Last Updated on October 21, 2025 by mcelik
The medical and disease status criteria that disqualify a patient from receiving stem cells as a treatment are outlined here.
A stem cell transplant can save lives for some medical conditions. But not everyone can get it. At our place, we check each patient’s health to see if a transplant is right for them.

Things like being very old, having uncontrolled infections, or serious organ problems can stop someone from getting a bone marrow transplant. We look at how well a patient can handle treatment and if they have cancer.
Knowing what makes someone not fit for BM transplantation helps us find other ways to help them. This way, we can find the best treatment for each patient.
Stem cell transplantation is a complex medical procedure. It requires a deep understanding of its basics to see if a patient is eligible. We will look at the main parts of stem cell transplantation. This will help us understand who might not be a good fit for this treatment.
Stem cells are special cells that can turn into different types of cells. This makes them very useful for treating diseases. Stem cell therapy uses this ability to help with certain cancers and blood disorders. Stem cells can fix damaged tissues and bring back normal cell function.
Stem cells have opened new ways to treat diseases that were hard to manage before. Knowing how stem cells work and their uses in therapy helps us see the importance of stem cell transplantation in medicine.
There are two main types of stem cell transplants: autologous and allogeneic. Autologous uses the patient’s own stem cells. These are collected, stored, and then given back after treatment. This method lowers the risk of GVHD but might not always have enough healthy stem cells.
Allogeneic uses stem cells from a donor. This type can help fight cancer better, but has a higher risk of GVHD. It needs careful matching between the donor and the patient.
To qualify for a stem cell transplant, patients must meet certain criteria. They need to have a condition that can be treated with stem cell therapy. They also need to be in good physical shape and have healthy organs. The exact criteria depend on the type of transplant and the condition being treated.
Knowing these basics is key to figuring out if a patient is right for stem cell transplantation. By looking at the transplant type, the patient’s condition, and their health, doctors can decide the best treatment.
The role of advanced age in stem cell transplant eligibility has changed. Age used to be a big factor, but now it’s not as simple. Medical tech and understanding health beyond age have led to new criteria.
Before, age 65 was often a limit for transplants. But this was seen as too simple. It didn’t consider how healthy someone could be at any age.
“Chronological age is just a number,” experts say. “What really matters is the patient’s health and how well they function.” This shows a move towards a more detailed look at who can get a transplant.
It’s important to know the difference between physiological and chronological age. Chronological age is how old you are in years. Physiological age is about your health and how well you function. This helps us decide if someone can get a transplant based on their real health.
Some people over 65 are healthier than others who are younger. So, we look at more than just age. We check how well someone functions, their health problems, and their mind.
Reduced-intensity conditioning (RIC) has made transplants possible for older patients. RIC is less harsh than old methods. It lowers the risk of serious problems and death during the transplant.
RIC lets us transplant more patients, including older ones. This is good news for those with blood cancers and other diseases that can be treated with transplants.
Key considerations for older patients include their health, any health problems, and how well they can function. Looking at the whole picture helps us decide who will benefit from a transplant.
Systemic infections that are not controlled are a big problem for stem cell transplants. These infections can make the transplant harder and raise the chance of problems after the transplant.
Bacterial infections are a big worry for those getting stem cell transplants. Active bacterial infections need to be fixed before transplant to lower the risk of serious issues. We check how bad these infections are with cultures and tests.
Viral infections are also key in deciding if someone can get a transplant. Some viruses can come back after a transplant because of weakened immunity. We watch viral loads closely and use antiviral drugs to stop them from coming back.
Fungal infections are also very important. Invasive fungal infections can be deadly for those with weak immune systems. We work hard to find and treat fungal infections before transplant.
By managing and treating systemic infections well, we can lower the risks of stem cell transplant. This helps improve how well patients do after transplant.
Cardiac dysfunction is a key factor in deciding if someone can get a stem cell transplant. The heart’s health is very important for a patient’s overall well-being. It affects how well they can handle the transplant process.
The left ventricular ejection fraction (LVEF) shows how well the heart pumps blood. A low LVEF means a patient might face more risks during the transplant. “A reduced LVEF is associated with increased morbidity and mortality in patients undergoing stem cell transplantation,” say heart specialists.
Usually, an LVEF of 50% or more is needed for transplant eligibility. But, this can change based on the transplant center and the patient’s health.
A detailed cardiac check is vital before a transplant. It helps figure out if someone can get a stem cell transplant. Tests like echocardiography and stress tests are part of this check.
It’s important to do a thorough cardiac check to spot risks early. “A detailed cardiac evaluation is key to reducing risks with stem cell transplantation,” says a top cardiologist.
Heart failure is graded by how severe it is. Patients with severe heart failure (NYHA Class III or IV) might not be eligible for a transplant. This is because they face a higher risk of problems.
Arrhythmias and structural heart diseases are big worries for stem cell transplants. Patients with these issues might be at higher risk during the transplant.
We look closely at these conditions to see if someone is right for stem cell therapy. “Managing arrhythmias and structural heart disease is key for successful stem cell transplantation,” say recent guidelines.
