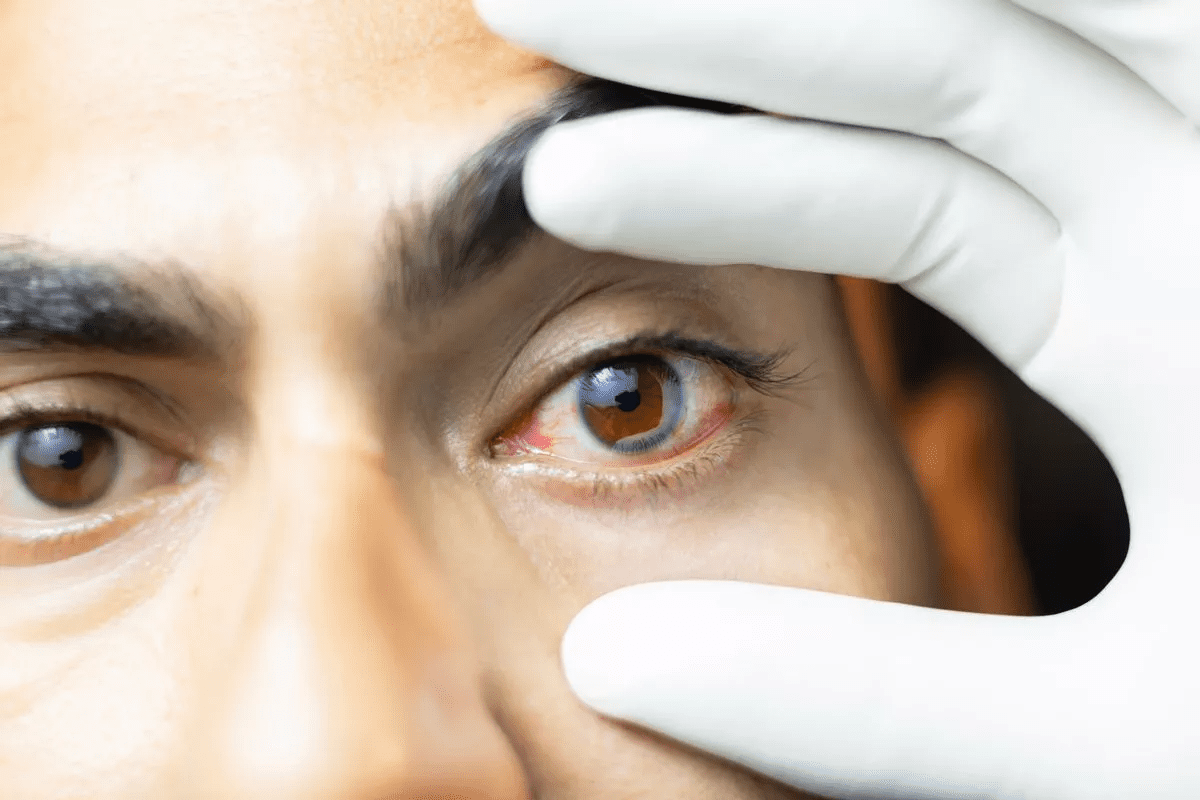
After retinal detachment surgery, patients face challenges in their recovery. They must manage their position to help the gas bubble in their eye heal. Proper care after surgery is key for a good outcome.Specific posturing instructions for sleeping when you have a gas in eyeball after retinal detachment surgery. Sleep with gas in eyeball.
The face-down position is vital during sleep and daily activities. It helps the gas in the eyeball heal. UHCW patient info shows that keeping the gas bubble in the right spot is important.
At Liv Hospital, we know how important patient education is. We teach you about the gas bubble and face-down positioning. This knowledge is essential for a successful recovery. We help you learn how to sleep after retinal detachment surgery for a smooth recovery.
Key Takeaways
- Maintaining a face-down position is key after retinal detachment surgery.
- The gas bubble in the eye is vital for healing.
- Good care after surgery is essential for recovery.
- Learning about post-surgery needs is important.
- Liv Hospital offers full support for international patients with retinal detachment surgery.
Understanding Retinal Detachment Surgery and Recovery

It’s important for patients to understand retinal detachment surgery and recovery. This surgery aims to fix the retina and prevent vision loss. It’s a complex process that helps restore vision.
What Happens During Retinal Detachment Surgery
The surgery involves removing the vitreous gel from the eye. This gel is replaced with a gas bubble. The gas helps hold the retina in place.
