An epiretinal membrane is a condition where a layer of cells forms on the retina’s surface. This can cause vision problems. Many people don’t know they have it until a routine eye exam.What is ERM ophthalmology? This ultimate guide explains epiretinal membrane, its causes, symptoms, and treatment.
We will look into the causes, symptoms, and treatments for epiretinal membrane. This will help you understand this common eye condition. We’ll also talk about what to do if you’re diagnosed with it.
Key Takeaways
- Understanding what epiretinal membrane is and how it’s diagnosed.
- Recognizing the symptoms that may indicate the presence of a membrane in the eyes.
- Exploring treatment options available for epiretinal membrane.
- Learning how to manage vision problems caused by this condition.
- Understanding the importance of regular eye exams for early detection.
Understanding Epiretinal Membrane
Epiretinal membrane, also known as macular pucker or cellophane maculopathy, is a layer of fibrous tissue on the retina. It affects the macula, which is key for central vision and fine detail.
Definition and Alternative Names
Epiretinal membrane (ERM) is a fibrocellular layer on the retina’s surface, over the macula. It can cause visual disturbances by distorting the retina and affecting light focus on photoreceptors.
Other names for ERM include:
- Macular pucker
- Cellophane maculopathy
- Premacular fibrosis
These names highlight the condition’s impact on the macula and the membrane’s appearance.
Anatomy of the Retina and Macula
The retina is a complex neural tissue inside the eye. It’s vital for vision, converting light into neural signals for the brain. The macula, at the retina’s center, handles:
- Central vision
- Fine detail vision
- Color vision
The macula has many photoreceptor cells. It’s key for sharp, straight-ahead vision, like reading and driving.
Epidemiology and Prevalence
ERM is more common in older adults, with prevalence rising with age. Studies show:
- ERM incidence increases after 50.
- By 70, many have ERM.
Knowing ERM’s epidemiology is key for prevention and treatment, mainly in older populations.
ERM in Ophthalmology: Pathophysiology and Classification

It’s important to know how Epiretinal Membrane (ERM) works and how it’s classified. ERM happens when fibrocellular tissue forms on the retina’s inner side. This can cause big problems with vision.
Formation of Fibrocellular Tissue
ERM starts with myofibroblastic cells growing at the retina’s edge. These cells help make fibrocellular tissue. This tissue can shrink and pull on the retina, causing vision issues.
Grades of Epiretinal Membrane
ERM is divided into grades to show how bad it is. The grade helps decide how to treat it. Doctors look at how it looks and how it affects the retina to grade it.
- Grade 1: A thin, clear membrane.
- Grade 2: A more opaque membrane with lines on the retina.
- Grade 3: A thick membrane that really distorts the retina.
Natural History and Progression
How ERM changes over time can vary. Some stay the same, while others get worse. It’s key to watch how ERM changes to act fast. Things like how bad the membrane is and other eye problems can affect how it progresses.
Knowing about ERM’s causes and types helps doctors find better ways to treat it. This can lead to better results for patients.
Primary vs. Secondary Epiretinal Membranes
Epiretinal membranes (ERM) are divided into primary and secondary types. Each has its own causes and characteristics. Knowing these differences helps doctors diagnose and treat patients better.
Idiopathic (Age-Related) ERM
Primary ERM, or idiopathic ERM, is the most common type, making up about 95% of cases. It often affects people over 50. The exact reason for idiopathic ERM is not known, but it’s linked to aging and changes in the vitreous gel.
Posterior Vitreous Detachment
Posterior vitreous detachment (PVD) happens when the vitreous gel pulls away from the retina. It’s common with age and increases the risk of ERM. This separation can cause the retina to stretch, leading to ERM.
Secondary Causes of ERM
Secondary ERM is linked to other eye problems or events. This includes retinal diseases, inflammation, trauma, or surgery. These conditions can cause ERM as a complication or response.
