Epiretinal membrane (ERM) is a condition where a layer of cells forms on the retina. It’s also known as cellophane maculopathy. Studies show that about 30 million people in the United States have ERM in at least one eye.What is a macular epiretinal membrane? This ultimate guide explains what ERM is, how serious it is, and treatment.
ERM can change how well you see and affect your daily life. Some people don’t notice any problems and just need to keep an eye on it. But others might see their vision get worse and need treatment. At Liv Hospital, we use the latest imaging and our team’s expertise to handle ERM well.
Understanding ERM is key to managing and treating it properly.
Key Takeaways
- ERM affects about 30 million people in the United States.
- It can cause big problems with vision if not treated.
- Liv Hospital offers top-notch imaging and care for ERM.
- Many ERM cases don’t show symptoms and just need watching.
- Finding ERM early is important for good treatment.
Understanding Macular Epiretinal Membrane: Definition and Overview
ERM, or epiretinal membrane, is a layer that forms on the retina’s surface. It affects vision. This condition happens when fibrocellular tissue grows on the retina, mainly on the macula. The macula is key for central vision and fine details.
“The formation of an epiretinal membrane can lead to significant visual disturbances, including distorted vision and decreased visual acuity,” as noted by retinal specialists. We will explore ERM in detail, explaining the terms and how it changes the eye.
What Happens in the Eye with ERM?
With ERM, a fibrocellular layer grows on the retina’s surface. This layer can cause the retina to wrinkle or distort, leading to vision problems. The macula, important for sharp vision, is hit hard by ERM.
Terminology: Macular Pucker and Cellophane Maculopathy
ERM is also known as macular pucker or cellophane maculopathy. “Macular pucker” means the retina wrinkles. “Cellophane maculopathy” describes the ERM’s clear, membrane-like look.
These terms show how ERM affects the retina and vision. Knowing them is key for diagnosis and treatment.
Basic Eye Anatomy and ERM Formation
The retina is at the back of the eye, turning light into signals for the brain. The macula, part of the retina, is vital for central vision. ERM forms on this surface, causing the retina to distort. This distortion messes with light processing, leading to vision problems.
ERM forms due to various reasons like aging, retinal tears, or surgery issues. Knowing the eye’s anatomy and how ERM forms helps understand its effects.
Prevalence and Epidemiology of ERM

The study of ERM shows us how it affects people. It’s clear that getting older plays a big part in its development.
Age-Related Incidence Rates
Research shows ERM gets more common with age. It’s rare in people under 50 but becomes more common after that. About 7% to 11.8% of people have ERM, and this number goes up to 17% for those over 80.
As more people live longer, knowing about ERM’s age-related increase is key for doctors and planners.
Key Findings from the Blue Mountains Study
The Blue Mountains Eye Study gave us important info on ERM.
“The Blue Mountains Study revealed a 5.3% incidence rate of ERM over a 5-year period, with 9.3% progression from early to advanced stages.”
Statistical Data in the United States
In the U.S., ERM’s prevalence follows global patterns, with age being a big factor. Here’s a table with data on ERM in different age groups:
Age Group | Prevalence of ERM |
50-59 years | 4.5% |
60-69 years | 8.2% |
70-79 years | 12.1% |
80+ years | 17% |
These numbers show ERM’s impact grows with age. This highlights the need for focused healthcare plans.
Types of Epiretinal Membranes
It’s important to know the different types of epiretinal membranes to choose the right treatment. These membranes are classified based on their cause and characteristics. This helps doctors diagnose and treat them well.
Idiopathic ERM (Primary)
Most cases, about 95%, are idiopathic ERM, or primary ERM. This type happens without a known cause or related eye disease. Researchers think age-related changes in the vitreous gel might cause it.
“The high number of idiopathic ERM cases shows how complex eye health is,” say eye specialists. “We need more research to understand and manage it better.”
Secondary ERM
Secondary ERM is caused by other eye diseases or conditions. This includes retinal detachment, diabetic retinopathy, or problems after surgery. It often means the eye has more serious issues and might need a different treatment plan.
Secondary ERM often comes from other eye problems. So, treating these issues early can help prevent ERM from forming.
