We are dedicated to top-notch healthcare for everyone. At Liv Hospital, we use the latest Optical Coherence Tomography (OCT) tech. This helps us spot and treat epiretinal membrane (ERM), a common eye problem.How to read epiretinal membrane on OCT. This guide explains 5 key findings for ophthalmologists to identify ERM.
It’s key for eye doctors to know how to read OCT scans for ERM. This knowledge helps them make better choices for their patients. With OCT, we give the best care to those with ERM, making sure they get the right treatment.
Key Takeaways
- ERM is a fibrocellular tissue that grows on the retina’s inner side.
- OCT is the top choice for diagnosing ERMs.
- Knowing about ERM and its effects on the macula is vital for doctors.
- Liv Hospital follows the latest academic guidelines for ERM diagnosis and treatment.
- Using OCT for ERM management leads to better patient results.
The Clinical Spectrum of Epiretinal Membrane

Understanding ERM is key for good care. ERM is when a membrane forms on the retina’s inner side. It can mess with your vision and life quality.
Definition and Terminology: Macular Pucker and Cellophane Maculopathy
ERM is also known as macular pucker and cellophane maculopathy. These names describe how the retina looks with ERM. Macular pucker means the membrane tightens, making the retina wrinkle. Cellophane maculopathy makes the retina look like cellophane.
Even though there are different names, they all mean the same thing. Using the right words helps doctors talk clearly and make accurate diagnoses.
Epidemiology and Risk Factors
ERM is quite common, with most cases being idiopathic. This means about 95% of ERMs have no known cause. Other ERMs happen because of eye diseases, injuries, or surgeries.
Risk Factor | Description | Association with ERM |
Retinal Vascular Diseases | Diseases affecting the blood vessels of the retina | Secondary ERM |
Retinal Vein Occlusion | Blockage of the retinal veins | Secondary ERM |
Ocular Inflammatory Disease | Inflammation within the eye | Secondary ERM |
Trauma | Physical injury to the eye | Secondary ERM |
Intraocular Surgery | Surgical procedures within the eye | Secondary ERM |
Knowing about ERM’s causes is vital. It helps doctors diagnose and treat it better. This leads to better results for patients.
Optical Coherence Tomography: Gold Standard for ERM Diagnosis
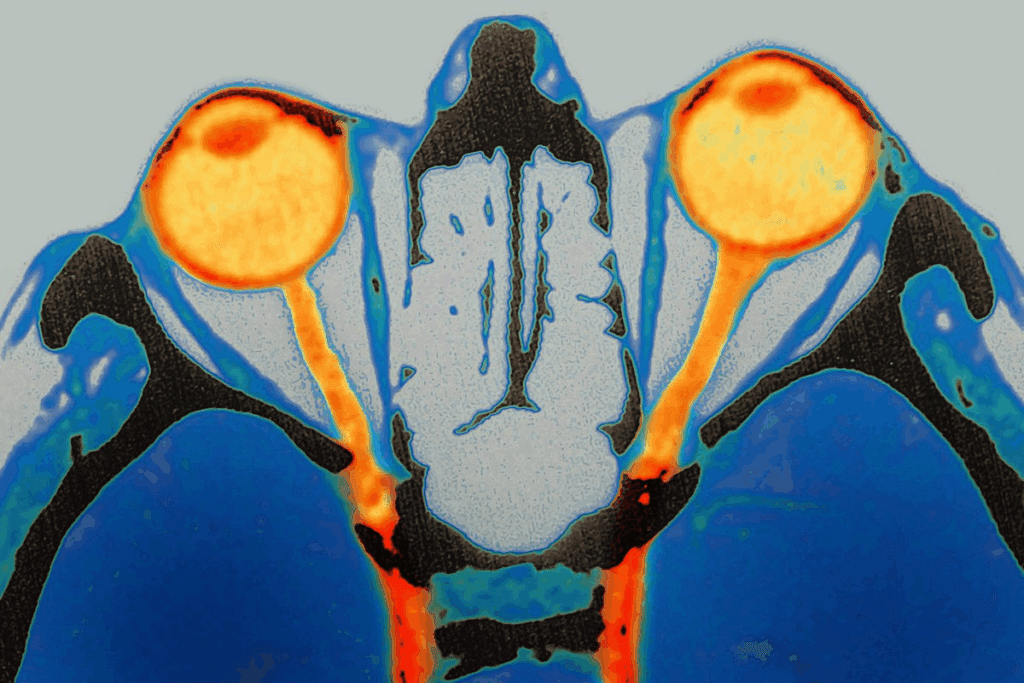
OCT technology has made diagnosing ERM more accurate. It gives high-resolution images of the retina. This makes it key for spotting Epiretinal Membrane (ERM).