The table below shows the main differences between primary and secondary ERM:
Characteristics | Primary ERM | Secondary ERM |
Cause | Idiopathic, age-related | Associated with other ocular conditions or events |
Prevalence | Approximately 95% of ERM cases | Less common, associated with specific conditions |
Risk Factors | Aging, PVD | Retinal vascular diseases, ocular inflammation, trauma, surgery |
It’s vital for doctors to know the difference between primary and secondary ERM. This helps them give the right care and treatment plans to patients.
Risk Factors for Developing Epiretinal Membrane
Several factors can increase the risk of getting Epiretinal Membrane. These include age, eye health, and overall health. Knowing these risks helps doctors spot who’s at higher risk and take steps to prevent it.
Age-Related Factors
Getting older is a big risk for Epiretinal Membrane. The risk goes up after 50. Changes in the vitreous and retina with age help create ERM. People over 60 have a 6% to 20% chance of getting ERM.
- Getting older raises the risk of ERM.
- Changes in the vitreous with age can cause ERM.
- Retinal thinning with age also plays a part.
Ocular Conditions and Procedures
Some eye problems and surgeries can raise the risk of ERM. For example, retinal detachment and diabetic retinopathy increase the risk. Cataract surgery can also lead to ERM in some cases.
- Retinal detachment is a big risk for ERM.
- Diabetic retinopathy raises the risk of ERM.
- Cataract surgery can sometimes cause ERM.
Systemic Health Conditions
Some health conditions outside the eyes can also raise the risk of ERM. Diabetes and hypertension are examples. These conditions might harm the retina and lead to ERM.
“Understanding the link between systemic health and eye health is key to managing ERM risk.”
— Ophthalmology Expert
Knowing the risks for Epiretinal Membrane helps doctors find and help at-risk patients. They can then work on prevention and treatment plans.
Common Symptoms and Clinical Presentation
Knowing the symptoms of ERM is key for early diagnosis and treatment. The signs of ERM can differ a lot from person to person. Some might have mild symptoms, while others face severe visual problems.
Visual Disturbances and Metamorphopsia
Metamorphopsia is a major symptom of ERM. It makes straight lines look distorted or wavy. This happens because of the membrane’s effect on the retina. People may also see things blurry, have double vision, or struggle with central vision.
ERM symptoms can get worse over time. Some people see their vision slowly get worse. Others might stay the same for years, but then get much worse.
Progression of Symptoms
How fast ERM symptoms get worse can vary a lot. Things like the size and location of the membrane matter. So does having other eye problems. Seeing an eye doctor regularly is important to keep track of vision changes.
Impact on Daily Activities and Quality of Life
ERM can really affect daily life and quality of life. Problems with vision can make simple tasks hard, like reading or driving. It can make people feel less independent and more frustrated. It’s important to understand how ERM affects daily life to give good care and support.
Diagnosis and Differential Diagnosis
Diagnosing ERM involves both old and new methods. It’s important to get it right to choose the best treatment and help patients.
