Spotting flare in the anterior chamber is key for diagnosing and treating eye inflammation. We use advanced tests to find and measure inflammation in the eye’s fluid flare in anterior chamber of eye.
When we look closely with a slit lamp, anterior chamber flare shows up as a haze or light. This is because there’s more protein in the fluid. It’s a sign of inflammation inside the eye, like anterior uveitis.
New studies show tools like laser flare photometry and optical coherence tomography help measure aqueous flare and cells. These tools help us give precise diagnoses and treatment plans.
Key Takeaways
- Anterior chamber flare is a critical diagnostic indicator for ocular inflammation.
- Advanced diagnostic techniques enable objective measurements of inflammatory markers.
- Laser flare photometry and anterior segment optical coherence tomography are key diagnostic tools.
- Accurate diagnosis is key for effective management of intraocular inflammation.
- Recognizing flare in the anterior chamber is essential for preventing vision-threatening complications.
Understanding Anterior Chamber Flare
For ophthalmologists, grasping the details of anterior chamber flare is key to top-notch patient care. Flare in the anterior chamber shows the breakdown of the blood-aqueous barrier. This leads to proteins leaking into the aqueous humor.
Definition and Pathophysiology
Anterior chamber flare is seen as protein exudates in the aqueous humor. It’s spotted with slit-lamp biomicroscopy. The breakdown of the blood-aqueous barrier causes this, letting proteins and big molecules into the chamber. This can happen from inflammation, trauma, or surgery.
The blood-aqueous barrier keeps the aqueous humor clear. When it fails, proteins and other stuff leak out. Knowing why this happens helps doctors diagnose and treat flare in the anterior chamber.
Clinical Significance in Ophthalmology
Flare in the anterior chamber is important because it shows up in many eye problems, like uveitis. It shows how bad the inflammation is. Spotting and measuring flare helps doctors decide on treatment and check if it’s working.
Doctors look at flare and cells in the chamber together. This gives a full picture of the eye’s inflammation. It’s vital for planning treatment and tracking how the disease is doing.
The Anatomy of the Anterior Chamber
Understanding the anatomy of the anterior chamber is key for eye doctors. It’s filled with aqueous humor, a clear fluid made by the ciliary body.
Normal Structure and Function
The anterior chamber is surrounded by the cornea in front and the iris and lens in back. It helps keep the eye’s pressure right and feeds nutrients to the cornea and lens. The aqueous humor is vital, supplying nutrients and removing waste.
The ciliary body makes aqueous humor. It flows through the pupil into the chamber. Then, it’s drained through the trabecular meshwork into Schlemm’s canal.
Blood-Aqueous Barrier Integrity
The blood-aqueous barrier keeps the anterior chamber safe. It controls what gets from the blood into the aqueous humor. This barrier stops harmful substances from entering the eye.
Keeping the blood-aqueous barrier strong is important. It keeps the aqueous humor clear and the anterior chamber healthy. If it breaks down, problems like flare can happen. This is when proteins leak into the chamber.
Pathophysiology of Flare in Anterior Chamber of Eye
Exploring the cause of flare in the anterior chamber shows us how complex the eye’s inner workings are. Flare is a sign that something is off in the eye’s normal function.
Protein Leakage Mechanisms
When the blood-aqueous barrier breaks down, proteins leak into the aqueous humor, causing flare. This leakage is key because it affects the clarity of the aqueous humor and our vision.
Protein leakage happens because the blood vessels in the eye become more open. This openness lets proteins and other substances move into the aqueous humor, leading to flare.
Blood-Aqueous Barrier Disruption
The blood-aqueous barrier is vital for keeping the eye’s internal environment stable. When this barrier is damaged, proteins and other molecules leak into the aqueous humor.
This damage can be caused by inflammatory conditions and traumatic injuries. Knowing what causes it helps us manage flare better.
