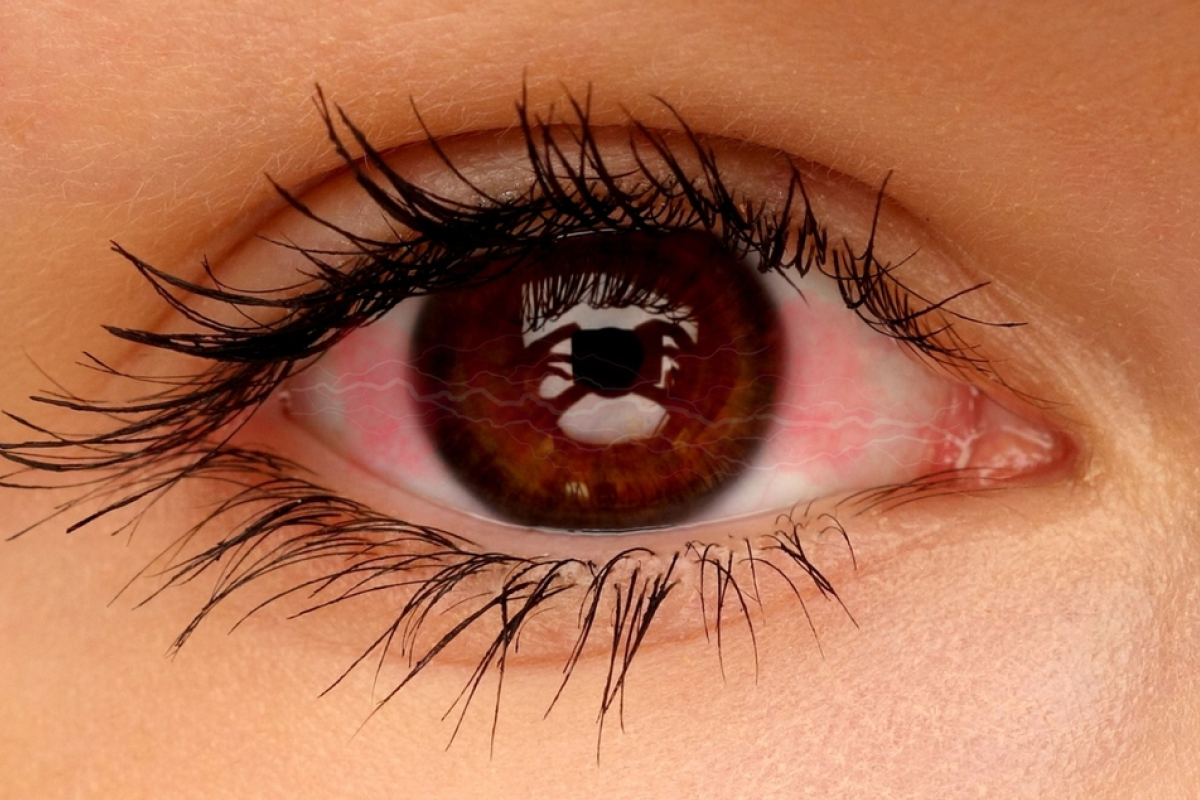
Recovering from retinal detachment surgery with a gas bubble is key. The surgery removes the vitreous humor to fix the retina. A gas bubble is then put in to keep the retina in place while it heals. Essential face-down positioning for healing when recovering from retinal detachment gas bubble surgery. Master retinal detachment gas bubble recovery.
It’s important to stay in a face-down position to heal well. This guide will help you understand how to sleep after surgery. It covers how to position yourself for comfort.
Key Takeaways
- Maintaining a face-down position is key after surgery.
- A gas bubble helps keep the retina in place while it heals.
- Knowing the recovery process can greatly improve results.
- Proper positioning is important for the best vision recovery.
- Following post-surgery instructions is very important.
Understanding Retinal Detachment Surgery

It’s important for patients to understand retinal detachment surgery. This surgery aims to attach the retina to the back of the eye. It uses gas bubbles to help the healing process.