Classification Based on Severity
ERM severity is measured using imaging like Optical Coherence Tomography (OCT). Knowing the severity helps doctors see how the disease is progressing and if treatment is needed.
- Mild ERM: Minimal symptoms, often not requiring immediate treatment.
- Moderate ERM: Noticeable symptoms, may require monitoring or treatment.
- Severe ERM: Significant visual disturbances, often necessitating surgical intervention.
Differences Between Early and Advanced Stages
In the early stages, ERM might not cause symptoms or only slight ones. But, as it gets worse, vision problems get more serious. These include distorted vision and seeing objects as smaller than they are.
Early detection and monitoring are key to managing ERM well and avoiding big vision loss. When it’s more advanced, treatment might need to be stronger, like surgery.
“Moving from early to advanced ERM stages can really affect a person’s life,” say eye doctors. “That’s why getting medical help early is so important.”
Common Causes of Epiretinal Membrane
Epiretinal membrane formation is often linked to several key factors. We will explore these in detail. Knowing these causes is key to diagnosing and treating this condition effectively.
Posterior Vitreous Detachment
Posterior vitreous detachment (PVD) is a major cause of epiretinal membrane, mainly in idiopathic cases. PVD happens when the vitreous gel in the eye separates from the retina. This separation can damage the retina, leading to ERM. Studies show PVD is behind about 95% of idiopathic ERM cases.
Post-Surgical Development
ERM can also occur after eye surgery, like cataract surgery. The exact reasons are not fully known. But, it’s thought that surgery trauma or changes in the vitreous gel post-surgery might cause ERM. So, patients who have had cataract surgery should watch for signs of ERM.
Retinal Vascular Diseases
Retinal vascular diseases, such as diabetic retinopathy, raise the risk of ERM. These diseases change the retina’s blood vessels, leading to fibrovascular membranes, a type of ERM. It’s important to manage these vascular diseases to prevent ERM.
Inflammatory Eye Conditions and Uveitis
Inflammatory eye conditions, including uveitis, can also lead to ERM. Eye inflammation can cause cells to grow on the retinal surface, forming membranes. Treating the underlying inflammation is key to managing ERM.
The following table summarizes the common causes of ERM and their characteristics:
Cause | Description | Risk Factors |
Posterior Vitreous Detachment | Separation of vitreous gel from the retina | Age, myopia |
Post-Surgical Development | ERM formation after eye surgery | Cataract surgery, other retinal surgeries |
Retinal Vascular Diseases | Diseases affecting retinal blood vessels | Diabetes, hypertension |
Inflammatory Eye Conditions | Uveitis and other inflammatory conditions | Autoimmune disorders, infections |
Understanding these causes helps in diagnosing and managing ERM. This can improve patient outcomes.
Signs and Symptoms of ERM
Knowing the signs and symptoms of ERM is key for early diagnosis and treatment. Epiretinal membrane (ERM) can show up in many ways, affecting people’s lives differently.
Asymptomatic Presentation
Many people with ERM don’t show symptoms. They might find out they have ERM during a routine eye check-up.
Visual Disturbances: Metamorphopsia and Micropsia
Symptoms can include metamorphopsia, where straight lines look wavy, and micropsia, where things seem smaller. These issues can really mess with daily tasks.
For example, reading or driving can become hard. Metamorphopsia makes everyday tasks tricky.
Progression of Symptoms Over Time
How ERM symptoms get worse can vary. Some people see a slow decline, while others stay the same for a while.
It’s important to watch how symptoms change. Regular eye exams help track vision and guide treatment.
Impact on Daily Activities
ERM symptoms can really affect daily life. They can make reading, driving, or tasks needing clear vision hard.
The table below shows common ERM symptoms and how they can affect daily life:
Symptom | Description | Impact on Daily Activities |
Metamorphopsia | Distortion of straight lines | Difficulty reading, driving |
Micropsia | Objects appear smaller | Challenges with tasks requiring precise vision |
Asymptomatic | No noticeable symptoms | No immediate impact, but regular monitoring is necessary |
In summary, knowing about ERM symptoms is critical for managing the condition. Recognizing visual disturbances and their effects on daily life helps patients and doctors create effective treatment plans.