Inflammatory Mediators
Inflammatory mediators are key players in flare’s pathophysiology. They make the blood vessels in the eye more open, leading to protein leakage and flare.
The release of inflammatory mediators is a response to injury or disease in the eye. Controlling this response is important for reducing flare and getting the eye back to normal.
Common Causes of Anterior Chamber Flare
Knowing what causes anterior chamber flare is key to treating it. There are many reasons why flare happens in the front part of the eye. We’ll look at each one closely.
Inflammatory Conditions
Inflammatory conditions are a big reason for flare in the anterior chamber. Anterior uveitis is a common eye inflammation. It can break down the blood-aqueous barrier, causing flare.
Other conditions that can lead to flare include:
- Behçet’s disease
- Sarcoidosis
- Ankylosing spondylitis
These conditions need a detailed diagnosis to manage well.
Traumatic Causes
Eye trauma is another major reason for flare. Both blunt and penetrating injuries can damage the eye, causing inflammation and flare.
The flare’s severity depends on the injury’s extent. Post-traumatic uveitis is a common issue that can cause a lot of flare.
Type of Trauma | Common Outcomes |
Blunt Trauma | Hyphema, angle recession, uveitis |
Penetrating Trauma | Endophthalmitis, uveitis, retinal detachment |
Iatrogenic Factors
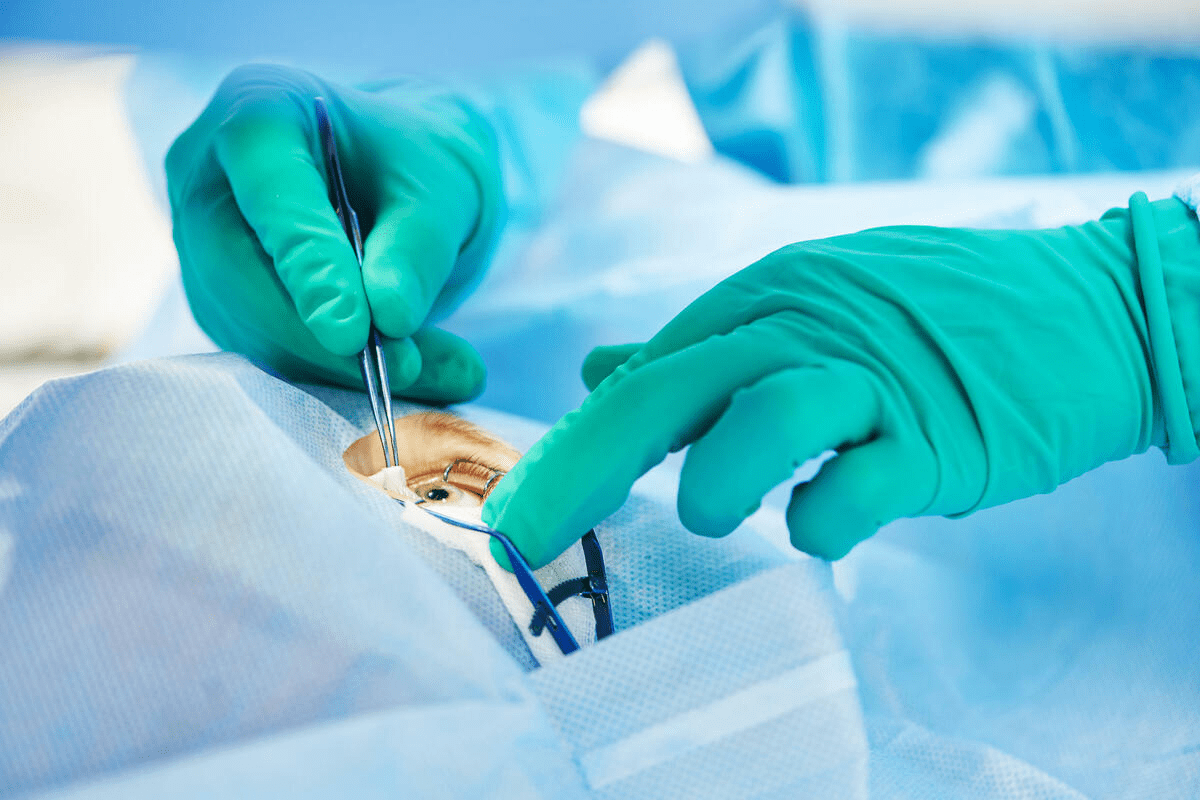
Medical procedures can also cause flare. For example, cataract surgery can lead to inflammation after the operation.