What Happens During Retinal Detachment Repair
During the surgery, the doctor might use different methods. These include scleral buckling, vitreoretinal surgery, or pneumatic retinopexy. The method chosen depends on the detachment’s severity and location. The main goal is to fix the retina and stop vision loss.
The surgery removes blood or debris from the eye. Then, the doctor attaches the retina with a gas bubble. This bubble acts like a bandage, helping the retina stick back in place.
The Role of Gas Bubbles in Recovery
Gas bubbles are key in the healing process after surgery. They help the retina attach by providing pressure. The gas used can be air, sulfur hexafluoride (SF6), or perfluoropropane (C3F8), each with different lifespans.
“The gas bubble needs to float upward and press against the correct part of the retina. That’s why patients are told to stay face-down. This helps gravity place the gas bubble correctly.”
Expected Timeline for Healing
The time a gas bubble stays in the eye varies. Air bubbles last about five to seven days. Sulfur hexafluoride (SF6) can last ten to thirty days. Perfluoropropane (C3F8) stays for six to eight weeks. Knowing this helps patients plan their recovery.
Gas Type | Duration |
Air | 5-7 days |
Sulfur Hexafluoride (SF6) | 10-30 days |
Perfluoropropane (C3F8) | 6-8 weeks |
The Importance of Retinal Detachment Gas Bubble Treatment
Gas bubbles are key in retinal detachment surgery. They act as a temporary support, helping the retina heal and attach properly.
How Gas Bubbles Work as Temporary Tamponades
During surgery, gas bubbles are injected into the eye. They hold the retina in place until it heals. This is vital for the retina to attach correctly and prevent further detachment.
After surgery, patients must keep their face down. This can last from a few days to two weeks. The exact time depends on where the retinal break is.
Types of Gas Bubbles: Air, SF6, and C3F8
There are different gases used in retinal detachment surgery. These include air, sulfur hexafluoride (SF6), and perfluoropropane (C3F8). The choice depends on the patient’s needs and the surgeon’s preference.
- Air bubbles are absorbed quickly, usually within a few days.
- SF6 gas bubbles last longer, typically remaining in the eye for 1-2 weeks.
- C3F8 gas bubbles have the longest duration, often lasting 6-8 weeks.
Duration Expectations: From Days to Weeks
The time a gas bubble stays in the eye varies. Most see vision improvements in four to six weeks. But, full healing can take up to a year.
Following your doctor’s post-operative instructions is critical. This includes keeping your face down. A gas bubble can affect your vision and daily life. But, with proper care, these challenges can be managed.
Why Face-Down Positioning Is Critical After Surgery
The need to lie face-down after retinal detachment surgery is not random. It’s based on science that helps healing. This position is key because it lets the gas bubble from surgery push against the retina. This helps it stick back in place.
The Science Behind Positioning Requirements
The rules for lying down come from where the retina broke and the gas used. The gas bubble acts like a temporary bandage, keeping the retina in place until it heals. By staying in the right position, patients make sure the gas stays in contact with the retina. This helps it heal properly.
Different gases last for different times. For example, air goes away fast, but gases like SF6 and C3F8 last longer. The gas used depends on the detachment’s complexity and location. This affects how long patients need to stay in the face-down position.
How Positioning Affects Retinal Healing
Right positioning is key for healing. When patients lie face-down, the gas bubble presses gently against the retina. This pressure helps it stick back in place. This is important to avoid problems like the retina detaching again or a macular hole not sealing properly.
By sticking to the recommended position, patients can greatly improve their recovery chances. It’s vital to follow the exact instructions from the healthcare team. These are made just for the patient’s specific situation.
Consequences of Not Following Positioning Instructions
Ignoring the positioning rules can cause serious issues. If the retina doesn’t heal right, it might detach again. Also, if a macular hole doesn’t seal fully or the gas bubble moves, it can lead to vision problems or even surgery failure.
It’s important for patients to know how they play a big part in their recovery. By following the positioning rules, patients can lower the risk of problems. This ensures the best results for their surgery.
