A macular pucker, also known as an epiretinal membrane (ERM), is a condition. It happens when a thin layer of scar tissue forms on the macula. The macula is the part of the retina that helps us see things clearly.What is a retinal wrinkle? This ultimate guide explains macular pucker (epiretinal membrane) and how it affects vision.
This condition can make straight lines look wavy or bent. Reading can become hard because letters or words might seem crowded or missing.
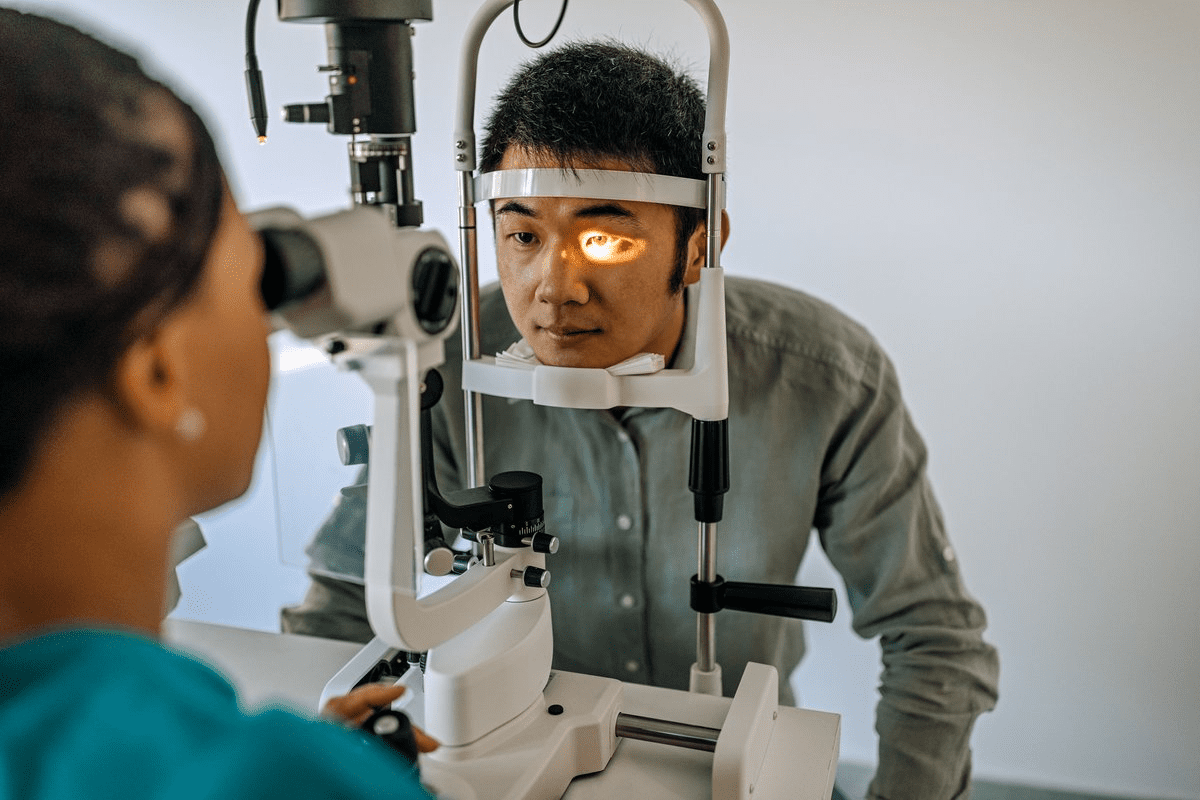
At Liv Hospital, our expert retinal specialists use advanced technology. They detect and manage macular puckers early. This helps keep your vision and quality of life good.
Key Takeaways
- A macular pucker is a thin layer of scar tissue on the macula.
- It can cause distorted vision and affect daily activities.
- Liv Hospital’s specialists use advanced technology for early detection.
- Early management can help preserve vision and quality of life.
- Macular pucker is also known as an epiretinal membrane (ERM).
Understanding Macular Pucker: Definition and Overview

A macular pucker, also known as an epiretinal membrane, forms on the macula. It causes visual distortions and discomfort. This condition is due to scar tissue on the macula, which is key for sharp vision.
The Structure of the Eye and the Macula’s Role
The human eye is complex, with the retina being a key part. The retina has cells that turn light into signals for the brain, helping us see. The macula, at the retina’s center, is vital for detailed vision, like reading and driving.
