After retinal detachment surgery, many patients ask about the best sleeping positions. At Liv Hospital, we know how important post-surgery care is. We give detailed advice to help our patients during this important time. Detailed guidance on whether can i sleep on my side after retinal detachment surgery is permitted during recovery.
It’s key to keep the right sleeping position after surgery. This ensures the gas or oil bubble in your eye stays in the best spot. Our team stresses the importance of following specific head positions for healing.
We’ll look into why post-surgery positioning is so important. We’ll also share tips on managing sleeping positions after retinal detachment surgery. This will help you understand this critical part of your recovery.
Key Takeaways
- Post-operative positioning is critical for successful recovery after retinal detachment surgery.
- Maintaining a face-down position is often recommended to ensure the gas or oil bubble is correctly positioned.
- Liv Hospital provides detailed post-operative guidance to support patients through their recovery.
- Strict adherence to specific head positioning protocols is necessary for optimal healing.
- Our medical team is dedicated to providing personalized care and support throughout the recovery process.
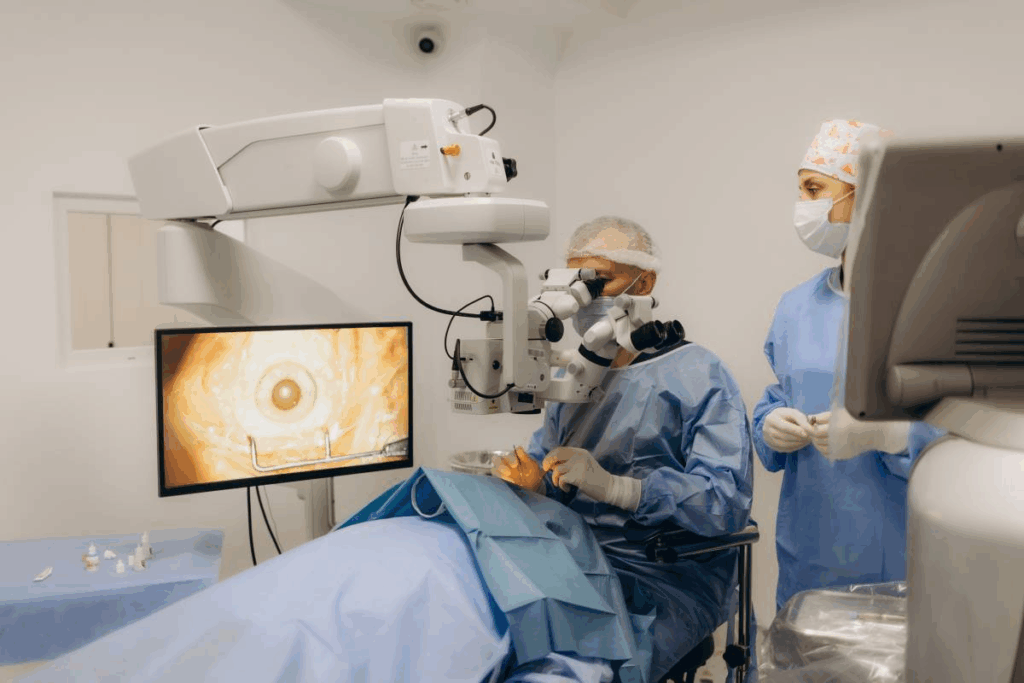
Understanding Retinal Detachment Surgery

It’s important for patients to understand retinal detachment surgery. This surgery aims to fix the retina to the back of the eye. It helps restore vision. Knowing the different techniques and materials used is key.
Types of Procedures: Vitrectomy and Pneumatic Retinopexy
There are two main surgeries for retinal detachment: vitrectomy and pneumatic retinopexy. Vitrectomy removes the vitreous gel and replaces it with gas or oil. This helps the retina attach back. It’s used for more serious cases.
Pneumatic retinopexy is simpler. It involves injecting a gas bubble to push the retina back. The choice depends on the detachment’s severity and location.
Procedure | Description | Typical Use Case |
Vitrectomy | Removal of vitreous gel, replaced with gas or oil | Complex retinal detachments |
Pneumatic Retinopexy | Injection of gas bubble to reattach retina | Less complex, localized detachments |
Gas Bubbles vs. Silicone Oil Tamponade
Gas bubbles or silicone oil tamponade are key in surgery. Gas bubbles are used in both types of surgery. They apply pressure to help the retina attach. The body absorbs the gas over time.
Silicone oil tamponade is for more serious cases. It’s not absorbed by the body and may need removal later.
“The choice between gas and silicone oil depends on the specific condition of the patient and the surgeon’s professional judgment.”
— Medical Expert, Ophthalmologist
Why Proper Positioning Matters for Recovery
After surgery, keeping the right position is vital. It helps the gas bubble or silicone oil stay in place. This aids in healing. Patients must follow a specific head position for a while.