The surgeon chooses the gas based on the case. Air lasts 5 to 7 days, SF6 10 to 14 days, and C3F8 55 to 65 days. This gas bubble acts as a tamponade to help the retina heal.
The Initial Recovery Phase
The first part of recovery is key. Patients must keep their face down to keep the gas bubble in place. This helps the retina attach properly.
During this time, patients might feel discomfort and have blurry vision. It’s important to follow the doctor’s advice on posture, medication, and follow-up visits.
Setting Realistic Expectations
Having realistic expectations is important for recovery. Recovery takes time, and vision may improve slowly. Knowing that the gas bubble will disappear and recovery can take weeks or months is vital.
Patients should also be aware of possible complications. Following post-operative care instructions helps ensure a good outcome.
Gas Type | Absorption Rate |
Air | 5 to 7 days |
Sulfur Hexafluoride (SF6) | 10 to 14 days |
Perfluoropropane (C3F8) | 55 to 65 days |
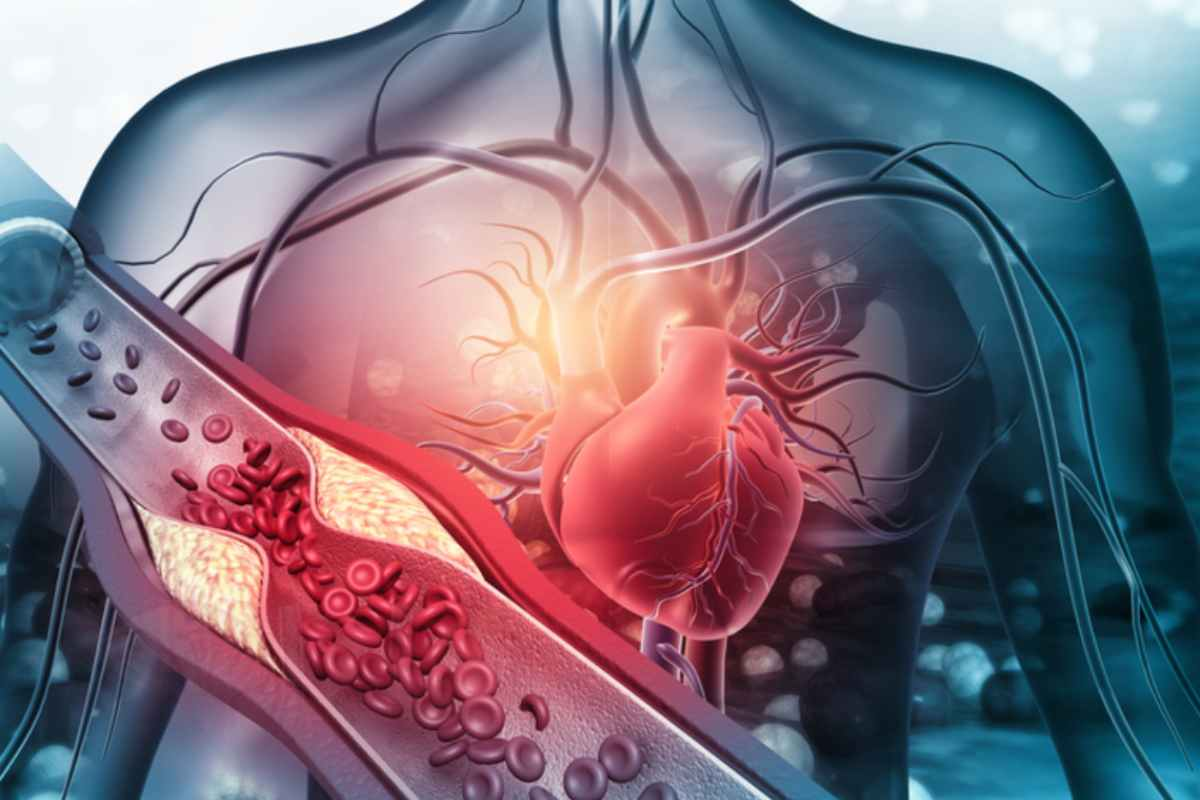
The Critical Role of Gas in Eyeball Following Retinal Surgery

Gas bubbles in retinal surgery have changed how we treat retinal detachment. This method has greatly improved results for patients. We’ll look at how gas bubbles help in healing and the different types used.