The macula has many photoreceptor cells. This makes it essential for tasks needing precision and clarity. Damage to this area can greatly affect one’s life.
What Happens When a Macular Pucker Forms
A macular pucker forms a scar tissue layer on the macula. This causes the macula to wrinkle, leading to distorted vision. Symptoms include blurred vision, double vision, or seeing lines as wavy.
Many factors can cause a macular pucker, like aging, retinal tears, or eye inflammation. Knowing these causes helps in managing and treating the condition.
Condition | Description | Impact on Vision |
Macular Pucker | Formation of scar tissue on the macula | Distorted vision, blurred vision |
Epiretinal Membrane | Layer of fibrous tissue on the retina’s surface | Visual distortions, metamorphopsia |
Retina Pucker | Scar tissue causing retinal wrinkling | Blurred vision, double vision |
Understanding the eye’s structure and the macula’s role helps us grasp the impact of macular pucker. It’s important to seek medical help if symptoms appear.
The Retinal Wrinkle: How Macular Pucker Develops

A macular pucker forms through a complex process that affects the retina. Scar tissue on the macula causes a wrinkling or puckering effect.
To grasp this, we must explore how scar tissue forms and its impact on the retina.
Formation of Scar Tissue on the Macula
Scar tissue on the macula is key in macular pucker development. Glial cells move through a defect in the retinal surface, forming a membrane. This membrane then contracts, causing the macula to wrinkle.
This process is like a membrane tightening over time, distorting the retinal tissue underneath.
The Process of Retinal Puckering
Retinal puckering happens when scar tissue on the macula contracts. This contraction wrinkles the retina, causing visual distortions.
The progression of retinal puckering varies. Some people see big changes, while others notice little.
Stage | Description | Visual Impact |
Early Stage | Initial formation of scar tissue | Mild visual distortions |
Advanced Stage | Contraction of scar tissue, significant puckering | Noticeable vision problems, including blurred vision and metamorphopsia |
Knowing the stages of retinal puckering helps in diagnosing and managing macular pucker.
Prevalence and Demographics: Who Gets Macular Pucker
As the world’s population gets older, macular pucker is becoming more common. It affects about 9% of people, with more cases as age increases. Knowing who is most at risk helps in catching and treating it early.
Age-Related Prevalence Statistics
Research shows that macular pucker strikes about 2% of those in their 50s. By the 75s, this number jumps to 20%. This rise with age stresses the need for regular eye checks as we get older.
Age Group | Prevalence of Macular Pucker |
50-59 years | 2% |
60-69 years | 5% |
70-79 years | 12% |
80 years and above | 20% |
Risk Factors for Developing Macular Pucker
Several factors can lead to macular pucker. These include:
- Age: The risk grows with age.
- Posterior Vitreous Detachment (PVD): PVD happens when the vitreous gel pulls away from the retina.
- Diabetes: People with diabetes face a higher risk.
- Eye Inflammation or Trauma: Eye issues or injuries can also raise the risk.
Knowing these risk factors helps spot who’s more likely to get it. They can then get eye exams more often.
Primary Causes of Macular Pucker
Knowing the main reasons for macular pucker is key for prevention and treatment. This condition causes scar tissue on the macula, leading to blurry vision. The main reason is posterior vitreous detachment (PVD), a condition that happens as we age.
Posterior Vitreous Detachment (PVD)
Posterior vitreous detachment is behind 95% of macular pucker cases. As we get older, the vitreous gel shrinks and separates from the retina. This can lead to the formation of epiretinal membranes and macular pucker. It’s important to watch for PVD as it can cause more serious eye problems.
Secondary Causes of Epiretinal Membranes
While PVD is the main cause, other factors can also lead to epiretinal membranes and macular pucker. These include retinal tears, eye trauma, and diabetic retinopathy. Knowing these secondary causes helps us spot who’s at higher risk and prevent the condition.
Cause | Description | Risk Factor |
Posterior Vitreous Detachment (PVD) | Age-related condition where vitreous gel separates from the retina | High |
Retinal Tears | Tears in the retina can lead to epiretinal membrane formation | Moderate |
Eye Trauma | Physical injury to the eye can cause epiretinal membranes | Moderate |
Diabetic Retinopathy | Diabetes-related damage to the retina can lead to macular pucker | High |
By understanding both the main and secondary causes of macular pucker, we can improve diagnosis and treatment. This can lead to better outcomes for those affected.
