Have you seen straight lines look wavy or blurry? Or is your central vision getting fuzzy in one eye? You might have an epiretinal membrane (ERM). This is a common eye problem that affects millions globally.What is an epi membrane? This ultimate guide explains the epiretinal membrane (ERM) in ophthalmology and its treatment.
At Liv Hospital, we offer top-notch eye care with the latest tools. An ERM, or “macular pucker,” is a thin tissue layer on the retina. It can mess with your vision, mainly in older folks.
It’s key to know about ERM for both patients and doctors. While some cases just need watching, knowing the causes and treatments helps keep your eyes healthy.
Key Takeaways
- Epiretinal membrane (ERM) is a common age-related eye condition.
- ERM is also known as “macular pucker.”
- A thin layer of fibrocellular tissue forms on the retina’s surface.
- ERM can cause distorted vision and is common in older adults.
- Understanding ERM is key for managing and treating it well.
Definition and Overview of Epiretinal Membrane

Understanding epiretinal membrane (ERM) is key to treating vision problems. ERM is a common issue that affects the retina’s back part, over the macula. It creates a fibrocellular layer on the retina’s surface, causing various vision problems.
Medical Definition of ERM
ERM is a fibrocellular layer on the retina’s surface, mainly affecting the macula. It can pull on the retina, causing visual distortions and decreased visual acuity. It often happens with age but can also come from other eye issues or surgery.
ERM is a big reason for vision loss in many people. It can make the retina thicker, cause edema, and even lead to retinal detachment in bad cases. Knowing what ERM is helps doctors treat it well.
Anatomy of the Retina and Macula
The retina is a complex layer at the eye’s back, turning light into signals for the brain. The macula, at the retina’s center, is key for fine detail vision and face recognition. It’s the most sensitive part, handling central vision.
The retina and macula have many layers of cells working together for vision. The macula has lots of cone photoreceptors for detailed vision and color. Any problem, like ERM, can greatly affect how we see.
The Epi Membrane: Structure and Formation
To grasp the epi membrane retina, we must look at its cells and how it forms. Epiretinal membranes (ERMs) grow on the retina’s surface, impacting our sight.
Cellular Composition of Epiretinal Membranes
ERMs are made up of different cells. These include glial cells, retinal pigment epithelial cells, and myofibroblastic cells. These cells grow and gather on the retina, creating a membrane that can mess with our vision.
Cellular Components of ERM:
Cell Type | Role in ERM Formation |
Glial Cells | Provide structural support and contribute to membrane formation |
Retinal Pigment Epithelial Cells | Influence membrane characteristics and potentially contribute to its growth |
Myofibroblastic Cells | Play a key role in the contraction and thickening of the ERM |
How ERMs Develop on the Retinal Surface
ERMs grow on the retina for many reasons. They can appear without a clear cause (IERM) in about 95% of cases. Or they can come from trauma, surgery, or long-term eye diseases. Myofibroblastic cells growing at the vitreoretinal interface are key to ERM formation.
“The pathogenesis of ERM involves a complex interplay of cellular proliferation, membrane formation, and vitreoretinal interaction.” –
ERM Research Study
ERMs can really mess with our vision, causing things like distorted vision and blurry sight. Knowing how ERMs form and grow is key to treating them well.
Understanding ERMs helps us see how complex this condition is. It shows why we need a full approach to care.
Prevalence and Demographics
ERM affects a lot of people, with its numbers changing with age. It’s a big deal for eye health, mainly for older folks.
Age-Related Incidence Rates
As people get older, ERM becomes more common. At least 2 percent of those over 50 have it. By 75, that number jumps to 20 percent. This shows why eye exams are key as we age.
Understanding the age-related incidence of ERM is key for catching it early. Research shows ERM affects 7 to 11.8 percent of people. This makes it a big public health issue.
