MRI Findings in IIH
MRI is a top tool for spotting IIH. It helps rule out other causes of high pressure in the brain. Common MRI signs include:
- Empty sella turcica
- Flattening of the posterior globe
- Distension of the perioptic subarachnoid space
- Tortuosity of the optic nerve
These signs show high pressure in the brain.
MR Venography
MR venography checks the cerebral venous sinuses. It helps find out if there’s a blood clot causing high pressure. It’s a key part of diagnosing IIH.
CT Scan and CT Venography
CT scans are first used to check for other causes of headaches and vision problems. CT venography looks at the cerebral venous sinuses like MR venography does.
Radiological Signs of Increased Intracranial Pressure
Several signs on neuroimaging studies show high pressure in the brain. These include:
Radiological Sign | Description |
Empty Sella Turcica | A condition where the sella turcica appears empty due to herniation of the arachnoid membrane. |
Flattening of the Posterior Globe | A sign of increased intracranial pressure causing deformation of the eyeball. |
Optic Nerve Sheath Distension | Distension of the subarachnoid space around the optic nerve, indicative of increased pressure. |
These findings are vital for diagnosing and managing IIH. They help tell it apart from other causes of headaches and vision problems.
Lumbar Puncture and CSF Analysis
A lumbar puncture is done to check the pressure and composition of cerebrospinal fluid (CSF). It’s a key step in diagnosing IIH. This procedure, also known as a spinal tap, is vital for assessing idiopathic intracranial hypertension.
Opening Pressure Measurement Technique
The opening pressure measurement is a key part of the lumbar puncture. It measures the pressure when CSF starts flowing out. Proper technique is essential for accurate readings.
The patient lies on their side, and the puncture is done at the L3-L4 or L4-L5 space. A manometer is used to measure the opening pressure in cm of CSF.
Interpreting CSF Pressure Values
In adults, normal opening pressure is between 6 to 20 cm CSF. In IIH, this pressure is usually higher, over 25 cm CSF. It’s important to understand these values in the context of the patient’s symptoms.
Pressure Range (cm CSF) | Interpretation |
6-20 | Normal |
21-24 | Borderline Elevated |
>25 | Elevated (suggestive of IIH) |
CSF Composition Analysis
The CSF is also analyzed for its composition. In IIH, the CSF is usually normal. This helps rule out other causes of high pressure in the brain.
“The cerebrospinal fluid analysis in idiopathic intracranial hypertension is usually normal, with no evidence of infection, inflammation, or malignancy.”
Procedural Considerations and Complications
Lumbar puncture is generally safe, but there are risks. These include headache, infection, and brainstem herniation in rare cases. Careful patient selection and technique can reduce these risks.
Headache after the procedure is common. It can be treated with conservative methods or sometimes with an epidural blood patch.
Differential Diagnosis and Exclusion Criteria
To diagnose IIH, it’s key to rule out other causes of high pressure in the brain. This means checking for and excluding different conditions that might look like IIH.
Secondary Causes of Intracranial Hypertension
There are many reasons why intracranial pressure might go up. These include problems with blood vessels, tumors, infections, and other issues.
- Vascular causes: Venous sinus thrombosis, arteriovenous malformations
- Neoplastic causes: Brain tumors, meningiomas
- Infectious causes: Meningitis, encephalitis
Venous Sinus Thrombosis
Venous sinus thrombosis is a serious condition that can look like IIH. It happens when a blood clot forms in the dural venous sinuses, raising pressure in the brain.
Diagnostic Features:
- MR venography showing absence of flow in the affected sinus
- Headache, often thunderclap in nature
- Seizures or focal neurological deficits
Condition | Diagnostic Features | Treatment Approach |
Venous Sinus Thrombosis | MRV showing absent flow, headache, seizures | Anticoagulation, thrombolysis |
Medication-Induced IIH | History of offending medication, elevated ICP | Withdrawal of offending drug, ICP management |
Medication-Induced Intracranial Hypertension
Some medicines can cause high pressure in the brain, making it seem like IIH. These include tetracyclines, vitamin A derivatives, and corticosteroids.
Management:
- Withdrawal of the offending medication
- Monitoring of intracranial pressure
- Alternative treatments for the underlying condition
Other Conditions Mimicking IIH
Other conditions like sleep apnea, chronic meningitis, and cerebral venous sinus thrombosis can also look like IIH. It’s important to do a detailed check to tell them apart from IIH.