Following the recommended position is important. It can help avoid complications and speed up recovery.
The Importance of Post-Surgery Positioning

Proper positioning after retinal detachment surgery is key for a good recovery. The way the patient is positioned after surgery is very important. It helps ensure the retina heals right.
After surgery, gas bubbles or silicone oil are often used to help the retina heal. Gas bubbles are very effective because they float up, pressing against the retina when the patient is face-down. This helps the detached retina attach back to its place.
How Gas Bubbles Support Retinal Healing
Gas bubbles help support the retina as it heals. When the patient is face-down, the gas bubble presses against the retina. This helps the retina attach back to the tissue underneath.
The Science Behind Face-Down Positioning
The science behind face-down positioning is based on the buoyancy of the gas bubble. The gas bubble is less dense than the fluid around it, so it floats up. By having the patient face-down, the gas bubble presses against the detached retina, helping it attach back.
Maintaining the face-down position can be hard, but it’s very important for the surgery’s success. Patients are usually told to stay in this position for a lot of their waking hours, at least in the first days after surgery.
Location of Retinal Break and Positioning Requirements
The location of the retinal break affects the needed positioning after surgery. For example, if the break is in the upper part of the retina, face-down is usually recommended. The exact positioning needed is based on the patient’s condition and the type of tamponade used.
Understanding the importance of post-surgery positioning and following the recommended positioning can greatly affect the outcome of retinal detachment surgery. By following the surgeon’s instructions, patients can improve their chances of a successful recovery.
Can I Sleep on My Side After Retinal Detachment Surgery?
Knowing the right sleeping position after retinal detachment surgery is key for healing. The surgery type and materials used, like gas bubbles or silicone oil, affect the recommended position.
Immediate Post-Surgery Sleeping Restrictions
Right after surgery, doctors usually tell patients not to sleep on their side. This is because the gas or oil bubble needs to stay in place. Sleeping on your side too soon can move the bubble, which might harm the retina’s reattachment.
In the first few days, patients are often told to sleep face-down. This helps keep the bubble in the right spot, aiding in healing.
When Side Sleeping May Be Permitted
When side sleeping is okay depends on how well you’re healing and the surgery type. Your doctor will give you specific advice based on your situation. As the retina heals and the bubble’s risk of moving goes down, you might start sleeping on your side.
It’s very important to listen to your surgeon about sleeping positions. Not waiting for your doctor’s okay to sleep on your side could risk the surgery’s success.
Factors That Determine Sleeping Position Recommendations
Many things affect the sleeping position advice after retinal detachment surgery. These include the tamponade type (gas bubble or silicone oil), the detachment location, and your health and healing.
- The size and location of the retinal break
- The type of surgical procedure performed (vitrectomy or pneumatic retinopexy)
- The surgeon’s professional judgment based on post-operative examinations
By sticking to the recommended sleeping positions and listening to your surgeon, you can improve your recovery chances.
Recommended Sleeping Positions Week by Week
Recovering from retinal detachment surgery needs careful attention to sleeping positions. These positions change over time. We’ll guide you through the best sleeping positions each week to help you recover smoothly.
First 24-48 Hours After Surgery
In the first 24-48 hours, you must sleep face-down. This helps the gas bubble or oil support the retina while it heals. Always follow your surgeon’s specific instructions during this time.
Days 3-7 Post-Surgery
By days 3-7, you might be able to adjust your sleeping position a bit. But, you should mostly stay face-down to support the healing retina. Always talk to your healthcare provider before making any changes.
Transitional Positioning Strategies
As you heal, you’ll start to move to different sleeping positions. This change should be slow and based on your surgeon’s advice. Keep an eye on your vision and tell your doctor about any changes or concerns.
Week 2 and Beyond
By week 2 and later, you might have more freedom in your sleeping positions. But, this depends on your healing and your surgeon’s advice. Always listen to your surgeon and watch for any discomfort or vision changes.
Face-Down Positioning Techniques
After retinal detachment surgery, patients must keep their face down to heal right. This can be tough, but with the right tools and advice, they can get through it.
Proper Head and Neck Alignment
Keeping your head and neck right is key in a face-down position. Correct alignment stops pain and neck problems. Make sure your spine is straight by using supports if needed.
A special pillow or support, like the RetinaRest, can really help. These items support your head and face, easing eye pressure and helping you heal.
Using Pillows and Supports Effectively
Pillows and supports are key for a comfy face-down position. Place pillows under your forehead, chest, or other spots to stay in position. Try different setups to find what works for you.
Using pillows right spreads your weight, easing neck and shoulder strain. This makes it easier to stay in the face-down position for longer.
Pictures and Illustrations of Correct Positions
Pictures or drawings show how to align your head and neck. They also show how to use pillows and supports.
