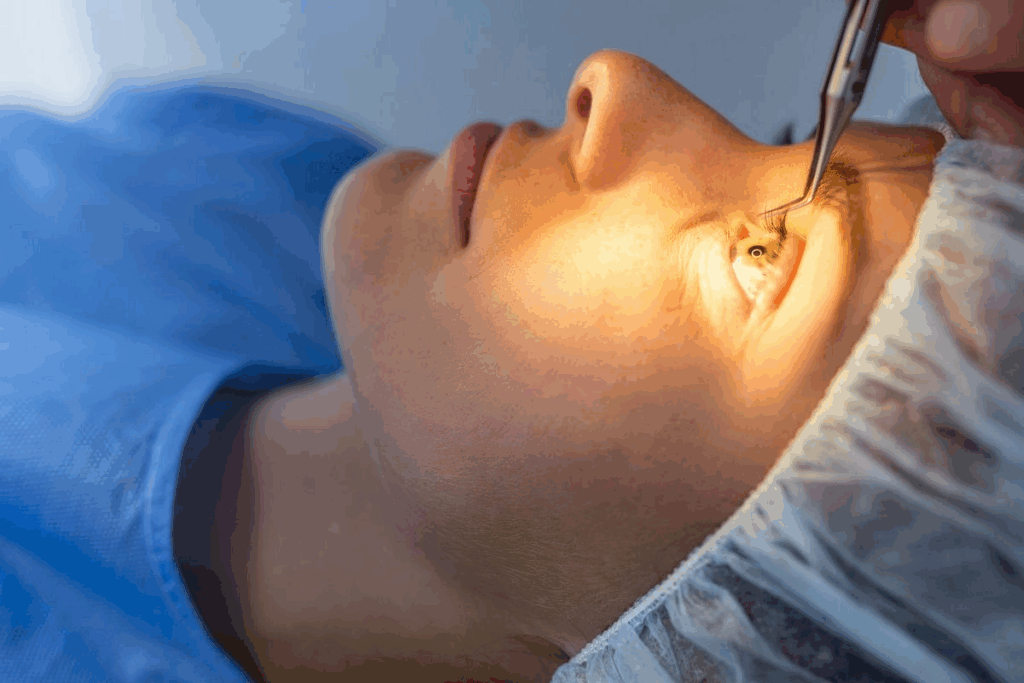
Spotting anterior chamber flare is key for diagnosing and treating serious eye problems. At Liv Hospital, our eye doctors use both old-school slit-lamp methods and new imaging tech. This helps them find and check this important sign with great care. Step-by-step method for recognizing flare in anterior chamber (protein leakage) during an eye examination. Spot flare in anterior chamber.
When proteins and other stuff mix with the aqueous humor, it looks cloudy. This is because the blood-aqueous barrier breaks down. Knowing how to spot flare in the eye is vital for eye health experts.
Key Takeaways
- Anterior chamber flare is a critical indicator of ocular inflammation.
- It is detected using slit-lamp biomicroscopy, revealing proteins and substances in the aqueous humor.
- The condition results from the breakdown of the blood-aqueous barrier, leading to a cloudy appearance.
- Accurate detection is key for diagnosing and managing eye inflammation.
- Liv Hospital’s eye specialists use advanced imaging for precise checks.
What Is Anterior Chamber Flare?
Anterior chamber flare is when proteins and other stuff show up in the aqueous humor. This means there’s inflammation in the eye. It’s very important for eye health and needs a close look.
We’ll dive into what anterior chamber flare is and why it matters. We’ll also look at how it shows up during a slit-lamp exam.
Definition and Clinical Significance
Anterior chamber flare makes the aqueous humor look cloudy because of proteins and other stuff. It’s a big deal because it shows the eye is inflamed. This can mean there’s an eye disease.
The flare is seen because of the Tyndall effect. This is when light scatters off particles in the aqueous humor.
Protein Exudation and the Tyndall Effect
The Tyndall effect happens when light scatters off tiny particles. In the case of anterior chamber flare, it’s because of proteins and stuff leaking into the aqueous humor because of inflammation.
Condition | Description | Clinical Significance |
Anterior Chamber Flare | Presence of proteins and substances in aqueous humor | Indicates ocular inflammation |
Tyndall Effect | Scattering of light by particles in aqueous humor | Makes flare visible during slit-lamp examination |
The Pathophysiology Behind Flare in Anterior Chamber
[Add image here]
Inflammatory processes in the eye can disrupt the blood-aqueous barrier. This leads to flare in the anterior chamber. It’s key to understanding eye inflammation.
Blood-Aqueous Barrier Disruption
The blood-aqueous barrier keeps the aqueous humor clear. When it’s disrupted, proteins and substances leak into the aqueous humor. This causes flare. Many factors can cause this disruption, like inflammation, trauma, or surgery issues.