How Serious Is Epiretinal Membrane?
It’s important for patients to know how serious Epiretinal Membrane (ERM) is. We’ll look at how ERM can affect vision and daily life. We’ll also compare it to other eye conditions.
Severity Spectrum of ERM
ERM can be mild or severe. Some people might not notice it much, while others might see big changes in their vision. Over time, symptoms can get worse.
The severity of ERM can vary a lot. It can range from no symptoms at all to serious vision problems. It’s key for patients to watch their condition closely.
Potential for Vision Loss
ERM usually doesn’t cause total blindness. But, it can make vision blurry or distorted. How much it affects vision varies from person to person.
Quality of Life Impact
ERM can really affect how you live your life. It can make everyday tasks hard, like reading or driving. It can also make you feel sad or less independent.
We know ERM can really change your life. It can stop you from doing things you love. This can make you feel frustrated and alone.
Comparing ERM to Other Retinal Conditions
ERM is different from other eye problems like macular degeneration. ERM can mess with your vision a lot, but it usually doesn’t cause total blindness. It can make everyday tasks hard, though.
- ERM is unique because it can cause big vision problems without making you blind.
- It affects your life in ways similar to other eye conditions.
- Getting surgery can really help people with ERM see better again.
Understanding ERM and comparing it to other eye problems helps patients and doctors. It helps them make better choices about treatment.
Diagnosing Epiretinal Membrane
To diagnose ERM, doctors use many methods. These range from basic eye exams to advanced imaging. Finding the right diagnosis is key to choosing the best treatment.
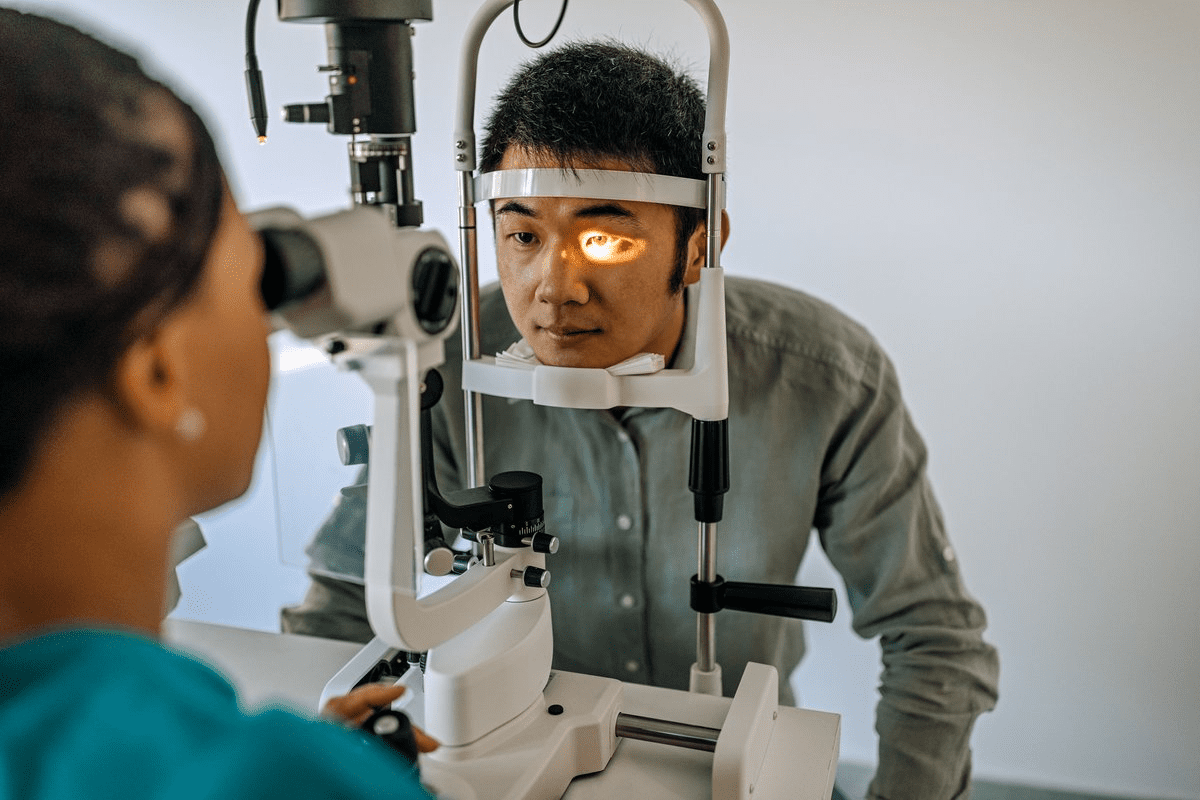
Comprehensive Eye Examination
A detailed eye exam is the first step. It includes checking the patient’s medical history and visual acuity. A dilated eye exam also looks for any retina issues.