It’s important to watch patients closely after surgery to manage flare well.
Understanding the causes of anterior chamber flare helps us create better treatment plans. This way, we can tackle the root cause and lower the chance of more problems.
Clinical Presentation and Associated Findings
The symptoms of flare in the anterior chamber are key for diagnosis. Ophthalmologists need to spot these signs to manage related conditions well.
Patient Symptoms
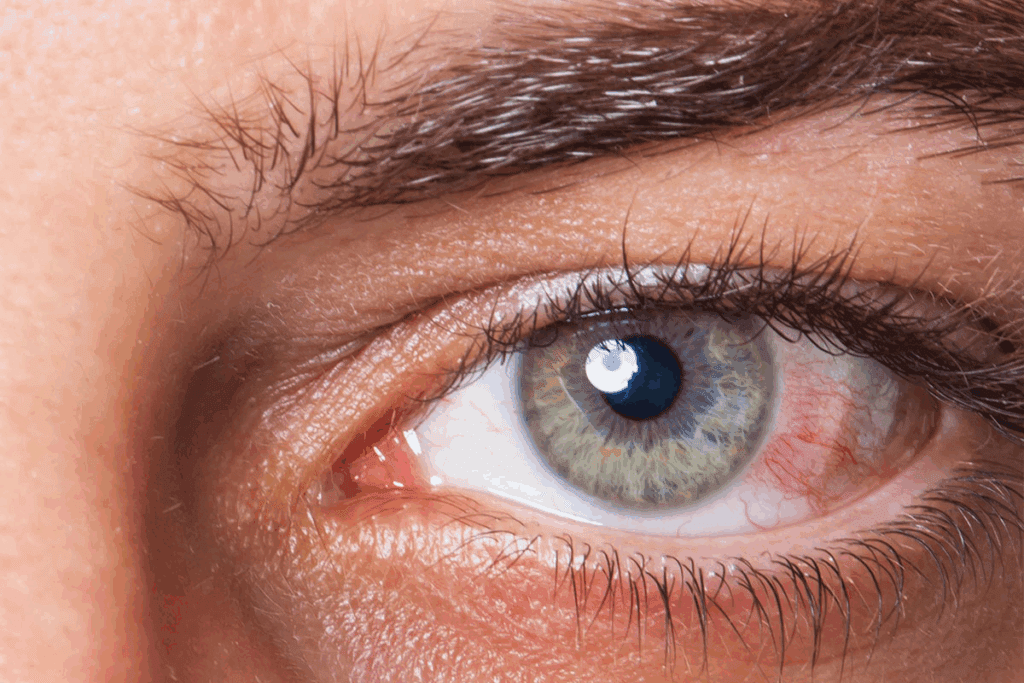
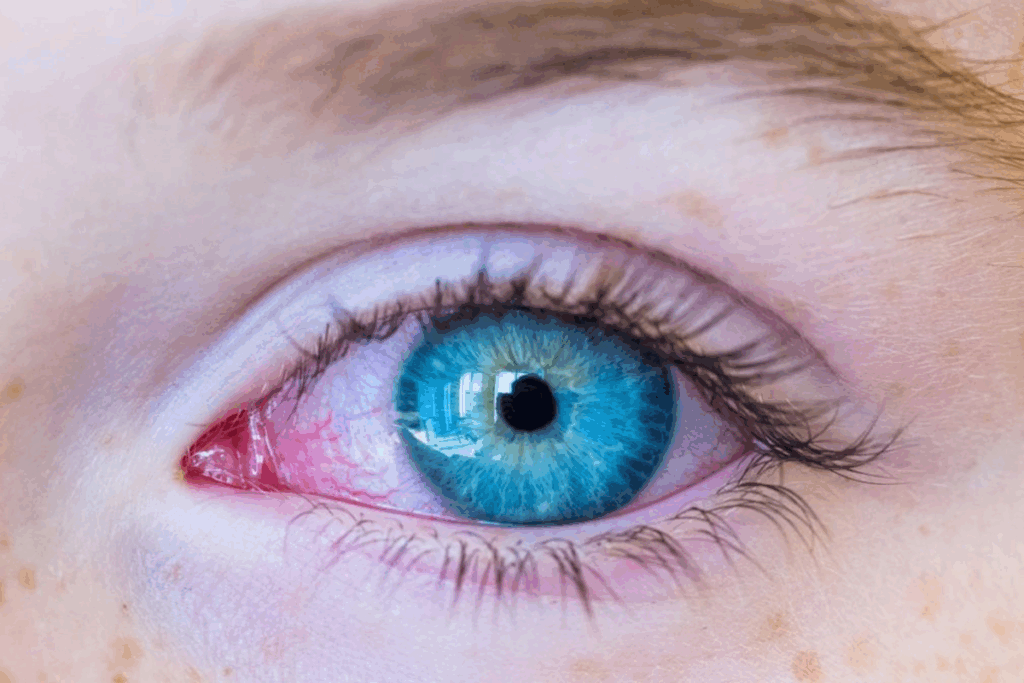
People with flare in the anterior chamber often feel pain, redness, and sensitivity to light. These signs show the inflammation at work.
They might also feel uncomfortable and light-sensitive. These feelings can really affect their daily life. We must think about these symptoms when we look at flare’s signs.
Visual Manifestations
Flare in the anterior chamber can make vision worse and blurrier. This happens because the inflammation affects the eye’s front part.
Table: Common Visual Manifestations
Manifestation | Description |
Decreased Vision | Reduction in visual acuity due to inflammation |
Blurred Vision | Loss of sharpness and clarity in vision |
Floaters | Perception of small spots or particles floating in the visual field |
Associated Clinical Signs
Signs like cells and flare seen on slit-lamp exams are key for diagnosing flare. These signs help us track the condition.