How Gas Bubbles Hold the Retina in Place
After surgery, a gas bubble is put in the eye’s vitreous space. This bubble acts as a temporary support, keeping the retina in place. It helps the retina reattach by sealing tears or holes.
Medical Expert, “The gas bubble acts as a temporary internal splint, allowing the retina to reattach and heal.”
“The introduction of intraocular gases has been a significant advancement in retinal detachment surgery, improving both the success rate and the postoperative management of patients.”
Different Types of Gas Bubbles and Their Absorption Rates
The gas used can affect how long it stays in the eye. Gases like sulfur hexafluoride (SF6), perfluoropropane (C3F8), and perfluoroethane (C2F6) are used. SF6 lasts about 2-3 weeks, while C3F8 can last 6-8 weeks.
Gas Type | Expansion Rate | Absorption Time |
Sulfur Hexafluoride (SF6) | 2 times | 2-3 weeks |
Perfluoropropane (C3F8) | 4 times | 6-8 weeks |
Perfluoroethane (C2F6) | 3 times | 4-6 weeks |
Studies show the gas choice depends on the patient’s needs. The body absorbs the gas bubble over time, making removal unnecessary.
Why Face-Down Positioning Is Essential After Surgery
Face-down positioning is key in the healing process after retinal detachment surgery. It’s not just a suggestion; it’s a must for the surgery to work right.
The Science Behind Positioning Requirements
A gas bubble is put in the eye during surgery to fix the retina. Face-down positioning helps the gas bubble stay in the right spot. This is vital for the retina to stick back together.
Keeping the face down helps the gas bubble stay where it needs to. This reduces the chance of problems and helps the healing go smoothly.
How Positioning Affects Gas Bubble Effectiveness
The gas bubble’s job is to keep the retina in place. When a patient is face-down, the bubble works best. It keeps the retina attached.
The Critical Scar Maturation Period (1-2 Weeks)
The first 1-2 weeks after surgery are very important. Face-down positioning is key during this time. It helps the retina stick back together and the scar to heal right.
Following the face-down rule during this time boosts recovery chances. It also lowers the need for more surgeries.
Required Positioning Duration Based on Detachment Location
The spot where the retinal detachment happens is key in figuring out how long a patient must stay face-down after surgery. This time can change a lot, depending on the detachment’s details.
Superior Retinal Breaks
Patients with superior retinal breaks usually need to stay face-down for 1 day. The gas bubble helps the superior retina because it floats up naturally. But, the exact time might change based on the patient and the doctor’s advice.
Inferior Retinal Breaks
For inferior retinal breaks, staying face-down is needed for 5 days or longer. The gas bubble must support the bottom retina, which is harder because it wants to float up. This longer time helps the retina heal and stick back together properly.
Factors That May Extend Positioning Requirements
Several things can make a patient need to stay face-down longer. These include:
- The size and complexity of the retinal detachment
- The presence of any complicating factors, such as vitreous hemorrhage
- The patient’s overall health and ability to comply with positioning instructions
It’s very important for patients to follow their surgeon’s exact instructions on how long to stay face-down. This can greatly affect the surgery’s success and the patient’s recovery.
Creating a Comfortable Face-Down Sleeping Environment
After retinal detachment surgery, sleeping face-down is key. A well-prepared sleeping area is vital for comfort and recovery. The right setup can make a big difference in how well you recover.
Essential Equipment for Face-Down Recovery
Several pieces of equipment help with face-down sleeping. These include:
- Face-Down Support Systems: These support the head and shoulders, making breathing easy and reducing face pressure.
- Three-Pad Faceplates: They offer extra support and can be adjusted for different sleeping positions, keeping the face aligned.
- Specialized Pillows: Designed for face-down sleep, these pillows help keep the neck and shoulders comfortable.
Arranging Your Bedroom for Maximum Comfort
The bedroom setup is also important for recovery. Here are some tips:
- Clear the Sleeping Area: Make sure the bed and around it are clutter-free for easy movement and safety.
- Adjust Lighting: Soft, dim lights create a calm sleep environment.
- Maintain a Comfortable Temperature: A cool, well-ventilated room is more comfortable during recovery.
Rental Equipment Options for Recovery
Renting specialized equipment can be convenient and cost-effective. Look into rental services that offer:
- Face-Down Positioning Devices: Great for those needing to stay in this position for a long time.
- Adjustable Hospital Beds: These beds adjust to various positions, providing comfort and flexibility during recovery.
Investing in the right equipment and adjusting your sleeping area can greatly improve comfort during recovery. Always talk to a healthcare provider to find the best options for your needs.