Symptoms and Visual Changes
Knowing the symptoms of macular pucker is key for early detection and treatment. We’ll look at the visual changes it causes. It’s important to spot the early signs and how they affect daily life.
Early Warning Signs
The first signs of macular pucker can be small but important. You might see distorted vision and blurred central vision. Straight lines might look wavy, and objects could seem off.
These signs can be clear when you read or try to see faces. Other signs include double vision in one eye and gray or cloudy spots in your central vision. These changes can come and go, so watch your vision closely.
How Vision is Affected
As macular pucker gets worse, vision problems get more serious. Reading and driving can become hard because of the distorted vision. It can also make it tough to recognize faces, affecting social life.
Visual changes from macular pucker can differ for everyone. But they often greatly affect daily life. If you notice these symptoms, see a doctor right away.
Progression of Symptoms Over Time
Macular pucker symptoms can get worse slowly over years. For some, vision decline is gradual. Others might see little change or no worsening.
It’s important to keep an eye on how symptoms change. Regular eye exams help track vision changes. This ensures the right treatment is used.
Diagnosing Macular Pucker
To find out if someone has macular pucker, doctors use special tools. It’s key to get the right treatment and help the patient get better.
Comprehensive Eye Examination Procedures
First, a detailed eye check is done. This includes looking at the patient’s health history and how well they can see. A special eye exam lets doctors see the retina and macula closely.
They look for signs of macular pucker, like thickening or distortion in the retina.
Optical Coherence Tomography (OCT) Imaging
Optical Coherence Tomography (OCT) imaging is a tool that shows the retina’s details without hurting it. It’s great for spotting macular pucker because it shows the layers of the retina clearly.
Fluorescein Angiography and Other Diagnostic Tools
Fluorescein angiography is another way to check for macular pucker. It uses dye to light up the blood vessels in the retina. This helps doctors see any problems with blood flow.
Other tools, like fundus photography, help track how the condition changes over time.
By using all these tools together, doctors can find out if someone has macular pucker. Then, they can plan the best treatment for each patient.
Treatment Options for Macular Pucker
Choosing a treatment for macular pucker depends on how much it affects your vision and daily life. Options range from watching it closely to more serious surgery. This choice depends on how bad the symptoms are and how much they affect your life.
Monitoring and Non-Surgical Approaches
If macular pucker doesn’t hurt your vision much, doctors might just watch it. They’ll check your eyes often and use Optical Coherence Tomography (OCT) imaging to see if it changes. For some, this is enough, as long as the symptoms aren’t too bad.
Other non-surgical ways include using visual aids or changing your daily habits. These help manage symptoms but don’t fix the problem itself.
Vitrectomy Surgery: Procedure and Recovery
If macular pucker really hurts your vision, vitrectomy surgery might be needed. This surgery removes the vitreous gel and scar tissue causing the problem. It aims to reduce pressure on the retina and improve your sight.
The surgery is done under local anesthesia. After, you’ll need to rest and follow care instructions to heal right. Most people can get back to normal in a few weeks. But it might take longer for your vision to fully get better.
Risks and Benefits of Surgical Intervention
Vitrectomy surgery can help a lot, but it’s not without risks. Benefits include better vision and less symptoms. But, there are risks like infection, retinal detachment, or cataracts.
Talking to your eye doctor about these risks and benefits is key. They’ll help you decide if surgery is right for you. The decision depends on how bad your symptoms are, how they affect your life, and your eye health.
In short, treating macular pucker is all about what’s best for you. It might be watching it, trying non-surgical methods, or surgery. The goal is to keep or improve your vision and quality of life.
When to See an Eye Doctor
Knowing when to visit an eye doctor is key to keeping your vision sharp. Macular pucker can seriously affect your sight. Getting medical help quickly is very important.
Warning Signs That Require Immediate Attention
If you notice any of these symptoms, see an eye doctor right away:
- Distorted vision: Straight lines look wavy or distorted.
- Blurred vision: Trouble reading or doing daily tasks because of blurry vision.
- Double vision: Seeing two images instead of one, a sign of advanced macular pucker.
- Blind spots: Blind spots or missing areas in your vision.
These signs might mean you have macular pucker or another serious eye problem. Getting checked and treated quickly can save your vision.