Other signs include red conjunctiva, swollen cornea, and iris changes. We need to look at these signs closely. This helps us understand how much inflammation is in the eye.
By knowing the signs of flare in the anterior chamber, we can give the right diagnosis. Then, we can make a good treatment plan for our patients.
Equipment Required for Detecting Flare
Ophthalmologists use special tools to find flare. The main tool is slit lamp biomicroscopy. It helps check the front part of the eye for signs of inflammation.
Slit Lamp Biomicroscopy Setup
The slit lamp is key in eye exams. It’s used to look at the front part of the eye. Setting it up right is key for spotting flare:
- Adjust the slit lamp to provide a narrow beam of light.
- Ensure the beam is focused on the anterior chamber.
- Use appropriate magnification to visualize flare.
A top ophthalmology journal says, “The slit lamp biomicroscope is the best for eye exams.”
This shows how important using the slit lamp right is for finding flare.
Optimal Room Conditions
Good room conditions help spot flare better:
- Dim the room lights to reduce background illumination.
- Maintain a stable temperature to minimize patient discomfort.
Controlled environmental conditions help see better with the slit lamp.
Additional Diagnostic Tools
While the slit lamp is main, other tools help measure flare:
- Laser flare photometry for objective measurement.
- Anterior segment optical coherence tomography (OCT) for detailed imaging.