Talking to your doctor or a medical expert can also help. They can give you specific advice on keeping the right position during recovery.
Equipment to Help With Proper Sleeping Positions
Recovering from retinal detachment surgery can be tough. But, the right equipment can help you stay in the right position. It’s key for healing well. There are many tools made to help patients get the right posture.
Specialized Recovery Chairs for Detached Retina
There are chairs made just for patients recovering from retinal detachment. These chairs adjust to fit each person’s needs. They also have features like reclining and support to make sitting more comfortable.
Key Benefits of Recovery Chairs:
- Adjustable positioning to accommodate different surgical requirements
- Enhanced comfort through ergonomic design
- Support for maintaining face-down positioning
Face-Down Pillows and Support Systems
Face-down pillows and support systems are vital for retinal detachment recovery. They help keep patients comfortable while keeping them in the right position.
Features to Look for in Face-Down Pillows:
- Soft, breathable materials for comfort
- Adjustable designs to accommodate different face shapes and sizes
- Durable construction to support long-term use
Rental vs. Purchase Options
Patients can choose to rent or buy recovery equipment. The choice depends on how long they need it, what they prefer, and their budget.
Rental Options | Purchase Options |
Cost-effective for short-term needs | More economical for long-term requirements |
Access to latest equipment without long-term commitment | Ownership and control over the equipment |
May include maintenance and support services | Potential for resale or reuse |
Knowing about the different equipment options can help patients make the best choice for their recovery. This way, they can support their healing from retinal detachment surgery.
Managing Comfort While Maintaining Proper Position
After retinal detachment surgery, it’s important to manage both position and comfort. This ensures the best healing. Patients need to find a balance between keeping the right position and avoiding discomfort and strain.
Pain Management Strategies
Managing pain well is key during recovery. We suggest a mix of medication and other methods to handle pain. You can use over-the-counter pain relievers as your surgeon advises. Also, cold compresses on the eye area can help with swelling and pain.
Key Pain Management Techniques:
- Using prescribed pain medication as directed
- Applying cold compresses to reduce swelling
- Resting in a comfortable, supported position
Preventing Neck and Back Strain
Long periods of face-down can strain your neck and back. To avoid this, use ergonomic support tools like special pillows and adjustable chairs. Gentle stretching, as okayed by your surgeon, can also help.
Tips for Reducing Strain:
- Using ergonomic support tools
- Performing gentle stretching exercises
- Adjusting your position periodically as allowed by your surgeon
Tips for Posturing After Eye Surgery
Correct posturing is vital for healing. We recommend using mirrors or visual aids to keep the right position. Having a caregiver help with positioning in the first few days is also beneficial.
Comfort Measure | Description | Benefit |
Pain Medication | Using prescribed medication as directed | Reduces post-operative pain |
Cold Compresses | Applying cold packs to the area around the eye | Reduces swelling and discomfort |
Ergonomic Supports | Using specialized pillows and adjustable chairs | Prevents neck and back strain |
Common Challenges and Solutions
Recovering from retinal detachment surgery can be tough. But, with the right strategies, patients can face common obstacles head-on. The post-surgery period often brings challenges that can affect recovery. Understanding these challenges and using effective solutions can improve the recovery experience and outcomes.
Dealing With Discomfort and Pain
Managing pain and discomfort is key during recovery. Patients may feel pain ranging from mild to severe, based on their surgery and individual response.
- Follow the pain management plan given by your doctor, which may include medication and other interventions.
- Use cold compresses to reduce swelling and ease discomfort.
- Keep the recommended position to lessen eye strain.
Talking to your healthcare provider about your pain is important. They can adjust your treatment plan as needed.
Managing Bathroom Breaks and Daily Activities
Even simple tasks like using the bathroom or doing daily activities can be hard after surgery. To manage these tasks well:
- Plan ahead by having necessary items within easy reach to minimize movement.
- Use adaptive equipment such as grabbers or long-handled tools to reduce strain.
- Have assistance available, specially during the initial recovery period.
By taking these precautions, patients can lower the risk of complications and make recovery easier.
Strategies for Getting Quality Sleep
Quality sleep is essential for recovery, but it can be hard due to the need for face-down positioning. To improve sleep quality:
- Use specialized pillows or support systems designed for face-down positioning.
- Create a comfortable sleep environment by adjusting lighting and temperature.
- Establish a relaxing bedtime routine to signal the body that it’s time to sleep.
By using these strategies, patients can improve their sleep quality. This is vital for healing and overall recovery.
Signs That Your Positioning May Be Incorrect
It’s important to know the signs of wrong positioning after retinal detachment surgery. You need to watch how your body reacts to the surgery and the healing position. We’ll talk about the main signs that show your positioning might not be right.
Physical Symptoms to Watch For
Physical signs can tell you if your positioning is off. Increased pain or discomfort in your eye or head means the retina might not be supported right.