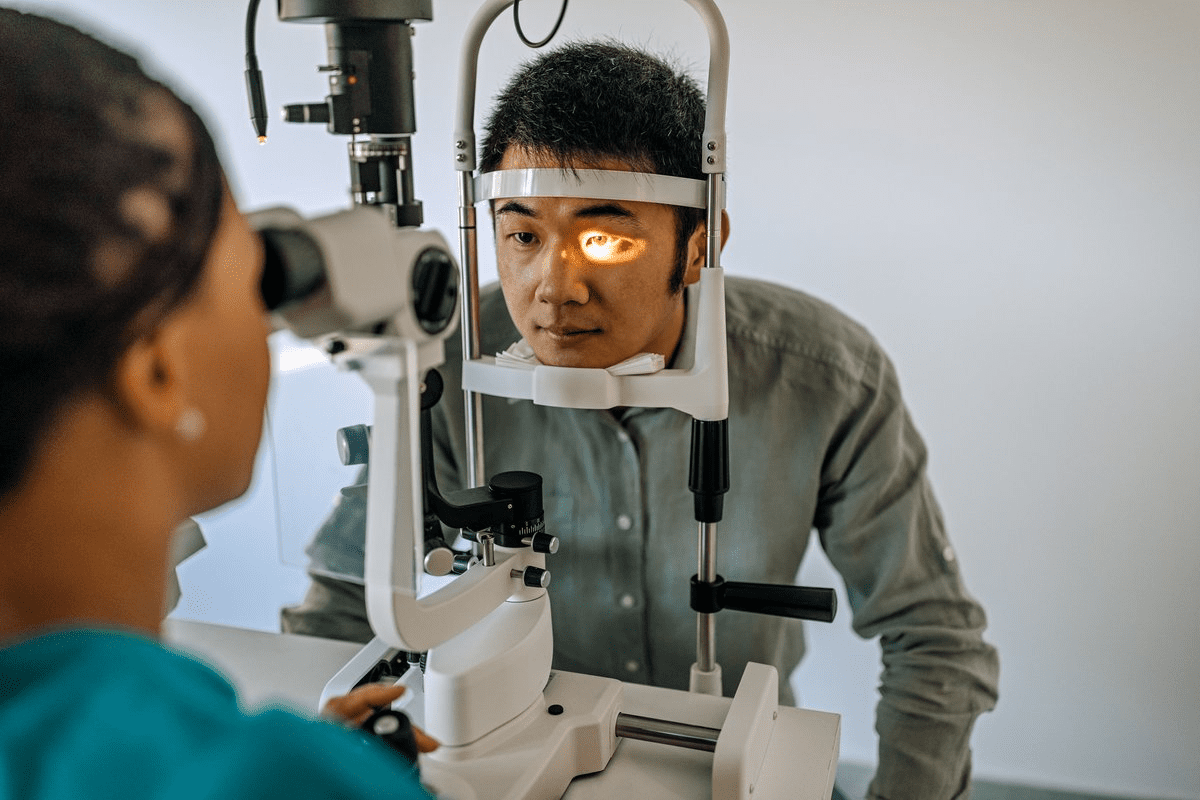
Clinical Examination Techniques
Clinical exams are key in spotting ERM. They include:
- Slit-lamp exams to check the front part of the eye and rule out other issues.
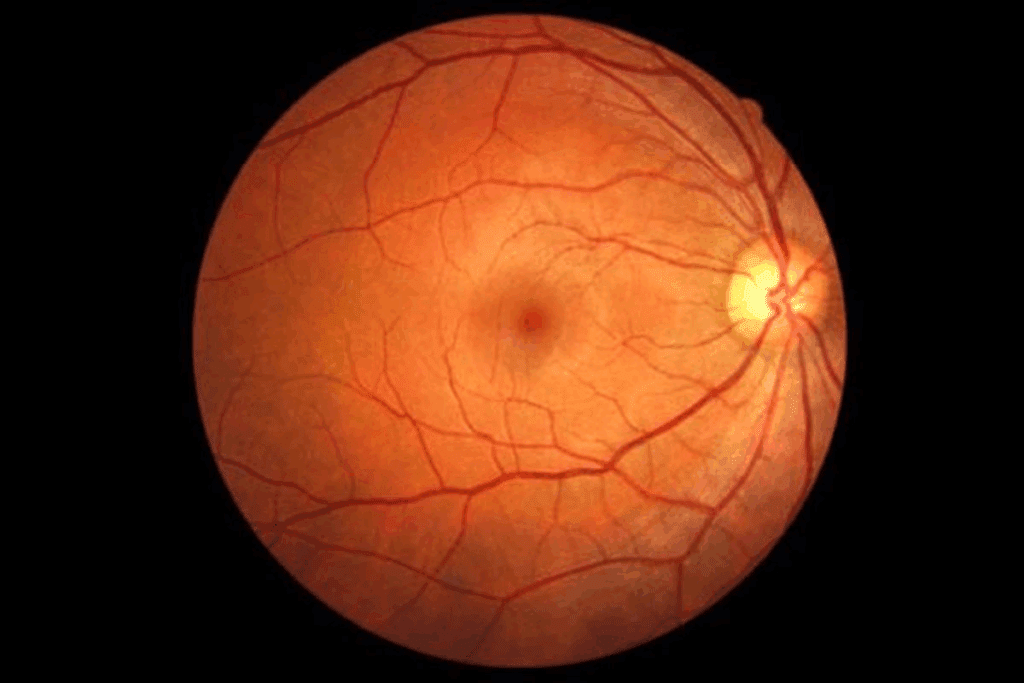
- fundus exams to see the retina and macula.>
During a fundus exam, doctors can see ERM, where it is, and any other eye changes. Fundus photography helps record these findings and track changes over time.