These tools add to what the slit lamp shows. They give a full view of inflammation in the front chamber.
Step-by-Step Technique for Identifying Flare
To accurately diagnose flare in the anterior chamber, we use slit lamp biomicroscopy. We’ll show you how to do it right.
Patient Positioning and Preparation
Getting the patient in the right position is key. We adjust the chin rest and forehead support for comfort and stability. The patient’s eyes should be level with ours.
Clear instructions are given to get the position just right. Experts say it’s essential for a good exam.
Slit Lamp Settings and Adjustments
To spot flare, we fine-tune the slit lamp settings. We start with a narrow slit, about 1 mm wide, to see particles better. Adjusting the slit beam’s height is also important to avoid light scatter.
The light’s intensity is set based on the patient’s eye color and flare severity. We begin with a medium setting and tweak as needed. The angle between the light and view arms is set at 45 to 60 degrees for flare detection.
Examination Methods
With the slit lamp ready, we start the exam. The patient looks straight ahead and then slightly to the side. We focus the beam on the anterior chamber to look for flare.
Slow and gentle movements help us see how much flare there is. We compare the beam’s clarity in the chamber to the rest of the area. Using scales like the SUN Working Group’s helps track flare severity over time.
- Use a systematic approach to examine all areas of the anterior chamber.
- Compare findings with previous examinations to assess progression or improvement.
- Document the findings thoroughly in the patient’s record.
Relationship Between Flare and Cells in the Anterior Chamber
It’s important to understand how flare and cells work together in the anterior chamber. Both are signs of inflammation in this area.
Differentiating Cells from Flare
Cells and flare are different but connected. Cells are white blood cells and other inflammatory cells. Flare is when proteins leak into the aqueous humor, making it hazy.
Telling cells apart from flare is key for a correct diagnosis. Cells are counted one by one with a slit lamp. Flare is judged by how hazy the chamber is.
Clinical Significance of Combined Findings
Seeing both cells and flare means there’s active inflammation. This is important for diagnosing and treating uveitis and other inflammatory eye diseases.
The importance of these signs can be seen in several areas:
- Accurate diagnosis
- Assessing how severe it is
- Tracking how well treatment is working
- Understanding what the future might hold
Quantitative Assessment Methods
Measuring flare and cells is key for tracking disease and treatment. Laser flare photometry is a precise way to measure flare. It gives a clear measure of inflammation.
Method | Description | Advantages |
Slit Lamp Examination | Visual check of cells and flare | Easy to get, fast |
Laser Flare Photometry | Measures flare precisely | Very accurate, objective |
Anterior Segment OCT | Clear images of the chamber | High detail, all-encompassing |
Using these methods together helps doctors fully understand inflammation in the anterior chamber. This leads to better care for uveitis and similar conditions.
Standardized Grading Systems for Anterior Chamber Flare
To ensure consistency in diagnosing and managing uveitis, standardized grading systems for anterior chamber flare are essential. These systems help clinicians communicate effectively and make informed decisions for patient care.
SUN Working Group Classification
The Standardization of Uveitis Nomenclature (SUN) Working Group classification is widely accepted. It grades anterior chamber flare based on its severity. This allows for a standardized approach to documentation and clinical assessment.
Key components of the SUN Working Group classification include:
- Grade 0: No flare
- Grade 1+: Faint flare
- Grade 2+: Moderate flare
- Grade 3+: Marked flare
- Grade 4+: Intense flare
Documentation Best Practices
Accurate documentation of anterior chamber flare is critical. It helps monitor disease progression and treatment response. We recommend using a standardized template that includes the flare grade and other relevant clinical findings.
Best practices for documentation include:
- Using the SUN Working Group classification for grading flare
- Recording the grade in the patient’s medical record
- Including photographs or diagrams when possible
- Documenting any changes in flare grade over time
Clinical Application of Grading
The clinical application of flare grading goes beyond documentation. It informs treatment decisions, monitors disease activity, and provides prognostic information.