Stiffness or strain in your neck or back from staying in one position too long is common. But, if the pain is bad or doesn’t go away, you might need to change how you’re sitting.
Vision Changes That Require Immediate Attention
Changes in your vision are a big sign of how well your positioning is working. If you see flashes of light, an increase in floaters, or a shadow descending over your vision, get medical help right away.
These signs could mean the retinal detachment is getting worse or there are other problems.
When to Contact Your Surgeon
If you notice any strange or worrying symptoms, call your surgeon fast. Keep a log of your symptoms to talk about with your surgeon. Include when they happen and how long they last.
Your surgeon can tell you if you need to change your position or if there are other issues to fix.
Combining Face-Down and Side Sleeping Techniques
After retinal detachment surgery, mixing face-down and side sleeping can help with recovery. Doctors might suggest changing sleeping positions as healing progresses. This ensures the best recovery.
“Flexibility and following recommended positions are key to recovery,” says Medical Expert, a top eye doctor. Patients need to adjust their sleep to aid healing.
Research on Combined Positioning Approaches
Studies have looked into mixing face-down and side sleeping for retinal detachment surgery. They found that a mix can improve recovery in some cases.
A study in the Journal of Ophthalmology showed that switching positions under doctor’s watch can lead to better recovery. This is as good as or better than staying in one position.
How to Safely Implement Physician-Approved Side Sleeping
When starting side sleeping after surgery, follow your doctor’s advice closely. Make sure the operated eye is not under pressure.
- Use pillows to support your head and body, keeping everything aligned and reducing strain.
- Avoid lying directly on the operated side unless your doctor says it’s okay.
- Watch how your body reacts to the new position and tell your doctor about any issues.
Monitoring Your Progress During Position Transitions
Keep an eye on how you’re doing when switching positions. Tell your doctor about any changes or worries. Regular check-ups are key to adjusting the plan as needed.
“Watching how patients do during position changes is vital for success,” says Medical Expert, a specialist in eye surgery. “By observing their responses, we can make the best decisions for their care.”
By mixing face-down and side sleeping under a doctor’s watch, patients can get the best recovery after surgery.
Conclusion: Ensuring Successful Recovery Through Proper Positioning
Proper positioning after retinal detachment surgery is key for a good recovery. By following post-operative instructions, patients can greatly improve their results. We’ve looked at the different parts of post-surgery positioning. It’s important to keep following these guidelines to help the retina heal right.
Sticking to the recommended positioning is vital for surgery success. Patients who keep the right position can lower the chance of problems and help healing. We urge patients to team up with their healthcare team to make sure they’re using the best positioning for their needs.
By using the right positioning and proper care after surgery, patients can have a successful recovery and get their vision back. We’re dedicated to helping patients through their recovery, giving them the tools and advice they need for the best results.
FAQ
Can I sleep on my side after retinal detachment surgery?
Right after surgery, it’s best not to sleep on your side. Your doctor will tell you what’s best. This depends on the surgery, the type of fluid used, and where the detachment is.
How long do I need to maintain a face-down position after retinal detachment surgery?
How long you need to lie face-down varies. It depends on your specific case and the fluid used. Your doctor will give you specific instructions.
What are the benefits of using a specialized recovery chair after retinal detachment surgery?
Special chairs can make recovery more comfortable. They help you stay in the right position. This reduces strain on your neck and back.
How can I manage discomfort and pain after retinal detachment surgery?
To manage pain, follow your doctor’s advice on medication. Use ergonomic supports and rest often. Keeping the right position also helps.
What are the signs that my positioning may be incorrect after retinal detachment surgery?
If you feel more pain, discomfort, or see vision changes, it might mean you’re not in the right position. Contact your doctor right away if you notice these signs.
Can I transition between face-down and side sleeping positions during recovery?
As you get better, your doctor might say it’s okay to switch positions. Always follow their advice and watch how your body reacts to these changes.
What type of equipment is available to support patients during their recovery?
There are many options, like special chairs, pillows, and supports. You can rent or buy them, based on what you need.
How can I prevent neck and back strain while maintaining a face-down position?
Use pillows and supports right, keep your head and neck straight, and rest often. Exercises and ergonomic aids can also help.
What are the recommended sleeping positions week by week after retinal detachment surgery?
Your sleeping position will change as you heal. You’ll start face-down, then move to other positions. Your doctor will guide you on the best position each week.
How do gas bubbles support retinal healing after retinal detachment surgery?
Gas bubbles help the retina heal. Lying face-down keeps the bubble in contact with the retina. This helps it reattach.
References
National Health Service (NHS). Sleeping Positions After Retinal Detachment Surgery. Retrieved from https://www.hey.nhs.uk/patient-leaflet/instructions-re-post-operative-posturing-following-retinal-surgery/