High-resolution OCT lets us see the macula in 3D and cross-section. This boosts our ability to spot and manage ERM. The tech has evolved from time-domain to spectral-domain OCT, giving clearer images and more detailed info.
Evolution from Time-Domain to Spectral-Domain OCT
The switch from time-domain OCT (TD-OCT) to spectral-domain OCT (SD-OCT) has improved ERM diagnosis. SD-OCT offers better image quality and scans faster than TD-OCT. This lets doctors spot even small changes in the retina.
SD-OCT is now the top choice for finding ERM. It shows detailed images of the retina and any ERM-related issues. This tech has helped us understand ERM better and its effects on the retina.
Sensitivity Comparison: OCT vs. Clinical Examination
OCT is more sensitive than clinical exams for ERM diagnosis. Clinical exams rely on symptoms and biomicroscopic findings. These might miss early or subtle ERM. But OCT can spot ERM early, even before symptoms or signs appear.
OCT’s sensitivity in finding ERM makes it vital in ophthalmology. It allows for early treatment and could improve patient results. OCT gives a clear view of the retina. This helps doctors track ERM and decide on treatment.
Normal Macular Anatomy on OCT: A Reference Point
To accurately diagnose and manage ERM, it’s essential to understand the normal macular anatomy on OCT. The macula is key for central vision and fine detail. Knowing its normal structure helps spot changes due to ERM.
Identifying Retinal Layers and Landmarks
On OCT, the normal macula shows as a layered structure. We can spot several key layers. These include the retinal nerve fiber layer and the retinal pigment epithelium. Each layer is vital for vision.
“The retina is not just a simple layer; it’s a complex neural tissue that converts light into signals that are interpreted by the brain,” as noted by experts in the field of ophthalmology. Recognizing these layers on OCT is fundamental for diagnosing ERM and understanding its impact on retinal anatomy.
Normal Foveal Contour and Thickness Parameters
The fovea, at the macula’s center, has a depression called the foveal pit. On OCT, this depression looks smooth and symmetrical. The retina’s thickness here is also important, with normal values ranging from 138 to 250 microns.
When we look at the macula on OCT, we must check for ERM and its effect on the retina. By comparing the affected area to normal anatomy, we can understand the pathology’s extent. This helps us plan the right treatment.
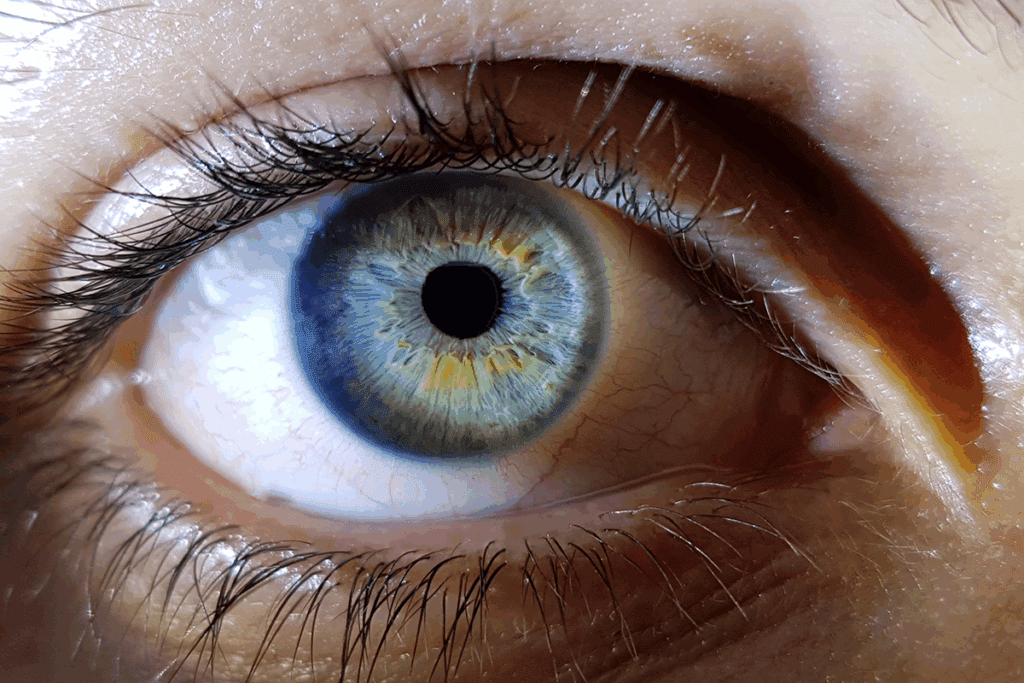
Epiretinal Membrane on OCT: Characteristic Appearance and Patterns
Epiretinal membrane on OCT is a key sign for doctors to spot and treat this issue. An OCT scan shows a clear band on the retina’s inner layer. This band is a sign of ERM.