Advanced Imaging Technologies
New imaging tools have changed how we diagnose ERM. Optical Coherence Tomography (OCT) gives clear images of the retina. This lets doctors measure ERM thickness and location accurately.
OCT angiography also shows vascular changes in the retina linked to ERM.
Distinguishing ERM from Other Macular Conditions
It’s important to tell ERM apart from other eye problems. This includes macular holes, edema, and age-related macular degeneration. Doctors must use their skills and tools to make the right call.
Condition | Key Features | Diagnostic Tools |
ERM | Membrane formation on the retinal surface, retinal distortion | OCT, Fundus examination |
Macular Hole | Full-thickness defect in the macula | OCT, Fundus examination |
Macular Edema | Fluid accumulation in the macula, retinal thickening | OCT, Fluorescein Angiography |
Age-related Macular Degeneration | Drusen, RPE changes, choroidal neovascularization | OCT, Fundus examination, Fluorescein Angiography |
By using both old and new methods, doctors can accurately diagnose ERM. This ensures the right treatment for each patient.
Treatment Options for Epiretinal Membrane
Managing Epiretinal Membrane (ERM) requires a variety of approaches. This includes watching the condition or going under the knife. We’ll look at the best ways to treat ERM, aiming to improve symptoms and life quality.
Observation and Monitoring Protocols
For those with mild symptoms, watching and checking up is often advised. Regular eye exams are key to track the condition’s progress. We use advanced tools like optical coherence tomography (OCT) to see how the membrane affects the retina.
Watching protocols might include:
- Regular OCT scans to monitor membrane thickness and retinal distortion
- Visual acuity tests to assess changes in vision
- Amsler grid testing to detect metamorphopsia (distorted vision)
Surgical Intervention: Vitrectomy and Membrane Peeling
For those with serious vision loss, surgery is often needed. The main surgery for ERM is pars plana vitrectomy (PPV) with membrane peeling. This involves removing the vitreous gel and the membrane to ease retina pressure.
Key aspects of vitrectomy and membrane peeling include:
Procedure | Description | Benefits |
Vitrectomy | Removal of the vitreous gel | Reduces traction on the retina |
Membrane Peeling | Removal of the epiretinal membrane | Improves retinal surface regularity |
Post-Surgical Care and Rehabilitation
After surgery, proper care is essential for the best results. We usually suggest:
- Using antibiotic and anti-inflammatory eye drops to prevent infection and inflammation
- Avoiding strenuous activities and heavy lifting for several weeks
- Attending follow-up appointments to monitor healing and vision recovery
Rehabilitation might include vision therapy to help with any vision issues.
Emerging Treatments and Research
New treatments for ERM are being researched, including medicines and advanced surgery. We’re looking into:
- Anti-vascular endothelial growth factor (anti-VEGF) injections to reduce membrane formation
- Minimally invasive surgical techniques to reduce recovery time
- Stem cell therapies to promote retinal health and regeneration
As research grows, we might see new treatments for ERM soon.
Living with Epiretinal Membrane
Living with epiretinal membrane means getting medical treatment, visual rehab, and making lifestyle changes. We know managing ERM needs a full plan to lessen its daily life impact.
Visual Rehabilitation Strategies
Visual rehab is key for ERM patients to adjust to changes. It includes ways to boost visual skills and daily living activities. Visual rehabilitation programs are made for each person. They might teach better eye movement, visual processing, and handling visual distortions.