Bilateral Occurrence and Risk Factors
ERM can hit one or both eyes, which is a big worry for patients. Older people are more likely to get it. Other risks include past eye surgeries, retinal detachments, and certain eye problems.
While age is a big risk, other things can play a part in ERM. Keeping an eye on eye health and acting fast on any changes is important. This helps manage ERM well.
Knowing how common ERM is helps doctors plan better care. This can lead to better results for patients.
Types of Epiretinal Membranes
ERM can appear in different forms, mainly as idiopathic or secondary. Knowing the type helps doctors understand the cause and choose the right treatment.
Idiopathic Epiretinal Membrane (IERM)
Most ERM cases, about 95%, are idiopathic. Idiopathic ERM happens without a clear reason or related eye condition. Studies show it’s more common in older people, possibly linked to aging.
Idiopathic ERM is hard to deal with because we don’t know what causes it. But, new ways to diagnose and track these membranes have helped a lot.
Secondary Epiretinal Membranes
Secondary ERM is linked to eye and body conditions. For example, diabetic retinopathy, retinal detachment, and eye injuries can cause it. Knowing the cause is key to treating it well.
Secondary ERM needs a careful treatment plan. This plan considers the condition that caused it. For example, treating diabetic retinopathy is important for secondary ERM linked to it.
In short, knowing if ERM is idiopathic or secondary is critical for doctors. It helps them plan the best treatment and improve patient results.
Causes of Epiretinal Membrane
Epiretinal membrane forms due to many factors, like age and eye health. Knowing what causes it helps in finding better treatments.
Aging Process and ERM Development
Getting older increases the risk of getting an epiretinal membrane. The eye’s vitreous gel changes with age, which can cause ERM. Research shows ERM is more common after 50.
Table: Age-Related Incidence of ERM
Age Group | Incidence of ERM |
40-49 years | 2.3% |
50-59 years | 5.6% |
60-69 years | 12.1% |
70+ years | 18.5% |
Ocular Conditions Leading to ERM
Eye problems like diabetic retinopathy and retinal vein occlusion can lead to ERM. Knowing these conditions helps spot who’s at risk.
Systemic Conditions Associated with ERM
Diabetes and high blood pressure can also increase ERM risk. Keeping these conditions in check might lower ERM risk.
It’s important to remember that while these conditions are linked to ERM, the exact reasons for ERM are being studied.
Symptoms and Clinical Presentation
ERM can cause many visual symptoms that make daily tasks hard. These symptoms can really change how well someone lives, so it’s key to know what they are and how they show up.
Visual Disturbances in ERM
People with ERM face many visual problems. They might see things blurred, have monocular diplopia (double vision in one eye), or see things as smaller than they are. These issues can make simple tasks like reading, driving, and seeing faces hard.
How bad these problems are can differ from person to person. It depends on how big the ERM is and where it is. Some people might not even notice it, while others find it very hard to deal with.
Metamorphopsia and Its Impact on Daily Life
Metamorphopsia is a big sign of ERM. It makes straight lines look wavy. This can really mess up tasks that need clear vision, like reading or using computers. Metamorphopsia can make daily life tough.
Dealing with ERM and its visual problems can be tough. But knowing the symptoms and how they affect life can help. People can then get the right medical help and find ways to live better with ERM.
Diagnosis of Epiretinal Membrane
To diagnose Epiretinal Membrane, doctors use many methods. They start with simple checks and then use advanced imaging. This mix helps them understand the condition well, making treatment easier.