Determining Your Face-Down Positioning Schedule
The time you need to stay face down after retinal detachment surgery varies. It depends on how bad the detachment is and the size of the gas bubble used. Usually, you’ll need to stay face down for 5 to 14 days. Sometimes, your doctor might ask you to do it for a week or two more.
Positioning Requirements Based on Break Location
The spot where the retinal break is matters a lot. If it’s in the top part of your retina, you’ll need to stay face down. This helps the gas bubble push against the detached area. But if it’s in the bottom part, you might not need to stay face down as long.
Remember, the positioning plan is made just for you. Your doctor will decide based on your specific situation. They’ll look at the size and location of the detachment and the gas used.
Working With Your Doctor to Create a Positioning Plan
It’s important to work with your doctor to make a plan that’s right for you. They’ll tell you how to stay in the right position, even when you’re sleeping or eating. It’s key to follow these instructions to help your retina heal right.
Sticking to the positioning plan is very important. By understanding why you need to stay face down and working with your team, you can help your surgery succeed. This will make your recovery better and increase your chances of a good outcome.
Essential Equipment for Face-Down Recovery
The right equipment can greatly improve comfort and success in face-down recovery. After retinal detachment surgery, patients must stay face-down for a long time. This can be hard without the right support.
Face-Down Positioning Chairs and Supports
Face-down positioning chairs offer comfort and support during recovery. They have adjustable features for different body types and preferences. These chairs help keep the right posture, easing neck and back strain.
Supports are also key for keeping the patient’s position stable. They can be used with chairs or alone, based on the patient’s needs.
Specialized Pillows and Cushions
Specialized pillows and cushions are vital for comfort in face-down recovery. They are made to support the head and body in the right position. This reduces discomfort and pressure points.
Some pillows have cutouts or contours for breathing and vision while staying face-down. Cushions support the knees or legs, easing strain and boosting comfort.
Rental vs. Purchase Options for Recovery Equipment
Patients can choose to rent or buy recovery equipment. Renting is often cheaper, great for those needing it short-term. Rental services offer various options and flexible periods.
Buying equipment might be better for those needing it long-term or frequently. It’s important to talk to healthcare providers to find the best option for your recovery needs.
Setting Up Your Recovery Space at Home
After retinal detachment surgery, creating a recovery space at home is key. It should be both comfortable and safe. A well-prepared environment can greatly help your healing.
Creating a Comfortable Recovery Station
First, find a comfy spot to rest and stay face-down. Use a chair with good support or a face-down positioning system. Stacked pillows or a face-down pillow can add to your comfort. Place a mirror on a table to watch TV or talk to others without hurting your neck.
Organizing Necessities Within Reach
Make sure all you need is close by. Keep your phone, water, snacks, and meds within arm’s length. A bedside table or tray is great for this. It lets you reach for things without getting up or straining.
Safety Considerations for Limited Visibility
Safety is a big deal when you can’t see well. Clear your space of tripping hazards and make sure it’s bright. A flashlight or nightlight can help at night. Having someone to help you is also a big plus.
Setting up your recovery space right can make a big difference. It helps you stay comfortable and safe. This focus on healing can reduce the chance of problems.
How to Sleep After Retinal Detachment Surgery
After retinal detachment surgery, finding a good sleeping position is hard. The need to sleep face-down can be tough. But, the right tools and methods can make it easier and follow the doctor’s advice.
Face-Down Sleeping Positions and Techniques
Face-down sleeping is key for recovery after retinal detachment surgery. To sleep comfortably, patients can use special equipment. This equipment helps keep the body in the right position.
Using a face-down support at the bed is a good method. It lets patients rest their face on a soft surface while keeping their body right. Three-pad faceplate systems also offer support and comfort.
Using Specialized Pillows and Face Cradles
Special pillows and face cradles are important for face-down sleeping. They are made to hold the face and support the head. This reduces neck strain and helps sleep better.
Extra pillows can also help support the body. Placing pillows under the arms, chest, or legs helps keep a stable and comfy position.
Side-Sleeping Alternatives (When Approved by Doctor)
In some cases, doctors might say it’s okay to sleep on your side instead. But, this should only be done if a doctor says it’s okay. It might not be good for everyone.