Regular Eye Exams and Macular Pucker Detection
Regular eye exams are vital for catching macular pucker early. Your eye doctor can:
- Check your vision and look for any changes.
- Do a detailed eye exam with your pupils dilated to see the retina and macula.
- Use tools like Optical Coherence Tomography (OCT) to see the retina clearly.
Seeing an eye doctor regularly can help find problems early. This can lead to better treatment results. If you’re at risk for macular pucker, make sure to get regular check-ups.
Living with Macular Pucker: Coping Strategies
Macular pucker can be tough, but there are ways to make life better. You need to treat it medically, change your lifestyle, and get emotional support.
Visual Aids and Assistive Technologies
Visual aids and tech are key for those with macular pucker. Magnifying glasses, big print, and text-to-speech software make daily life easier.
Magnifying glasses help with reading and tasks. Digital devices can be set to high contrast to ease eye strain.
Lifestyle Adjustments for Better Vision
Changing your lifestyle can help with macular pucker. Make your home brighter and reduce glare.
- Use brighter, focused lighting to cut down eye strain.
- Anti-glare screens on digital devices are also helpful.
- Eating foods good for your eyes is important.
Emotional Impact and Support Resources
Macular pucker affects your emotions too. It’s key to face these challenges and find support.
Support groups, online or in-person, offer community and understanding. Professional counseling helps with emotional issues.
With medical care and these strategies, you can live a better life with macular pucker.
Conclusion: Protecting Your Eye Health
Keeping your eyes healthy is key to avoiding vision issues, like macular pucker. Regular eye exams help catch problems early. Knowing the signs and risks of macular pucker helps you protect your vision.
Good eye health comes from regular check-ups and healthy habits. It also means watching for early signs of eye trouble. Simple steps, like shielding your eyes from UV rays and managing health issues, help a lot.
We urge you to make eye health a priority. Schedule eye exams regularly and learn about preventing macular pucker. This way, you can lower the chance of vision problems and keep your eyes in top shape.
FAQ
What is macular pucker?
Macular pucker is a condition where a thin layer of scar tissue forms on the macula. This causes distorted vision. It’s also known as epiretinal membrane or macular membrane pucker.
What are the symptoms of macular pucker?
Symptoms include distorted vision and blurred vision. It can also make reading or daily activities hard. Some people see straight lines as wavy or experience double vision.
How is macular pucker diagnosed?
Doctors use a thorough eye exam to diagnose it. They use Optical Coherence Tomography (OCT) imaging and fluorescein angiography. These tools help them see the condition and its severity.
What causes macular pucker?
The main cause is posterior vitreous detachment (PVD). This is when the vitreous gel separates from the retina. Other causes include retinal tears, eye trauma, and diabetic retinopathy.
Who is at risk of developing macular pucker?
Older adults are more likely to get it. The risk goes up with age. People with a history of eye problems are also at higher risk.
Can macular pucker be treated?
Yes, it can be treated. Doctors might use non-surgical methods or surgery. The choice depends on how severe it is and the person’s eye health.
What is vitrectomy surgery for macular pucker?
It’s a surgery to remove the vitreous gel and scar tissue. It’s done under local anesthesia. Recovery time varies by person.
Can macular pucker be prevented?
There’s no sure way to prevent it. But regular eye exams can catch it early. Early treatment can help avoid vision loss.
How can I cope with macular pucker?
Use visual aids and assistive technologies. Make lifestyle changes to improve vision. Seek support from family, friends, or groups.
What are the benefits of regular eye exams in detecting macular pucker?
Regular exams can catch it early. This allows for quick treatment and less chance of vision loss. They also find other eye problems like cataracts or glaucoma.
Is macular pucker related to other eye conditions?
Yes, it’s linked to conditions like retinal detachment, diabetic retinopathy, and age-related macular degeneration. Having these conditions raises the risk of macular pucker.
Can a flat macula be a sign of a resolved macular pucker?
A flat macula might mean the pucker was treated. But, it’s key to follow up with an eye doctor. They can confirm the diagnosis and check for other issues.
What is the difference between macular pucker and macular fold?
Macular pucker and macular fold are similar but different. Pucker is scar tissue on the macula. Fold is a more severe retina distortion.
Can eye trauma cause macular pucker?
Yes, eye trauma can lead to macular pucker. It causes scar tissue on the macula, leading to vision distortion.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/18709382/