Pulmonary function is key in deciding if a patient can get stem cell transplantation. Good lung health is needed to handle the treatment and transplant.
We use pulmonary function tests (PFTs) to check lung capacity and health. These tests look at DLCO (Diffusing Capacity of the Lung for Carbon Monoxide) and FEV1 (Forced Expiratory Volume in 1 second). These are important for seeing if a patient can get a stem cell transplant.
DLCO shows how well the lungs move gases. FEV1 measures air exhaled in one second. Both are key to see if a patient can handle the transplant.
There are certain DLCO and FEV1 levels to follow. A DLCO ≥ 60% and an FEV1 ≥ 60% of the predicted value are okay for transplant. Values less than these might mean a greater risk of lung problems after transplant.
“Pulmonary function tests are vital in assessing the risk of pulmonary complications after stem cell transplantation.”
Chronic obstructive pulmonary disease (COPD) is a big worry for transplant. Severe COPD can make transplant risks higher. We look at COPD’s impact on health before deciding on a transplant.
Pulmonary hypertension also affects transplant suitability. High blood pressure in the lungs can cause serious problems. We check how bad pulmonary hypertension is before transplant.
In short, lung function is very important for a stem cell transplant. We do detailed checks, including PFTs, to make sure patients are ready for transplant.
Significant liver dysfunction can stop stem cell transplantation. The liver is key for recovery after such a procedure. Any liver condition can make the transplant harder.
Before a stem cell transplant, patients get a detailed liver check. Tests like liver enzyme levels and bilirubin levels are used. Imaging studies like ultrasound or CT scans are also done.
Liver enzyme levels show liver damage or dysfunction. High levels mean the liver is stressed or sick. This might make a patient not eligible for a transplant.
Cirrhosis and advanced liver disease are big worries for transplant patients. Cirrhosis causes liver scarring and can lead to failure. Advanced liver disease makes the transplant riskier.
We carefully check patients with cirrhosis or advanced disease. We look at how severe their condition is and the transplant risks.
Hepatitis status is key to transplant eligibility. Active hepatitis means a liver infection that might get worse with the transplant.
We check hepatitis status with viral load tests and liver function tests. This helps us understand the transplant risks.
Veno-occlusive disease (VOD) is a serious risk after stem cell transplant. It blocks small hepatic veins, causing liver problems.
We check VOD risk by looking at liver function, medical history, and other factors. This is important for deciding if a patient can have a stem cell transplant.
When deciding if a patient can get a stem cell transplant, their kidney health is key. Kidney problems can make it hard for a patient to get a transplant. We use tests to check how well the kidneys are working to see if there are risks.
We look at creatinine clearance and Glomerular Filtration Rate (GFR) to check the kidneys. A certain GFR level is needed for transplant eligibility. Those with a GFR below this level might face more risks.
A GFR under 60 mL/min/1.73 m shows serious kidney trouble. We check these levels to see if a patient can get a stem cell transplant.
Dialysis patients are a special case. Dialysis helps with kidney failure, but it doesn’t mean they can’t get a transplant. But deciding on a transplant for dialysis patients needs careful thought.
We look at each case closely. We consider why the kidneys failed and the patient’s health.
Managing kidney disease well is important before a transplant. This might mean adjusting medicines, managing fluids, and treating other health issues.
By improving kidney health, we can lower the chance of transplant problems.
Patients with kidney problems might need to change their medicines. Some drugs could harm the kidneys or cause bad reactions.
We help patients adjust their medicines to fit their kidney health. This ensures they are safe and well-managed.
Checking a patient’s performance status is key to seeing if they can get a stem cell transplant. Performance status shows how well a patient can perform daily tasks.
“A patient’s performance status is a strong predictor of their outcome after stem cell transplantation,” as emphasized by various clinical studies. We use standardized scales to evaluate this status.
The ECOG (Eastern Cooperative Oncology Group) performance status and Karnofsky Performance Status (KPS) are two common scales. The ECOG scale goes from 0 (fully active) to 5 (dead). The KPS scale goes from 100 (normal) to 0 (dead).
Usually, a KPS score of 70 or higher and an ECOG score of 2 or less are okay for transplant.
Being able to do daily tasks is key for stem cell transplant patients. Those who can do more tasks tend to do better. We check how well a patient can do things on their own.
Frailty means a person’s body can’t handle stress well. We check for frailty to see who might face more risks after transplant. The Fried Frailty Index is one tool we use.
A patient’s nutrition is also very important. Being malnourished can make transplant risks higher. We look at things like serum albumin and BMI to check nutrition.
In short, checking a patient’s performance status, including their ability to do tasks, frailty, and nutrition, is key to deciding if they can get a stem cell transplant.
Stem cell transplantation for patients with current or recent cancers is a big decision. It involves looking at several important factors.
One major worry is the chance of getting a second cancer. We look at the first cancer, its treatment, and the risk of it coming back or a new one appearing after the transplant.