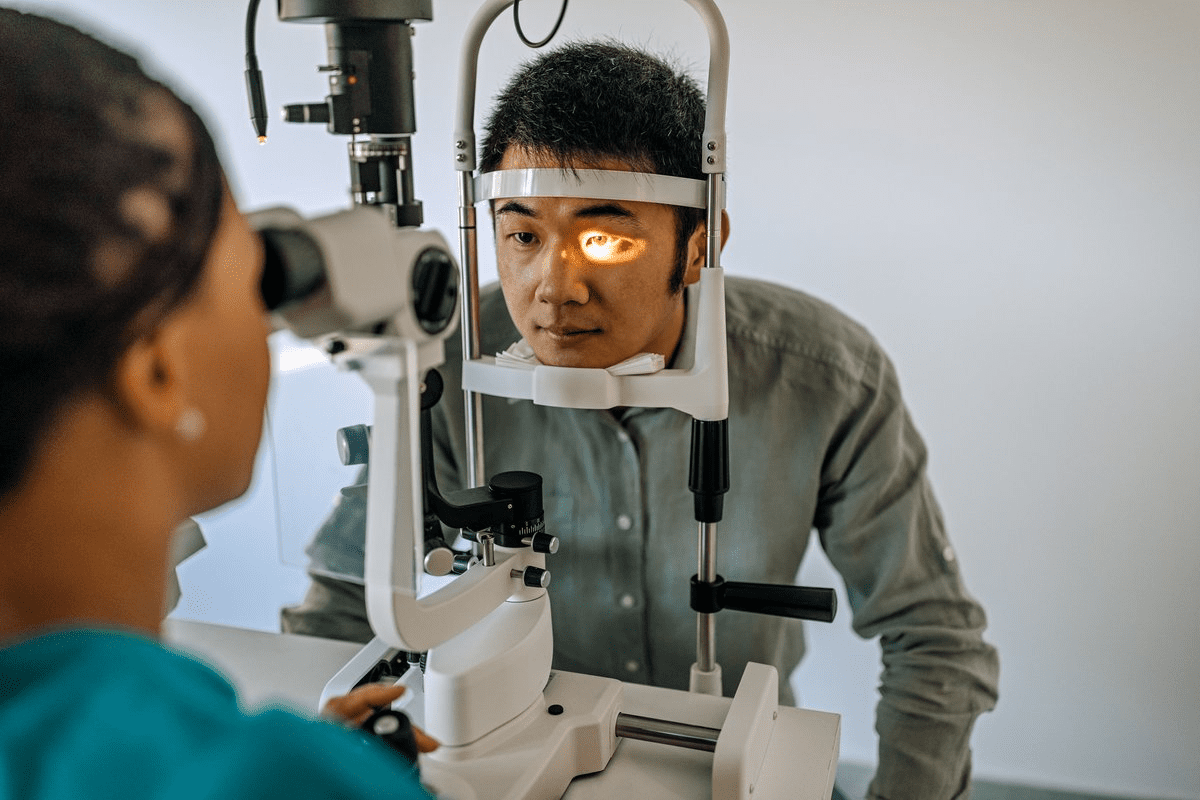
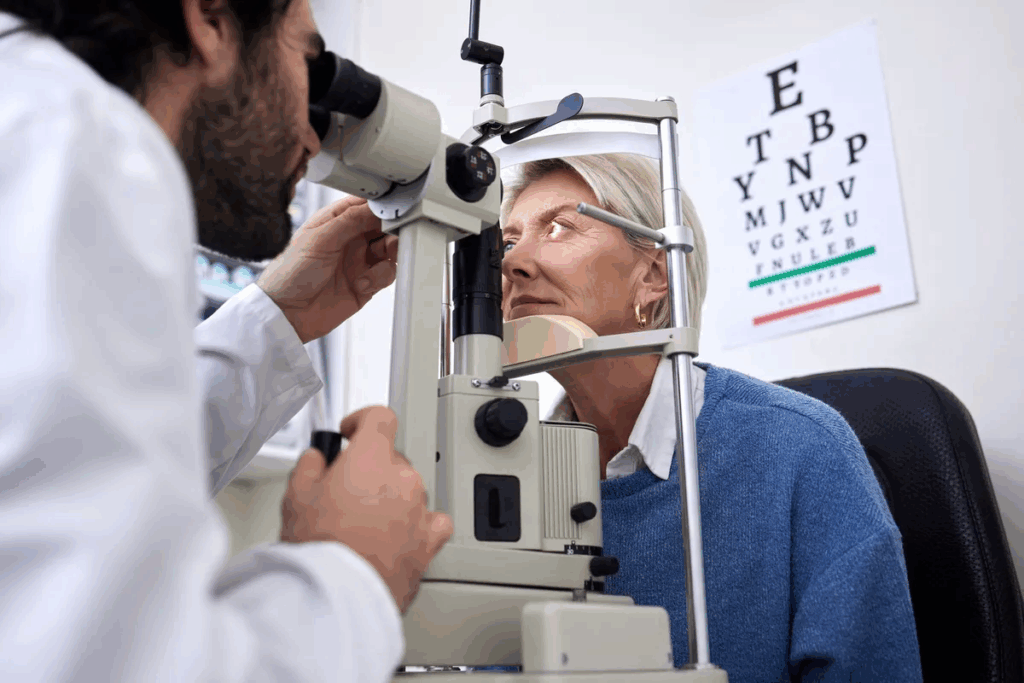
Clinical Examination Techniques
Doctors first check for ERM with a slit-lamp and fundus exam. These tools help spot signs like thickened retina or distortion.
Slit-lamp examination looks at the front parts of the eye. Fundus examination focuses on the retina and macula. Both are key for finding ERM and seeing its effects.
Imaging Technologies for ERM Detection
Imaging is key in finding ERM. Optical Coherence Tomography (OCT) gives clear images of the retina and ERM. OCT shows how thick the retina is and if ERM is present.
Other tools like fundus fluorescein angiography help check for vascular changes in ERM.
Differential Diagnosis Considerations
When diagnosing ERM, doctors must think of other conditions that look similar. They look out for macular edema, vitreomacular traction syndrome, and retinal detachment.
Condition | Key Features | Differential Diagnosis Clues |
ERM | Retinal thickening, distortion | OCT shows ERM, retinal thickening |
Macular Edema | Retinal thickening, fluid accumulation | OCT shows fluid accumulation, not ERM |
Vitreomacular Traction Syndrome | Vitreous traction on macula | OCT shows vitreous traction, not ERM |
Getting the diagnosis right is key for treating ERM well. Doctors use both old and new methods to care for patients with ERM.
Treatment Options for Epiretinal Membrane
Treating Epiretinal Membrane (ERM) requires a mix of non-surgical and surgical methods. Each patient’s case is different, so we tailor the treatment to fit their needs.
Conservative Management Approaches