The clinical utility of flare grading includes:
- Guiding the intensity of anti-inflammatory therapy
- Monitoring response to treatment
- Identifying possible complications early
- Facilitating communication among healthcare providers
By adopting standardized grading systems for anterior chamber flare, we can improve patient care. This also advances our understanding of uveitis and other inflammatory conditions.
Advanced Technologies for Objective Flare Measurement
New technologies are changing how we check flare in the eye’s front part. Tools like laser flare photometry and anterior segment optical coherence tomography (OCT) make flare checks more accurate. This helps doctors make better diagnoses and care for patients.
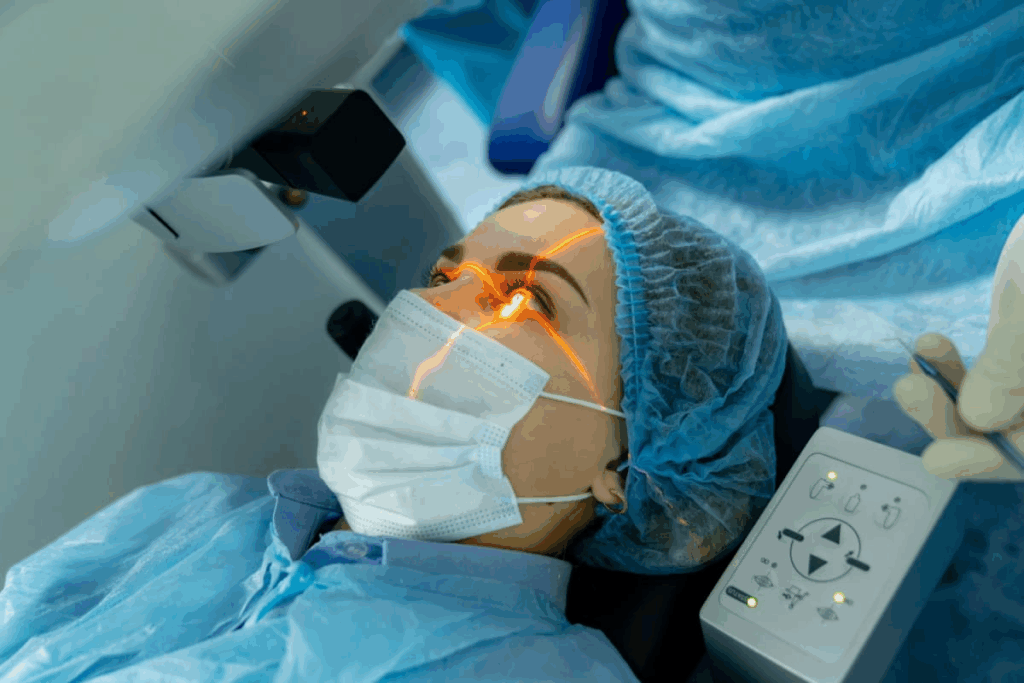
Laser Flare Photometry Principles
Laser flare photometry is a precise way to find and measure protein leaks in the eye’s front. It uses a laser to see how much light is scattered by proteins in the eye’s fluid. This shows how much flare there is.
This method is very sensitive. It can spot small changes in flare that doctors might miss. It’s great for tracking how well treatments are working and catching flare-ups early.
Anterior Segment Optical Coherence Tomography
Anterior segment OCT gives detailed pictures of the eye’s front part. It’s mainly for looking at structures, but it can also hint at flare levels.
Newer OCT models are getting better at showing details faster. This means doctors can see more clearly and make better connections with what they see and feel.
Correlation with Clinical Grading
Research shows that laser flare photometry and OCT match up well with doctor’s flare grades. But these tools are more precise and can catch small changes.