During the dilated exam, eye drops widen the pupils. This lets doctors see the retina clearly. They look for signs of ERM, like thickening or distortion.
Optical Coherence Tomography (OCT)
OCT is a non-invasive test for ERM. It uses low-coherence interferometry to get detailed retina images. This helps doctors see any ERM-related issues.
OCT helps us understand how severe ERM is. It shows the membrane’s thickness and its effect on the retina. This info helps decide the best treatment.
Other Diagnostic Imaging Techniques
Other tests like fundus fluorescein angiography (FFA) and fundus photography are also used. They help spot vascular changes and other ERM signs.
Differential Diagnosis
It’s important to rule out other conditions when diagnosing ERM. Symptoms can be similar to other eye problems. We look at conditions like macular degeneration or retinal detachment to make sure we’re right.
The table below shows how we diagnose ERM:
Diagnostic Method | Description | Role in ERM Diagnosis |
Comprehensive Eye Examination | Includes medical history review, visual acuity testing, and dilated eye exam | Initial assessment and detection of retinal abnormalities |
Optical Coherence Tomography (OCT) | Non-invasive imaging test providing high-resolution retinal images | Critical for assessing ERM severity and retinal layer distortion |
Fundus Fluorescein Angiography (FFA) | Imaging technique that highlights retinal vascular changes | Helps identify vascular abnormalities associated with ERM |
Risk Factors for Developing ERM
Epiretinal Membrane (ERM) can develop due to age, eye conditions, and health issues. Knowing these factors helps in early detection and management.
Age-Related Factors
Age is a big risk for ERM, with most cases diagnosed at 65. As we get older, the eye’s vitreous gel changes, leading to ERM. Regular eye exams are key for older adults.
Previous Eye Conditions and Surgeries
Eye conditions and surgeries can raise ERM risk. For example, posterior vitreous detachment and retinal tears increase the chance. We’ll look at how these conditions affect ERM.
Eye Condition/Surgery | Relation to ERM |
Posterior Vitreous Detachment | Increased risk due to vitreous gel separation |
Retinal Tears | Higher risk of ERM formation |
Cataract Surgery | Potential for post-surgical ERM development |
Systemic Health Conditions
Some health conditions, like diabetes and hypertension, raise ERM risk. We’ll see how these conditions impact the eye and lead to ERM.
Genetic Predisposition
Genetics might also play a part in ERM. Research is ongoing to understand the genetic factors. This knowledge helps in spotting those at higher risk.
Understanding these risk factors helps us identify and manage ERM early. This approach is key to effective treatment.
Treatment Options for Epiretinal Membrane
There are different ways to treat ERM, from watching it closely to surgery. The right choice depends on how bad it is and the patient’s overall health. It also depends on how much it affects their vision and the risks of each treatment.
Observation and Monitoring Approach
For mild ERM, watching it closely might be the best plan. Regular eye checks help track any changes. Watching it closely is often chosen when surgery risks are too high. This is true when the ERM doesn’t really bother the patient’s daily life.
Vitrectomy Surgery Procedure
Vitrectomy surgery is key for serious ERM cases. It removes the vitreous gel and carefully peels the membrane off the retina. This surgery is done under local anesthesia, making recovery faster. It aims to fix vision problems and improve how well you can see.