Hyperreflective Band on Inner Retinal Surface
The ERM band looks like a thin, bright line on the retina’s inner side. It shows where fibrocellular growth is happening. The band’s size and shape tell us how severe the ERM is.
ERM can also cause other changes in the retina, like thickening or edema. These changes help doctors understand how ERM affects vision and eye health.
Classification of ERM Severity on OCT
Doctors use OCT to grade ERM’s severity. They look at the membrane’s thickness, how well it sticks to the retina, and any other changes. This system helps doctors talk clearly about ERM with each other.
- Mild ERM: Thin membrane with little retinal change.
- Moderate ERM: Thicker membrane with more noticeable changes.
- Severe ERM: Big changes in the retina and often edema.
By grading ERM, doctors can link what they see on scans to how it affects patients. This helps them make better treatment plans and care for patients better.
Key Finding #1: Central Foveal Thickness Measurements
When we diagnose Epiretinal Membrane (ERM), we look closely at the Central Foveal Thickness (CFT). This is done using Optical Coherence Tomography (OCT). CFT helps us understand how severe ERM is and its effect on the macula.
Normal vs. Pathological CFT Ranges
CFT measurements usually range from 138 to 702 microns in ERM patients. Knowing the normal and abnormal ranges is key for a correct diagnosis. Normal CFT values are between 245 to 255 microns. But, this can change a bit depending on the OCT device and the study population.
Abnormal CFT values mean the retina is not healthy, like in ERM. We’ve seen that higher CFT often means more severe symptoms in our patients.
Correlation Between Increased CFT and Visual Symptoms
There’s a strong link between higher CFT and visual problems. Studies show that bigger CFT values lead to worse vision. This includes metamorphopsia and lower visual acuity.
We use CFT to decide if surgery is needed. By watching CFT changes, we see how ERM is progressing and if treatment is working. This helps us make better choices for our patients.
Key Finding #2: Inner Segment Ellipsoid Band Integrity
The inner segment ellipsoid band is key in checking how bad an epiretinal membrane (ERM) is. This band, or IS/OS junction, is important for the retina to work right. Looking at this band on OCT helps see how ERM affects the retina.
Assessment Methods for IS/OS Junction Disruption
To check the IS/OS junction, several methods are used. High-resolution OCT imaging shows the retinal layers clearly, including the inner segment ellipsoid band. The damage can be measured by its length or as a percentage in an area.
Assessment Techniques:
- Manual measurement of disruption length
- Automated software analysis for quantification
- Qualitative assessment of disruption severity
These methods help understand the IS/OS junction disruption well. This is key for knowing how well a patient will do and planning treatment for ERM.
Assessment Method | Description | Clinical Utility |
Manual Measurement | Direct measurement of IS/OS disruption length | High accuracy, but time-consuming |
Automated Software Analysis | Quantification of disruption using OCT software | Fast and efficient, but may require validation |
Qualitative Assessment | Visual grading of disruption severity | Quick and simple, but subjective |
Clinical Relevance in Visual Prognosis
Checking the inner segment ellipsoid band’s health is important for knowing how well a patient will see. Studies show that big damage to this band means worse vision. So, looking at this band helps predict how well surgery will work and what to tell patients about their vision.
Knowing how much damage there is helps doctors set realistic hopes for patients. It also helps decide the best treatment for ERM.
Key Finding #3: Maximal Retinal Thickness as a Predictive Biomarker
In diagnosing ERM, maximal retinal thickness (MRT) is key. It’s measured with OCT. This helps us understand how well a patient can see.
Measurement Protocols for MRT
Getting MRT right is important. We use OCT to check the retina’s thickness. Here’s how we do it:
- Find the thickest part of the retina on the OCT scan
- Make sure the scan is over the fovea
- Measure from the inner limiting membrane to Bruch’s membrane with software calipers
Being consistent in measuring MRT is vital. We use the same OCT and method for all scans. This helps us get accurate results.