For many, the first step is conservative management. This means watching the condition closely to see how it changes. If symptoms are mild, we might suggest waiting and seeing how things go.
Wearing glasses or contact lenses can also help improve vision. Sometimes, we recommend low vision aids to make daily tasks easier.
Surgical Interventions: Vitrectomy and Membrane Peeling
If conservative methods don’t work, surgery might be needed. The main surgery for ERM is pars plana vitrectomy with membrane peeling. This involves removing the vitreous gel and the membrane to reduce retina traction.
This surgery is done under local anesthesia. The goal is to improve or stabilize vision. We decide on surgery based on how bad the symptoms are and the patient’s health.
We talk to our patients about the surgery’s benefits and risks. This helps them make an informed choice.
Post-Operative Care and Recovery
After surgery, proper care is key for a good outcome. We give detailed instructions on how to care for your eyes post-surgery. This includes using eye drops, avoiding heavy lifting, and attending follow-up appointments.
Most people can go back to normal activities in a few weeks. But, it can take several months to fully recover. Following our instructions carefully helps avoid complications and ensures the best vision.
We’re here to support our patients during recovery. We answer any questions or concerns they may have.
Living with ERM: Coping Strategies and Adaptations
Coping with ERM requires a mix of visual aids and lifestyle changes. People with ERM often need to adjust their daily routines to handle visual issues.