Membrane Peeling Techniques
Peeling the membrane is a big part of ERM surgery. New tools and methods have made it safer and more effective. Using dyes like brilliant blue helps see the membrane better, making removal more precise.
Post-Surgical Recovery Timeline
After surgery, recovery takes time. It can take months for vision to fully come back. Care includes eye drops to prevent infection and follow-up visits. Patients should avoid hard work and heavy lifting early on.
Knowing about ERM treatments helps patients make better choices with their doctors.
Prognosis and Long-Term Outlook
Knowing the prognosis of Epiretinal Membrane is key for patients. It helps them understand what to expect for visual recovery and possible complications. The long-term outlook for ERM depends on several factors. These include the condition’s severity and how well treatment works.
Visual Recovery Expectations
Visual recovery after ERM treatment varies. Most patients see improvement in three to six months after surgery. The extent of recovery depends on the ERM’s severity and any other eye issues.
Visual Outcomes: Many studies show that a lot of patients see better after surgery. But, how much improvement varies.
Potential Complications
Like any surgery, ERM treatment has risks. These can include retinal detachment, infection, and cataract. Knowing these risks helps patients make better treatment choices.
Complication Rates: While complications are rare, it’s important for patients to know the risks. They should talk about these with their healthcare provider.
Recurrence Rates
ERM often doesn’t come back after treatment. But, in some cases, it can, needing more treatment.
Outcome | Frequency |
Visual Improvement | 70-80% |
Recurrence | 5-10% |
Complications | <5% |
Factors Affecting Outcomes
Several things can affect ERM’s prognosis and long-term outlook. These include the patient’s health, other eye conditions, and the ERM’s severity at diagnosis.
Understanding these factors and talking to a healthcare provider helps patients. They can then make better choices about their care.
Conclusion
Understanding Epiretinal Membrane (ERM) is key to managing this common retinal issue. It affects millions globally. ERM forms a membrane on the retina’s surface, causing symptoms and vision problems.
We’ve looked at ERM’s causes, symptoms, diagnosis, and treatments. It can come from posterior vitreous detachment, surgery, or retinal diseases. A detailed eye check and Optical Coherence Tomography (OCT) are vital for the right treatment.
In summary, ERM can greatly affect daily life. But, new surgery methods have made treatments better. Knowing about ERM helps people deal with their diagnosis and treatment. This way, they can keep their vision and quality of life.
FAQ
What is Epiretinal Membrane (ERM) in ophthalmology?
Epiretinal Membrane (ERM) is a condition where a layer of fibrous tissue forms on the retina. This can cause visual disturbances.
How serious is Epiretinal Membrane?
ERM can be mild or severe. It can cause significant vision problems and affect your quality of life.
What are the common causes of Epiretinal Membrane?
ERM can be caused by several things. These include posterior vitreous detachment, post-surgical development, retinal vascular diseases, and inflammatory eye conditions.
What are the signs and symptoms of ERM?
Symptoms include visual disturbances like metamorphopsia and micropsia. These can affect your daily activities.
How is Epiretinal Membrane diagnosed?
Diagnosis involves a thorough eye examination and Optical Coherence Tomography (OCT). Other imaging techniques are also used to rule out other conditions.
What are the risk factors for developing ERM?
Risk factors include age, previous eye conditions and surgeries, systemic health conditions, and genetic predisposition.
What are the treatment options for Epiretinal Membrane?
Treatment options include observation, vitrectomy surgery, and membrane peeling techniques. The choice depends on the severity and impact of ERM.
What is the prognosis and long-term outlook for ERM?
The prognosis varies. Factors like visual recovery expectations, complications, recurrence rates, and outcomes all play a role in determining the long-term outlook.
Can Epiretinal Membrane cause vision loss?
Yes, ERM can cause vision loss. The extent varies among individuals and is considered with other retinal conditions.
How does ERM affect daily activities?
ERM can impact daily activities due to visual disturbances. It can affect tasks that require clear vision and reduce quality of life.
Is there a genetic predisposition to ERM?
There is evidence suggesting a genetic predisposition to ERM. Age and previous eye conditions are also risk factors.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK560703/