Step-by-Step Guide to Getting Quality Sleep While Face-Down
Sleeping after retinal detachment surgery needs careful positioning. Keeping your face down is key for surgery success. We’ll help you sleep well in this position.
Preparing for Bedtime After Retinal Surgery
Getting ready for bed is important after retinal surgery. Make your bedroom comfy for face-down sleep. You might need to move furniture or use special pillows.
Essential steps for bedtime preparation include:
- Ensuring your bed is at a comfortable height
- Having all necessary items within reach
- Creating a relaxing bedtime routine
Techniques for Falling Asleep in the Required Position
Falling asleep face-down can be hard. But, there are ways to make it easier. A face-down positioning device can help a lot.
Technique | Description | Benefit |
Relaxation Techniques | Deep breathing, progressive muscle relaxation | Reduces stress and promotes sleep |
Comfortable Positioning | Using supportive pillows or devices | Enhances comfort and maintains position |
Minimizing Distractions | Reducing noise, dimming lights | Creates a conducive sleep environment |
Managing Nighttime Bathroom Trips Safely
It’s important to handle nighttime bathroom trips safely. Try to drink less water before bed. Have a plan for safe bathroom visits.
Tips for safe nighttime bathroom trips:
- Move slowly and carefully to avoid slipping or falling
- Use a nightlight or flashlight to illuminate the path
- Consider having someone assist you if possible
By following these tips, you can sleep better while recovering from retinal detachment surgery.
Managing Pain and Discomfort for Better Sleep
Getting quality sleep is key for patients after retinal detachment surgery. A gas bubble in the eye can cause discomfort. The need to keep the face down adds to the physical strain.
Common Discomforts During Recovery
During recovery, patients face many discomforts. These include:
- Neck and back pain from staying face-down for long
- Eye discomfort or pain from the gas bubble
- General fatigue and irritability
Studies show that massages and ergonomic tools can help with neck and back pain. This is while staying face-down.
Medication Management for Sleep Improvement
Managing pain well is key for better sleep. Medication can help a lot. But, it’s important to take it as your doctor says to avoid bad side effects.
Medication Type | Purpose | Precautions |
Pain relievers | To manage pain | Follow dosage instructions carefully |
Sleep aids | To improve sleep quality | Use under doctor’s supervision |
Non-Medication Approaches to Pain Relief
There are ways to ease discomfort without medication. These include:
- Using ergonomic pillows and support devices
- Doing gentle stretching exercises as advised by healthcare providers
- Trying relaxation techniques like deep breathing or meditation
By using these methods, patients can manage their pain and discomfort better. This leads to better sleep during recovery.
Daytime Positioning and Rest Periods
After retinal detachment surgery, managing daytime positioning and rest is key. Patients must find a balance between staying in the face-down position and resting. This balance is important for a smooth recovery.
Balancing Face-Down Time Throughout the Day
It’s vital to mix face-down positioning with rest and daily activities. Taking breaks to rest while keeping the right position helps avoid fatigue. This approach supports overall well-being during recovery.
For example, patients can alternate between face-down time and breaks. It’s important to follow your doctor’s advice on how long and how often to stay in the face-down position.
Creating a Daytime Rest Schedule
Having a daytime rest schedule can help a lot. Planning your day ensures you rest enough and follow the positioning rules. Try dividing your day into parts for rest, positioning, and allowed activities.
Here’s an example of what your day could look like:
Time | Activity | Position |
9:00 AM – 10:00 AM | Breakfast and medication | Face-down |
10:00 AM – 12:00 PM | Rest | Face-down |
12:00 PM – 1:00 PM | Lunch | Face-down or sitting upright with caution |
1:00 PM – 3:00 PM | Quiet activities (reading, listening to music) | Face-down or slightly elevated |
Activities Compatible with Positioning Requirements
Even in the face-down position, you can do some things to make recovery easier. You can:
- Listen to audiobooks or podcasts
- Watch movies or TV shows on a tablet or laptop
- Play quiet games that don’t require holding a device
- Do gentle stretches or exercises approved by your healthcare provider
Choose activities that are comfortable and don’t hurt your positioning. Staying entertained and engaged can make recovery more enjoyable and less lonely.
Maintaining Mental Health During Restricted Positioning
After retinal detachment surgery, the face-down position can affect our mental health. It’s key to focus on our mental well-being during this tough time.