Visual Aids and Assistive Technologies
Visual aids and assistive technologies are key for ERM patients. They include:
- Magnifying glasses and lenses to enhance visual clarity
- Specialized lighting to reduce glare and improve visibility
- Electronic devices with text-to-speech functionality
- Smart glasses with augmented reality features
These tools greatly enhance life for those with ERM. For example, magnifying glasses aid in reading and other tasks needing clear vision.
Lifestyle Modifications and Support Resources
Along with visual aids, lifestyle changes help ERM patients. Recommended adjustments include:
- Eating a diet full of nutrients good for eye health
- Staying active to boost overall health
- Wearing sunglasses to block UV rays
- Getting support from family, friends, and groups
Support groups and counseling are also essential for ERM patients. They offer emotional support and useful tips from others facing similar issues.
By using visual aids, making lifestyle changes, and getting support, ERM patients can manage their condition well. This helps them keep a good quality of life.
Future Directions in ERM Management
New research and innovation are changing how we manage ERM. This brings hope to patients. We’re learning more about Epiretinal Membrane and finding new ways to treat it.
Emerging Treatments and Clinical Trials
ERM treatment is getting better fast. New treatments are being tested in clinical trials. For example, anti-vascular endothelial growth factor (anti-VEGF) agents might help lessen ERM symptoms.
“The future of ERM treatment is exciting,” says Medical Expert. “We’re on the edge of a new era with better, less invasive treatments for patients.”
Advances in Surgical Techniques
Surgery for ERM is getting better too. Intraoperative Optical Coherence Tomography (OCT) helps surgeons see better during surgery. This makes ERM surgery safer and more effective.
New tools and better techniques are also helping. Using dyed dyes makes the ERM easier to see and remove. This improves surgery results.
The future of ERM management looks bright. It will be shaped by new treatments, clinical trials, and better surgery. We’re dedicated to improving patient care and quality of life for those with ERM.
Conclusion
Knowing about epiretinal membrane (ERM) is key for both patients and eye doctors. ERM affects the retina’s surface and can harm vision and daily life. We’ve looked into what ERM is, how common it is, its symptoms, how it’s diagnosed, and how it’s treated.
ERM is a big deal in eye care and needs careful handling. Doctors use special tests and tools to spot ERM and figure out the best treatment. Treatments can be simple or involve surgery, like removing the membrane.
As eye care gets better, knowing about ERM is more important than ever. Keeping up with new ways to diagnose and treat ERM helps doctors give the best care. Good management of ERM can really help patients see better and live better lives.
FAQ
What is epiretinal membrane (ERM) in ophthalmology?
Epiretinal membrane, or macular pucker, is a thin layer of tissue on the retina. It can affect vision.
How serious is epiretinal membrane?
ERM’s impact can vary. It can cause big vision problems, but how it affects daily life depends on the person.
What are the causes of epiretinal membrane?
ERM can come from aging, eye conditions, or diseases. Aging is a big risk factor.
What are the symptoms of ERM?
Symptoms include vision problems and metamorphopsia. These can change daily life.
How is ERM diagnosed?
Doctors use exams and imaging like OCT to diagnose ERM. This helps them understand the condition well.
What are the treatment options for ERM?
Treatments range from watching it to surgery. The choice depends on how bad it is.
How can patients cope with ERM?
Patients can use aids, make lifestyle changes, and get support. This helps manage the condition.
Are there any emerging treatments for ERM?
Yes, new treatments and surgery methods are being tested. They might help patients in the future.
Can ERM occur in both eyes?
Yes, ERM can happen in both eyes. Age and other factors can increase this risk.
What is the role of OCT in diagnosing ERM?
OCT is key in diagnosing and managing ERM. It shows detailed retina images. This helps doctors decide on treatment.
References
National Health Service (NHS). Evidence-Based Medical Guidance. Retrieved from https://www.nhs.uk/conditions/macular-pucker/