A study on eye inflammation found, “The blood-aqueous barrier’s integrity is vital for eye function.”
The blood-aqueous barrier controls what molecules enter the aqueous humor.
Condition | Effect on Blood-Aqueous Barrier | Resulting Flare |
Inflammation | Increased permeability | Moderate to severe flare |
Trauma | Disruption due to injury | Variable flare |
Surgical complications | Post-operative inflammation | Mild to moderate flare |
Inflammatory Mediators and Protein Leakage
Inflammatory mediators are key in breaking the blood-aqueous barrier. They cause protein leakage into the aqueous humor, leading to flare. Flare shows how severe the eye inflammation is.
Understanding inflammatory mediators is vital for treating flare. By focusing on these mediators, we can lessen flare’s severity. This improves patient results.
Clinical Conditions Associated with Anterior Chamber Flare
It’s important to know the clinical conditions linked to anterior chamber flare for accurate diagnosis and treatment. This flare is a key sign of many eye problems. Recognizing these conditions is vital for proper care.
Anterior Uveitis and Iritis
Anterior uveitis and iritis are inflammatory eye diseases often seen with anterior chamber flare. These conditions cause inflammation in the uvea. This inflammation can break the blood-aqueous barrier, letting proteins leak into the anterior chamber.
Key features of anterior uveitis and iritis include:
- Inflammation of the uveal tract
- Disruption of the blood-aqueous barrier
- Presence of flare and cells in the anterior chamber
- Potential for complications such as synechiae and secondary glaucoma
Trauma-Induced Flare
Eye trauma can disrupt the eye’s structures, causing flare in the anterior chamber. The severity of the trauma affects the flare’s extent and complications.
Trauma-induced flare can result from:
- Blunt trauma causing mechanical disruption
- Penetrating injuries leading to direct damage
- Post-traumatic inflammation and healing responses
Post-Surgical Inflammation
Post-surgical inflammation is another common cause of anterior chamber flare. After eye surgery, the eye heals by inflaming and releasing inflammatory mediators.
Factors influencing post-surgical flare include:
- The type and complexity of the surgical procedure
- The extent of tissue trauma during surgery
- The patient’s individual healing response
Understanding these conditions helps us diagnose and manage patients with complex eye problems better.
Essential Equipment for Detecting Flare
To find flare in the anterior chamber, you need specific tools. Knowing how to use these tools is key.
Slit-Lamp Requirements
A slit-lamp biomicroscope is the main tool for spotting flare. It gives a close-up look at the front part of the eye. This lets you see flare clearly.
The slit-lamp must have a strong light and a zoom feature. This helps you see everything clearly during the exam.
Examination Room Setup
The room setup is important for finding flare. The room should be dimly lit. This cuts down on glare and makes the slit-lamp image clearer.
The slit-lamp should be placed for easy access and comfort. This makes the exam smooth and accurate.
It’s also good to have a slit-lamp that can be adjusted. This way, it fits the patient’s needs perfectly. This setup helps the doctor check for flare accurately.
Step-by-Step Technique for Identifying Flare in the Anterior Chamber
Identifying flare in the anterior chamber needs careful patient prep and precise slit-lamp use. We follow a detailed method. This includes getting the patient ready, setting up the slit-lamp right, and observing closely.
Patient Preparation and Positioning
Getting the patient ready is key for spotting flare. First, we make sure they’re comfy and in the right spot at the slit-lamp. We adjust the chin rest and forehead support to keep their head steady. Their eyes should match the slit-lamp’s level.
We tell the patient to stay calm and not move too much during the test.
Optimizing Slit-Lamp Settings
To see flare well, we tweak the slit-lamp settings. We adjust the beam’s width, height, and brightness. A thin beam with lots of light works best for flare.
We also make sure the slit-lamp is focused on the right spot. The magnification should be just right for a clear view without too much glare.
The main settings to adjust are:
- Beam width: Narrow for better contrast
- Beam height: Adjusted to cover the area of interest
- Illumination intensity: High to enhance visibility
- Magnification: Sufficient for clear visualization
Observation Methodology
With the patient ready and the slit-lamp set, we start observing. We scan the anterior chamber carefully, moving the beam across. This helps spot flare areas.
We look for the Tyndall effect, which shows up as light scattering by proteins in the aqueous humor. This means flare is present.
To improve our view, we use a few tricks:
- Compare the flare in the affected eye with the other eye, if possible.
- Look at the flare in different lights.
- Notice any other things in the anterior chamber, like cells or pigment.
By following these steps and using the slit-lamp well, we can spot flare accurately.