Correlation with Visual Acuity Outcomes
Research links MRT to how well patients can see. A thicker retina often means worse vision. Here’s what we’ve found:
MRT Range (microns) | Visual Acuity Outcome | Clinical Implication |
300-400 | Mild impairment | Monitoring recommended |
400-600 | Moderate impairment | Surgical consideration |
>600 | Severe impairment | Surgery often necessary |
This link helps us guess how well a patient will see. It guides our treatment choices. We tell patients what to expect and if surgery might help.
Key Finding #4: Disorganization of Retinal Inner Layers (DRIL)
OCT scans show DRIL, giving us clues about ERM’s severity and how it might affect vision. It’s key to know how to spot DRIL, grade its severity, and what it means for the future.
Identification and Grading of DRIL Severity
DRIL messes with the inner layers of the retina. On an OCT scan, we look for where these layers get mixed up or lost. The more disrupted, the worse the DRIL.
Doctors grade DRIL by how much it messes with the inner layers. Research shows this messiness affects how well a person can see. So, knowing how bad DRIL is helps predict how well a patient might see again.
DRIL as a Negative Prognostic Factor for Visual Recovery
Severe DRIL means a patient might not see as well after treatment for ERM. How much DRIL there is can affect how well a person can see. This makes it a key thing to check on an OCT scan.
Knowing about DRIL helps doctors talk to patients about what to expect. It shows how important detailed OCT scans are in treating ERM.
By checking DRIL on OCT scans, we can guess better how well a patient will see. This helps doctors plan the best treatment for ERM patients. It shows how important detailed scans are for good care.
Key Finding #5: Membrane-Retina Separation Characteristics
It’s key for eye doctors to know how the epiretinal membrane (ERM) and retina separate. This helps them plan surgery better. The way ERM sticks to the retina affects how hard surgery will be.
Adhesion Patterns Between ERM and Retinal Surface
How ERM sticks to the retina can differ a lot between people. Optical Coherence Tomography (OCT) lets us see these patterns clearly. We can tell if ERM sticks well or if there are gaps.
This info is key for planning surgery. The patterns can be different, like some ERMs sticking a lot or just in a few spots. Knowing this before surgery helps doctors prepare for challenges.
Implications for Surgical Complexity and Outcomes
The way ERM and retina separate affects how hard surgery is and how well it goes. ERMs that stick a lot can be harder to remove and might lead to more problems. But, those that stick less can be easier to take off.
Research shows that preoperative OCT assessment helps predict how hard surgery will be and how well the eye will do after. Knowing these details helps doctors talk to patients about what to expect. It also helps choose the right tools and methods for surgery.
In short, looking closely at how ERM and retina separate on OCT is very helpful. It helps doctors plan and do surgery better, which improves how well patients do.
Advanced OCT Technologies in ERM Assessment
Advanced OCT technologies are key in understanding and treating epiretinal membrane (ERM). These new tools help us see how ERM affects the retina. We’ll look at how OCT angiography and en face OCT improve ERM diagnosis.
OCT Angiography for Vascular Changes in ERM
OCT angiography shows the retina’s blood vessels without dye. It’s great for spotting changes in ERM, like changes in the foveal avascular zone and vessel density.
Vascular changes observed using OCT angiography include:
- Alterations in the foveal avascular zone
- Changes in retinal vessel density
- Potential ischemia or vascular remodeling
En Face OCT and 3D Reconstruction Techniques
En face OCT gives a direct view of the retina, showing ERM’s size and shape. With 3D reconstruction, it lets us see ERM’s details and how it interacts with the retina.
The table below shows how en face OCT and 3D reconstruction help with ERM assessment:
Feature | Benefit |
Topographical Analysis | Detailed assessment of ERM extent and morphology |
Relationship with Retina | Understanding ERM’s interaction with underlying retinal layers |
Surgical Planning | Aids in planning surgical interventions by visualizing ERM’s topography |
Advanced OCT technologies, like OCT angiography and en face OCT, give a full view of ERM’s effects on the retina and blood vessels.
Post-Surgical OCT Evaluation and Monitoring
OCT helps doctors keep an eye on ERM patients’ retinal health after surgery. This advanced imaging is key for checking how the retina changes after ERM surgery. It lets doctors see how well the patient is recovering and spot any issues early on.