Knowing how to tell IIH apart from other conditions helps doctors give the right care to patients with this complex issue.
Special Diagnostic Considerations
Accurate diagnosis of IIH is key in different patient groups. It’s complex because IIH shows up in many ways and can be mistaken for other conditions.
IIH Without Papilledema
Diagnosing IIH without papilledema is tough. We look at other signs like high CSF pressure and symptoms like headaches and vision problems.
- Checking CSF pressure is very important.
- Imaging, like MRI, helps find other causes.
- Visual field tests are key for spotting vision issues.
Pediatric IIH Diagnosis
Diagnosing IIH in kids is different. It needs special care because kids show symptoms in unique ways.
Important points include:
- Using the right diagnostic criteria for kids.
- Using gentle tests that kids can handle.
- Watching for how IIH affects their growth and vision.
Diagnosis in Atypical Presentations
IIH can show up in unusual ways, like without headaches or with strange symptoms. This needs a careful look and detailed tests.
We must think about:
- Other conditions that might look like IIH.
- The use of new imaging methods.
- The value of a full medical history and exam.
Emerging Diagnostic Technologies
New tech like advanced MRI and new CSF tests are helping us spot IIH better.
These new tools bring:
- Better accuracy in diagnosis.
- Deeper understanding of IIH.
- Chance for catching it sooner and treating it faster.
Conclusion
Getting a correct diagnosis is key to managing idiopathic intracranial hypertension (IIH) well. We’ve talked about how hard it is to diagnose IIH. It’s important to use a full approach that includes checking the patient, imaging the brain, and analyzing the cerebrospinal fluid (CSF).
Understanding what causes high pressure inside the skull and the signs of IIH is vital. This knowledge helps doctors make the right diagnosis. With the right diagnosis, they can create better treatment plans. This helps improve how well patients do with IIH.
There are treatments available that can help manage IIH symptoms and stop vision loss. This shows how important it is to diagnose IIH quickly and accurately. By working together, we can give better care to those with IIH.
FAQ
What is idiopathic intracranial hypertension (IIH)?
Idiopathic intracranial hypertension (IIH) is a condition where the pressure inside the skull goes up without a known reason. It often causes headaches and problems with vision.
What are the diagnostic criteria for IIH?
To diagnose IIH, doctors use the modified Dandy and Friedman criteria. These include symptoms of high pressure in the skull, high cerebrospinal fluid (CSF) pressure, and normal CSF composition.
How is opening pressure measured during a lumbar puncture?
Opening pressure is measured during a lumbar puncture. It’s the pressure of the CSF as it first flows out. This is done when the person is relaxed and lying down.
What is considered a normal opening pressure?
A normal opening pressure is usually below 25 cm H2O in adults. But, it can vary a bit based on the situation and how the patient is positioned.
What are the common symptoms of IIH?
Symptoms of IIH include headaches, vision problems like transient visual obscurations, double vision, and pulsatile tinnitus.
How is IIH differentiated from other causes of intracranial hypertension?
IIH is diagnosed by ruling out other causes of high pressure in the skull. This is done through clinical evaluation, neuroimaging studies, and CSF analysis.
Can IIH occur without papilledema?
Yes, IIH can happen without papilledema. But, papilledema is common in many cases. The diagnosis in such cases relies on other clinical and diagnostic criteria.
What role do neuroimaging studies play in diagnosing IIH?
Neuroimaging studies, like MRI and MR venography, are key. They help rule out other causes of high pressure and show signs of increased pressure in the skull.
Are there any specific considerations for diagnosing IIH in children?
Diagnosing IIH in children needs special care. This includes knowing the normal values for opening pressure in children and being aware of differences in symptoms.
What emerging diagnostic technologies are being explored for IIH?
New technologies for diagnosing IIH include advanced imaging and other innovative methods. These aim to improve how accurately we can diagnose and understand IIH.
What is the significance of accurate diagnosis in managing IIH?
Accurate diagnosis is key to managing IIH well. It lets doctors use the right treatments to lower pressure and ease symptoms. This improves patient outcomes.
References
National Center for Biotechnology Information. Diagnosing Idiopathic Intracranial Hypertension: A Guide. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6778406/