If side-sleeping is okay, patients can use body pillows or special side-sleeping supports. These help keep a comfy position and lessen strain on the operated eye.
Managing Discomfort During Sleep
It’s important to manage discomfort for a good recovery. Patients can try different things to feel better. This includes changing how they sleep, using more pillows, or trying relaxation techniques.
Following the doctor’s advice on pain management is also key. If discomfort doesn’t go away or gets worse, tell the doctor.
Daily Activities During Face-Down Recovery
Patients with retinal detachment surgery need to adjust their daily life. They must follow the face-down positioning rule. This can be tough, but with the right strategies, it’s doable.
Eating and Drinking While Maintaining Position
Drinking and eating in the face-down position is tricky. But, there are ways to make it easier. Drinking with a straw helps avoid tilting the head back. For eating, a lap tray or a special eating device can help keep the face down.
Meal Type | Suggestions |
Breakfast | Oatmeal, yogurt, or smoothies that can be consumed with a straw or spoon while face-down. |
Lunch/Dinner | Soups, pureed foods, or meals that can be eaten with a fork or spoon without needing to tilt the head. |
Snacks | Fruit purees, energy bars, or snacks that don’t require much preparation or utensils. |
Personal Hygiene Challenges and Solutions
Keeping clean is key during recovery. Wet wipes can be used for face and body cleaning. A handheld showerhead makes showering easier without standing up or tilting the head.
Tips for Personal Hygiene:
- Use a mirror or periscope to see while shaving or applying makeup.
- Keep hygiene products within easy reach to minimize movement.
- Consider enlisting the help of a caregiver for tasks that are challenging.
Entertainment and Passing Time Face-Down
Staying entertained is important for mental health during recovery. Listening to audiobooks, podcasts, or music is a good way to pass time. Watching TV or movies on a tablet or smartphone is also possible without tilting the head.
Taking Prescribed Medications Safely
Following the medication schedule is key for recovery. Keep medications in an easy spot and use a pill box or reminder. If pills are hard to swallow, talk to your doctor about other options.
By adjusting daily routines and using the right tools, patients can manage face-down recovery after retinal detachment surgery.
Managing Physical and Emotional Challenges
Recovering from retinal detachment surgery means dealing with both physical and emotional challenges. You’ll face neck and back pain, and the emotional toll of being stuck in one position for a long time. It’s important to tackle these issues head-on.
Neck and Back Pain Relief Strategies
Neck and back pain are common during face-down recovery. Here are some ways to ease these pains:
- Regular Massages: Gentle massages can help loosen up tight muscles in your neck and back. You might want to get a professional or ask a family member to help.
- Gentle Stretching: Once your doctor says it’s okay, try some gentle stretches. This can help keep your muscles flexible and reduce pain.
- Ergonomic Support Tools: Use pillows and chairs made for face-down recovery. They can help keep your body in the right position.
Preventing Pressure Sores
Staying in one position for too long can cause pressure sores. Here’s how to avoid them:
- Move a little bit when your doctor says it’s okay.
- Use cushions and pillows to spread out the pressure.
- Keep your skin clean and dry to prevent irritation.
Coping With Isolation and Frustration
Being stuck in one position can be tough. Here are some ways to cope:
- Stay Connected: Make regular phone calls, video chats, and use social media to stay in touch with loved ones.
- Engage in Activities: Read, watch movies, or do other hobbies to keep your mind busy and distract you from discomfort.
- Seek Support: Look into support groups or online forums for people going through similar experiences.
When to Seek Help for Positioning-Related Issues
If you’re in constant pain or discomfort, or have concerns about your position, reach out to your healthcare provider. They can adjust your recovery plan and offer support.
By using these strategies, you can manage the physical and emotional challenges of face-down recovery. This will help make your recovery process better.
Monitoring Your Recovery Progress
After retinal detachment surgery, it’s important to watch your recovery closely. As the gas bubble in your eye goes away, your vision will change. It’s key to notice these changes and any possible problems.