Early Post-Operative OCT Findings
Right after ERM surgery, OCT shows what changes have happened. These can include:
- Residual or recurrent ERM
- Cystoid macular edema
- Retinal layer disruption
- Changes in retinal thickness
Spotting these issues early is important for deciding on the next steps. For example, if there’s cystoid macular edema, doctors might need to use anti-VEGF injections.
Long-Term Structural Recovery Patterns
Long-term OCT scans show how the retina changes over time after ERM surgery. Important things to notice are:
- Gradual normalization of retinal thickness
- Improvement in retinal layer integrity
- Potential for visual acuity improvement
The erm retina and erm macular changes seen on OCT are very important. They tell doctors how well the surgery worked and what the patient’s future looks like. Knowing these long-term changes helps doctors give better care and manage what patients can expect.
In short, OCT is a vital tool for managing retina epiretinal membrane cases after surgery. By using OCT, doctors can make sure patients get the best care possible and improve their outcomes.
Conclusion: Integrating OCT Findings into Clinical Practice
We’ve seen how important Optical Coherence Tomography (OCT) is for diagnosing and treating epiretinal membrane (ERM). OCT shows ERM as a bright band on the inner retina. This helps doctors a lot.
Doctors can use OCT to measure the retina’s thickness and check its health. This helps them decide the best treatment and predict how well a patient will see. Using OCT makes treating ERM better and helps patients more.
Advanced OCT tools like OCT angiography and en face OCT help us learn more about ERM. As we get better at understanding ERM on OCT, we can make treatments even better. This means better eyesight for patients with ERM.
To use OCT well in treating ERM, doctors need to know a lot about ERM OCT images. This knowledge helps them give the best care to patients with ERM.
FAQ
What is an epiretinal membrane (ERM) and how is it diagnosed?
An epiretinal membrane (ERM) is a condition where a layer of fibrous tissue forms on the retina. It is diagnosed using Optical Coherence Tomography (OCT). OCT is the best tool for spotting ERM because it shows the retina’s details clearly.
What are the different types of ERM and their associated risk factors?
There are two types of ERM: idiopathic and secondary. Idiopathic ERM has no known cause. Secondary ERM is linked to other eye problems or surgeries. Risk factors include age, retinal detachment, and previous eye surgery.
How does OCT technology improve ERM diagnosis compared to clinical examination?
OCT gives a detailed view of the retina. It can spot ERM and its severity better than just looking at the eye. This makes OCT a key tool for diagnosing ERM.
What is the normal macular anatomy on OCT, and why is it important?
Normal macular anatomy on OCT shows clear retinal layers and a specific foveal shape. Knowing this is key to spotting ERM changes and judging its severity.
How is ERM severity classified on OCT?
ERM severity is judged by the look of the inner retinal surface, central foveal thickness, and the state of the inner segment ellipsoid band. These factors help determine how severe the ERM is.
What is the significance of central foveal thickness (CFT) measurements in ERM diagnosis?
CFT measurements are important for judging ERM severity. Higher CFT values are linked to vision problems. Measuring CFT helps track the condition’s progress and plan treatment.
How does the integrity of the inner segment ellipsoid band affect visual prognosis in ERM?
The inner segment ellipsoid band’s condition is a big factor in ERM patients’ vision recovery. Damage to this band often means worse vision outcomes.
What is the role of maximal retinal thickness (MRT) as a predictive biomarker in ERM?
MRT is a biomarker for predicting vision recovery in ERM patients. It helps assess the chance of vision improvement after treatment.
What is disorganization of retinal inner layers (DRIL), and how does it impact visual recovery?
DRIL is when the inner retinal layers get disrupted. It’s a bad sign for vision recovery in ERM patients, suggesting a less favorable outcome.
How do adhesion patterns between ERM and the retinal surface affect surgical outcomes?
The strength of adhesion between ERM and the retina can make surgery more complex. Stronger adhesions can make it harder to remove the ERM.
What advancements in OCT technology are being used for ERM assessment?
New OCT tech includes OCT angiography for vascular changes and en face OCT with 3D reconstruction. These advancements offer detailed views of ERM and its effects on the retina.
How is OCT used in post-surgical evaluation and monitoring of ERM patients?
OCT helps check early changes and long-term recovery in ERM patients after surgery. It’s key for monitoring surgery success and guiding further care.
What is the importance of incorporating OCT findings into clinical practice for ERM management?
Using OCT findings in patient care is vital. It ensures accurate diagnosis, severity assessment, and monitoring of ERM. This guides treatment decisions and improves patient outcomes.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/40359403/