Coping with the Psychological Challenges
Recovery can bring feelings of isolation and frustration. To deal with these, we suggest:
- Staying in touch with loved ones through calls or video chats
- Enjoying passive activities that make us happy
- Trying relaxation methods like deep breathing or meditation
These steps can help manage the mental strain of recovery.
Entertainment Options While Face-Down
Keeping our minds engaged is important during recovery. Here are some fun ideas while staying face-down:
- Listening to audiobooks or podcasts
- Watching movies or TV shows on a tablet or smartphone
- Playing audio games or interactive stories
These activities can help take our minds off discomfort and make recovery easier.
Building a Support System for Recovery
A strong support network is vital for recovery. This can include:
- Family or friends helping with daily tasks
- Support groups for those going through similar experiences
- Professional counseling or therapy services
Having a wide support system ensures we get the care and encouragement we need during this time.
Potential Complications and When to Contact Your Doctor
Knowing the warning signs of complications during retinal surgery recovery is key. This helps you get medical help quickly. Even though retinal detachment surgery works well most of the time, knowing about possible problems is important for a good recovery.
Warning Signs During Recovery
Keep a close eye on your condition during recovery. Look out for these warning signs:
- Increased eye pain that can’t be managed with medicine
- Changes in vision, like more blurriness or light flashes
- New floaters or a sudden increase in them
- Redness or swelling in or around the eye
If you notice any of these, call your doctor right away.
Emergency Symptoms That Require Immediate Attention
Some symptoms need quick medical help to avoid serious issues. These include:
- Severe eye pain that’s too much to bear
- Sudden vision loss or a big drop in vision
- Increased sensitivity to light
- Pus or discharge from the eye
Tracking Your Recovery Progress
It’s important to keep track of how you’re recovering. We suggest keeping a log of your symptoms, medicine, and any worries. This helps your doctor see how you’re doing and adjust your treatment if needed.
Also, don’t miss your follow-up appointments with your doctor. These visits are key for checking on your recovery and catching any problems early.
Conclusion
Recovering from retinal detachment surgery needs careful attention, mainly with gas in the eyeball and face-down positioning. This time can be tough, but by following the advice in this article, patients can improve their recovery chances.
The gas in the eyeball is key in the early recovery stages. It helps keep the retina in place. It’s vital to follow the face-down positioning to make sure the gas bubble supports the retina well. Always listen to your surgeon’s advice, as it’s made just for you.
Rest, managing pain, and knowing about possible issues help patients get through recovery easier. We suggest staying informed and active during this time. Your help is important for a good outcome.
FAQ
What is the purpose of the gas bubble in the eye after retinal detachment surgery?
The gas bubble keeps the retina in place. This allows it to heal properly during recovery.
How long do I need to maintain face-down positioning after retinal detachment surgery?
The time needed varies. It can be as short as 1 day for some cases or up to 5 days for others.
What are the different types of gas bubbles used in retinal detachment surgery?
Various gas bubbles are used, each with its own absorption rate. The choice depends on the case and the surgeon’s preference.
How can I create a comfortable face-down sleeping environment?
Use a face-down positioning device and a comfy mattress. Adjust your bedroom to make sleeping easier.
What are some tips for getting quality sleep while maintaining the face-down position?
Prepare for bed well. Use techniques to fall asleep in the right position. Manage bathroom trips safely at night.
How can I manage pain and discomfort during recovery?
Use medication and non-medication methods for pain relief. Address common discomforts during recovery.
How do I balance face-down time throughout the day?
Make a daytime rest schedule. Do activities that fit the face-down position to balance rest and activity.
What are some ways to maintain mental health during restricted positioning?
Deal with psychological challenges. Find entertainment while face-down. Build a support system for mental health.
What are the warning signs that I should watch out for during recovery?
Watch for severe pain, increased light sensitivity, and vision changes. Track your recovery closely.
How long does it take for the gas bubble to be absorbed after retinal detachment surgery?
The gas bubble’s absorption rate varies by type. It usually takes weeks for it to be fully absorbed.
Can I engage in normal activities during the recovery period?
Some activities may be off-limits. Always follow your surgeon’s instructions for resuming normal activities.
How can I manage nighttime bathroom trips safely while maintaining the face-down position?
Use a bedside commode or adjust your sleeping setup to reduce movement. This helps with safe nighttime bathroom trips.
References
National Center for Biotechnology Information. Vitrectomy: Surgical Removal and Replacement of the Vitreous Humor. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10187786/