Understanding Vision Changes as the Bubble Absorbs
As the gas bubble disappears, your vision might seem blurry or off. It’s normal for your vision to be blurry or distorted until the bubble is fully gone. Keeping a log of your vision changes is a good idea to talk about with your doctor later.
“The gas bubble absorbs at different rates for everyone,” says Medical Expert, a well-known eye doctor. “Usually, it starts to go away a few days to a week after surgery. But it can take several weeks for it to fully absorb.”
Recognizing Warning Signs and Complications
While you’re recovering, watch out for signs of trouble. Symptoms to watch for include:
- Increasing pain or discomfort
- Flashing lights or new floaters
- A sudden decrease in vision
- Increased sensitivity to light
If you notice any of these signs, get in touch with your doctor right away.
Follow-up Appointment Expectations
Going to your follow-up appointments is very important. Your doctor will check your eye, see how the gas bubble is doing, and look for any complications. We suggest asking questions and sharing any worries you have during these visits.
Typical Vision Improvement Timeline
Most people start to see their vision get better in four to six weeks after surgery. But it can take a year or more for the retina to fully heal. Being patient and following your doctor’s advice is very important. Keep a positive attitude and focus on getting better.
“The recovery can be tough, but most of our patients see a big improvement in their vision,” says Medical Expert, an expert in fixing retinal detachments. “By keeping an eye on your recovery and following your doctor’s advice, you can help your healing go smoothly.”
Conclusion: Life After Face-Down Recovery
Recovering from retinal detachment surgery takes time and following a recommended plan. Patients face challenges with face-down positioning but are on the path to healing and better vision.
With the right care and sticking to the recovery plan, patients can see great results. Life after recovery is a big achievement, ending a tough journey and starting a new chapter with better eye health.
As the gas bubble is absorbed and vision improves, patients will see their sight get better. It’s important to keep up with doctor’s appointments to check on progress and solve any issues. This helps patients smoothly move into life after retinal detachment recovery.
We know the recovery journey is tough, but with the right support and guidance, patients can succeed. Remember, being patient and following the recovery plan are essential for the best results in retina surgery recovery.
FAQ
What is the purpose of a gas bubble in retinal detachment surgery?
The gas bubble acts as a temporary fix. It helps the retina stick back in place while it heals.
How long do I need to maintain face-down positioning after vitrectomy?
Face-down time varies. It depends on where the retinal break is and the gas type used. It can be a few days to weeks.
What types of gas bubbles are used in retinal detachment surgery?
Air, SF6, and C3F8 are common. Each gas absorbs at a different rate.
How do I sleep comfortably after retinal detachment surgery?
Use special pillows or face cradles for comfort. Adjust your sleep area to reduce discomfort.
Can I rent or buy equipment for face-down recovery?
Yes, you can rent or buy chairs, supports, and pillows. They make recovery easier.
How do I manage daily activities while maintaining face-down positioning?
Keep things within reach. Use adaptive methods for eating and hygiene. Find ways to stay entertained while in the required position.
What are the consequences of not following face-down positioning?
Ignoring the position can harm healing. It may lead to complications or more surgery.
How will I know if my vision is improving after retinal detachment surgery?
Vision gets better slowly. Regular check-ups with your doctor are key. They help track your progress and address any issues.
How long does it take for the gas bubble to absorb after retinal detachment surgery?
Absorption time varies. Air absorbs quickly, while C3F8 takes weeks.
What should I do if I experience discomfort or pain during face-down recovery?
Follow your doctor’s pain relief advice. Adjust your equipment as needed. Seek help for persistent or severe pain.
Can I take a shower or bath while maintaining face-down positioning?
Yes, you can shower or bathe. Use special equipment or techniques to keep your face and eyes dry.
How do I prevent pressure sores during face-down recovery?
Change positions often. Use supportive gear. Follow your doctor’s advice on managing pressure points.
When can I resume normal activities after retinal detachment surgery?
Normal activity resumption varies. It depends on your recovery and your doctor’s specific instructions.
References
National Health Service (NHS). Retinal Detachment Surgery: Postoperative Sleep and Recovery Guide. Retrieved from https://www.nhs.uk/conditions/retinal-detachment/surgery/