Spotting flare right is vital for diagnosing and treating eye problems. By mastering this technique, eye doctors can do better at diagnosing and caring for patients.
Standardized Grading Systems for Flare Assessment
Standardized grading systems are key for consistent flare assessment in the anterior chamber. They help doctors track flare over time. This is vital for managing eye inflammation well.
SUN Working Group Classification
The SUN Working Group Classification is a widely accepted grading system for flare. It offers a systematic way to measure flare severity. This makes it easier for healthcare professionals to document and communicate flare levels.
Key features of the SUN Working Group Classification include:
- Standardized grading scale for flare intensity
- Clear criteria for grading flare from 0 to 4+
- Guidelines for documentation and monitoring
Grade | Flare Intensity | Description |
0 | None | No flare detected |
1+ | Faint | Slightly detectable flare |
2+ | Moderate | Clearly visible flare |
3+ | Marked | Prominent flare |
4+ | Very marked | Severe flare |
Documentation and Monitoring Protocols
Effective documentation and monitoring are key for tracking flare changes. This means recording flare grade at each visit and noting any changes or trends.
Best practices for documentation include:
- Using a standardized grading system consistently
- Recording flare grade at each visit
- Noting any changes or trends in flare severity
Advanced Diagnostic Methods for Quantifying Flare
Laser flare photometry is a key tool for measuring flare. It gives us an accurate way to see how severe eye inflammation is. This method has greatly improved our ability to understand and treat eye problems.
Laser Flare Photometry Principles
Laser flare photometry detects light scattered by proteins in the eye’s fluid. The Tyndall effect is the science behind it. It measures how light scatters when it hits tiny particles, like proteins in the eye.
The device sends a laser beam into the eye’s front part. It then catches the light scattered by proteins. This gives us a number that shows how much flare there is. It’s very good at catching small changes in protein levels.
Interpreting Laser Flare Photometry Results
To understand laser flare photometry results, we look at the protein levels. Results are shown in photon counts per millisecond (pc/ms). More photon counts mean more proteins, which means more flare.
Doctors use these results along with what they see and what the patient says. This way, they can figure out the best treatment. It helps them get a full picture of the patient’s health.
With laser flare photometry, we can measure flare more accurately. This helps us track how the disease is changing and if treatments are working. It’s a powerful tool for managing eye inflammation.
Differentiating Flare from Other Anterior Chamber Findings
It’s important for eye care professionals to know how to tell flare apart from other things in the anterior chamber. Getting the diagnosis right is key for good treatment and care.
Cells vs. Flare: Key Distinctions
One big challenge is telling flare apart from cells in the anterior chamber. Both show inflammation, but in different ways.
Cells show inflammation directly, meaning they are leukocytes and other cells in the chamber. Flare shows protein leaking into the aqueous humor because of a broken blood-aqueous barrier.
Characteristics | Cells | Flare |
Appearance | Discrete, floating particles | Diffuse haziness or cloudiness |
Indication | Presence of inflammatory cells | Protein leakage into aqueous humor |
Clinical Significance | Direct indicator of inflammation | Measure of blood-aqueous barrier disruption |
Mimicking Conditions and Artifacts
Some things can look like flare or make it hard to see. Knowing these can help doctors make the right call.
“The accurate assessment of flare is critical for diagnosing and managing ocular inflammation. Clinicians must be aware of the potential for mimicking conditions and artifacts that can complicate the diagnosis.” –
Ocular Inflammation Expert
Some things that can look like flare include:
- Vitreal or retinal detachment-related protein leakage
- Post-surgical or traumatic aqueous flare
- Artifact due to improper slit-lamp settings
To really tell flare apart from these look-alikes, doctors need to do a detailed check and think about the patient’s history.
Clinical Significance of Flare in Anterior Chamber
Understanding flare in the anterior chamber is key for managing eye diseases. Flare is not just a simple finding. It has big implications for patient care and treatment success.
Correlation with Disease Activity
The intensity of flare shows how active eye diseases are. Higher flare values mean more severe inflammation. This can cause serious problems if not treated right.
In diseases like anterior uveitis, flare shows how bad the inflammation is. This info helps doctors choose the right treatment. It might include anti-inflammatory meds or other steps.
Prognostic Value in Ocular Inflammation
Flare also tells us about the future of eye inflammation. The more flare, the higher the risk of serious problems. Patients with high flare values are more likely to face issues like synechiae or cystoid macular edema.
By measuring flare, we can spot who needs stronger treatment to avoid lasting damage. This info is key for making better decisions and improving patient results.
In short, flare in the anterior chamber is important for knowing disease activity and future risks. By managing flare well, we can better care for patients and get better results.