Adapting to metamorphopsia, where straight lines look bent, is a big part of rehab. Patients learn to work around this, making daily tasks easier.
Adaptive Technologies and Low Vision Aids
Adaptive tech and low vision aids greatly improve life for ERM patients. Items like magnifying glasses, telescopic lenses, and electronic devices boost vision. Low vision aids make reading, watching TV, and other daily tasks easier.
Also, new tech like e-readers and smartphone apps helps those with vision issues.
Lifestyle Modifications and Preventive Measures
Changing your lifestyle can help manage ERM and stop it from getting worse. Regular eye checks are key to watch the condition and catch any changes early. Maintaining a healthy lifestyle, like eating well and staying active, is also important.
- Eating foods rich in omega-3 fatty acids, lutein, and zeaxanthin
- Exercising regularly to maintain overall health
- Avoiding smoking and limiting alcohol consumption
When to Seek Medical Attention
Knowing when to see a doctor is vital for ERM patients. Sudden vision changes, more distortion, or other symptoms that worry you need a doctor visit. Regular follow-ups with eye care experts are key for managing ERM well.
Being proactive and informed helps patients manage their condition and keep their quality of life good.
Conclusion
We’ve looked into Epiretinal Membrane (ERM), a condition that affects the retina and macula. It causes various vision problems. Knowing about ERM is key in eye care, as it greatly impacts people’s lives.
We talked about what ERM is, how common it is, why it happens, how to find out if you have it, and how to treat it. We also pointed out the difference between primary and secondary ERM. We discussed how certain things can increase your risk of getting it.
Handling ERM requires a full plan, including watching it, surgery, and care after surgery. New treatments and studies are showing hope for better results for patients.
As we wrap up our look at ERM in eye care, it’s vital for people with symptoms to get checked by a doctor. Early diagnosis and the right treatment can greatly improve life for those with ERM.
FAQ
What is an epiretinal membrane (ERM) in the context of ophthalmology?
An epiretinal membrane is a condition where a layer of fibrocellular tissue forms on the retina. It often causes visual disturbances and metamorphopsia.
What are the alternative names for epiretinal membrane?
Epiretinal membrane is also known as macular pucker or cellophane maculopathy.
How serious is epiretinal membrane and what are its implications?
The severity of epiretinal membrane varies. It can cause significant visual disturbances. This can impact daily activities and quality of life if left untreated.
What is the prevalence of epiretinal membrane in different age groups?
Epiretinal membrane is more common in older adults. Its prevalence increases with age.
What are the risk factors for developing epiretinal membrane?
Risk factors include age-related factors, ocular conditions like posterior vitreous detachment, and systemic health conditions.
What are the common symptoms of epiretinal membrane?
Common symptoms include visual disturbances, metamorphopsia, and blurred vision.
How is epiretinal membrane diagnosed?
Diagnosis involves clinical examination techniques and advanced imaging technologies like optical coherence tomography (OCT). It also includes distinguishing ERM from other macular conditions.
What are the treatment options for epiretinal membrane?
Treatment options include observation and monitoring protocols, surgical intervention like vitrectomy and membrane peeling, and post-surgical care and rehabilitation.
What are the emerging treatments and research in the field of epiretinal membrane?
Emerging treatments and research include new surgical techniques, pharmacological interventions, and other innovative approaches to manage ERM.
How can individuals live with epiretinal membrane and manage its impact?
Strategies for living with ERM include visual rehabilitation, adaptive technologies, lifestyle modifications, and preventive measures.
When should I seek medical attention for epiretinal membrane?
It is essential to seek medical attention if symptoms persist or worsen, or if you experience sudden changes in vision.
What is the role of posterior vitreous detachment in the development of epiretinal membrane?
Posterior vitreous detachment is a significant risk factor for developing ERM. It can cause the formation of fibrocellular tissue on the retina.
Can epiretinal membrane be caused by other ocular conditions or procedures?
Yes, secondary ERM can be caused by various ocular conditions, such as retinal detachment, or ocular surgeries.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5377420/