Risk factors for a second cancer include past treatments like chemotherapy or radiation. Also, genetic risks and precancerous lesions play a part.
Disease-free intervals are key when deciding if a patient with a cancer history can get a stem cell transplant. The length of this interval depends on the cancer type and how aggressive it is.
For example, those with aggressive cancers might need a longer wait than those with less aggressive ones.
There are specific waiting times for different cancers to make sure they are in remission. These periods help lower the risk of the cancer coming back.
For patients with more than one cancer, a detailed risk-benefit analysis is needed. This means looking at the transplant’s risks against its possible benefits.
We consider the patient’s health, the status of their current cancer, and how much the transplant could help. This helps us decide if stem cell transplantation is right for them.
By carefully looking at these factors, we can make informed choices about stem cell transplantation for patients with current or recent cancers.
Checking if someone is a good candidate for a stem cell transplant is key. At our place, we look closely at each patient to see if a transplant is right for them.
When we check if someone can get a transplant, we look at many things. This includes their age, how well their organs work, how they feel, and if they have other cancers. Knowing what makes someone not a good candidate helps both patients and doctors make smart choices.
Our team works hard to find the best treatment for each patient. We check their health and look for any risks a transplant might bring.
By carefully checking who can get a transplant, we make sure patients get the best care. This way, we can give each patient the support and care they need during the transplant process.
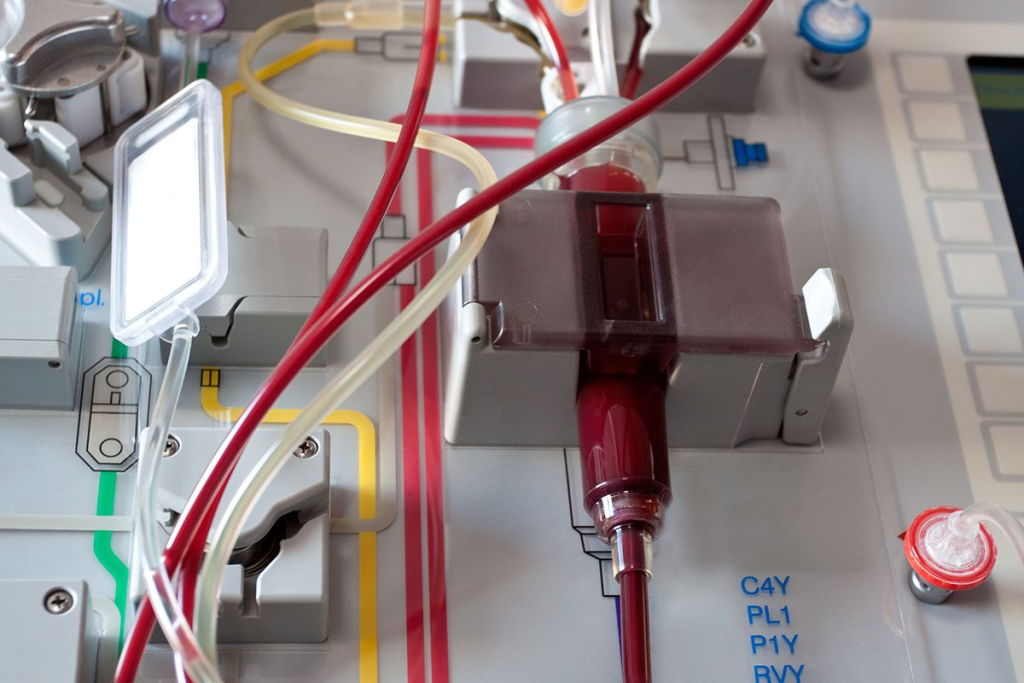
A stem cell transplant is a complex procedure. It replaces damaged or diseased stem cells with healthy ones. These can come from the patient themselves or a donor.
There are two main types. Autologous uses the patient’s own stem cells. Allogeneic uses stem cells from a donor.
Advanced age used to limit stem cell transplants. Now, it’s the patient’s physiological age that matters more than their chronological age.
Uncontrolled infections can make a transplant risky. It’s key to treat infections before transplant to avoid complications.
Heart function is critical. Poor heart function can raise transplant risks. A detailed heart check is needed before a transplant.
Poor lung function can increase transplant risks. Conditions like COPD and pulmonary hypertension can affect eligibility.
Liver problems, like cirrhosis, can be risky for transplant. A thorough liver check is essential for eligibility.
Renal problems can raise transplant risks. Patients with kidney disease need special care before a transplant.
A patient’s performance status is key. Poor scores on scales like ECOG and Karnofsky can indicate high transplant risks.
Current or recent cancers can affect transplant eligibility. A detailed risk assessment is needed.
Hematopoietic stem cell transplantation replaces blood cells. It’s a type of stem cell transplant.
An autologous transplant uses the patient’s own stem cells. This reduces the risk of graft-versus-host disease.
Stem cell therapy uses stem cells to treat conditions. In transplantation, it replaces damaged cells with healthy ones.
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!
WhatsApp us