Common Challenges in Flare Assessment
Getting flare assessment right is tough for doctors. They face many hurdles to give the best care to patients. Checking the flare in the front part of the eye is key to fighting eye inflammation. But, it’s not easy.
Technical Difficulties and Solutions
One big problem is technical issues. The quality of the slit-lamp exam can be affected by many things. This includes how well the patient cooperates, the doctor’s skill, and the equipment’s state. To fix this, keeping slit-lamp equipment in good shape and training doctors well are vital.
Another issue is that flare assessment is not always clear-cut. Doctors with different levels of skill might see things differently. To solve this, tools like the SUN Working Group Classification help standardize how flare is graded.
Technical Difficulty | Solution |
Poor slit-lamp quality | Regular equipment maintenance |
Variability in examiner expertise | Standardized training programs |
Subjective assessment | Use of standardized grading systems |
Reducing Inter-Observer Variability
Another big challenge is when different doctors see things differently. This can lead to mixed-up diagnoses and treatment plans. To tackle this, training doctors together and regular practice are key.
“Standardization and training are key to reducing variability in flare assessment and improving patient outcomes.”
— Expert in Ophthalmology
By tackling these issues with solutions like standard grading, training, and practice, we can make flare assessment more accurate. This helps patients get better care and better results.
Case Studies: Identifying Various Degrees of Flare
Case studies give us a close look at flare in the anterior chamber. They help us understand how flare affects our eyes. This knowledge is key to keeping our eyes healthy.
Mild Flare Presentation
A 45-year-old man had mild flare after cataract surgery. We found it with a slit-lamp exam. His vision was 20/30.
We treated him with eye drops. The flare went away in two weeks.
Mild flare characteristics: A bit of protein leak, a slight Tyndall effect, and it didn’t hurt his vision much.
Moderate Flare Characteristics
A 30-year-old woman had flare from uveitis. The slit-lamp showed a clear Tyndall effect. Her vision was 20/60.
We started her on anti-inflammatory meds. The flare got better in a month.
Moderate flare characteristics: More protein leak, a clear Tyndall effect, and it really affected her vision.
Severe Flare Examples
A 60-year-old man had severe flare after complicated surgery. The slit-lamp showed a big Tyndall effect. His vision was badly hurt.
Severe flare characteristics: A lot of protein leak, a big Tyndall effect, and it really hurt his vision.
Conclusion
Knowing how to spot flare in the anterior chamber is key for eye doctors. It helps them figure out and treat eye inflammation. We’ve looked into what flare is, why it matters, and how to find it, showing its big role in patient care.
The role of flare in the anterior chamber is huge. It shows how active an eye disease is and helps predict its future. By knowing how flare works and using clear grading systems, we can give better care to our patients.
To wrap it up, being good at finding and checking flare in the anterior chamber is vital. It helps us manage eye inflammation well. We stress the need for ongoing learning and practice in this field to improve patient care.
FAQ
What is anterior chamber flare?
Anterior chamber flare is when proteins and other substances mix with the aqueous humor. This makes the area look cloudy because the blood-aqueous barrier breaks down.
How is flare detected in the anterior chamber?
Doctors use a slit-lamp biomicroscope to spot flare. This tool shows proteins and other substances in the aqueous humor, causing light to scatter.
What is the Tyndall effect?
The Tyndall effect is when light scatters off particles in the aqueous humor. This makes flare visible when using a slit-lamp.
What conditions are associated with anterior chamber flare?
Flare can happen with anterior uveitis, iritis, trauma, or after surgery. These conditions cause inflammation in the eye.
How is flare assessed and graded?
Doctors use grading systems like the SUN Working Group Classification to measure flare. This helps track flare over time.
What is laser flare photometry?
Laser flare photometry is a tool that measures flare. It detects how much light scatters off proteins in the aqueous humor.
How do you differentiate flare from cells in the anterior chamber?
Flare and cells are different. Flare scatters light due to proteins and substances. Cells are distinct particles.
What are the challenges in assessing flare?
Assessing flare can be tricky. It’s hard to get accurate readings due to technical issues and observer variability. Standardized systems and training help improve accuracy.
What is the clinical significance of flare in ocular inflammation?
Flare shows how active an eye inflammation is. It helps predict complications and guides treatment.
How can flare assessment be improved?
To better assess flare, use standardized systems and train observers. Advanced tools like laser flare photometry also help.
What is the role of slit-lamp biomicroscopy in detecting flare?
Slit-lamp biomicroscopy is key for spotting flare. It lets doctors see the anterior chamber and detect substances in the aqueous humor.
Can flare be present without ocular inflammation?
Yes, flare can happen without inflammation. It can also occur due to trauma or after surgery, not just because of inflammation.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32255392/