Technology | Correlation with Clinical Grading | Advantages |
Laser Flare Photometry | High correlation | Objective measurement, high sensitivity |
Anterior Segment OCT | Moderate to high correlation | Detailed structural assessment, non-invasive |
Emerging Diagnostic Modalities
New tech is coming that might make flare checks even better. Things like advanced OCT angiography and new imaging ways are on the horizon.
Using these new tools could really help doctors do their jobs better. It could lead to better care for eye patients.
Clinical Correlation and Disease Management
It’s key to understand the link between flare in the anterior chamber and disease management. The level of flare helps decide treatment and predict disease outcomes. We’ll look at how flare affects diagnosis, treatment, and monitoring.
Diagnostic Implications
Seeing flare in the anterior chamber means inflammation or disease is present. Accurate diagnosis is vital to find the flare’s cause. This could be uveitis, trauma, or other issues. Clinicians use this info to choose the right tests and treatments.
Treatment Decision-Making
The flare’s severity plays a big role in treatment choices. A high flare level might need stronger anti-inflammatory drugs. But, a drop in flare shows treatment is working, guiding further adjustments.
Monitoring Disease Progression
Keeping an eye on flare is key in managing diseases. Regular checks help see if treatment is working. This is important to avoid complications and get the best results for patients.
Prognostic Significance
Flare’s impact on disease outcome is huge. Its presence and intensity at diagnosis and follow-ups offer insights. Patients with severe flare might need closer monitoring and stronger treatments to prevent complications.
In summary, grasping the clinical correlation of flare is vital for managing diseases. It helps in diagnosis, treatment, monitoring, and predicting disease outcomes. This way, doctors can give better care to patients with uveitis and similar conditions.
Conclusion
It’s important to spot flare in the anterior chamber for good uveitis care. We’ve looked at what flare is, how it works, and why it matters. We’ve also talked about how to find and measure it.
Checking for flare helps doctors decide on the best treatment and what to expect. Knowing how flare and cells in the chamber relate helps doctors take better care of patients.
Flare shows inflammation, and finding it right is key for treating uveitis. Using standard ways to measure and new tech like laser flare photometry makes flare checks more reliable.
In short, knowing about flare in the anterior chamber is key for managing uveitis well. By using what we’ve learned, doctors can give better care and help patients more.
FAQ
What is flare in the anterior chamber of the eye?
Flare in the anterior chamber is a haze or light reflection. It happens when there’s more protein in the aqueous humor. This usually occurs when the blood-aqueous barrier is disrupted.
What causes flare in the anterior chamber?
Flare can be caused by inflammation, like uveitis. It can also happen due to injuries or after surgery.
How is flare in the anterior chamber diagnosed?
Doctors use a slit lamp to diagnose flare. They also use laser flare photometry to measure its severity.
What is the clinical significance of flare in ophthalmology?
Flare is important for diagnosing and managing uveitis. It helps doctors track the disease’s progress and how well treatments are working.
How is flare differentiated from cells in the anterior chamber?
Flare is about protein leakage, while cells are inflammatory cells. Doctors can tell them apart by looking at them under a slit lamp.
What is the SUN Working Group classification for grading flare?
The SUN Working Group has a system for grading flare. It helps doctors document and decide on treatments consistently.
What advanced technologies are used for measuring flare?
Laser flare photometry and optical coherence tomography are used. They help measure flare objectively and accurately.
How does flare assessment influence treatment decisions?
The severity of flare guides treatment choices. It determines if anti-inflammatory therapy is needed and how intense it should be.
Can flare be used as a prognostic indicator?
Yes, flare’s presence and severity can predict uveitis’s course. It can also indicate the risk of complications.
What are the implications of aqueous flare in uveitis management?
Aqueous flare is a key sign of inflammation in uveitis. Managing it is vital for controlling the disease and avoiding complications.
How is flare related to the blood-aqueous barrier?
Flare happens when the blood-aqueous barrier is broken. This allows proteins to leak into the aqueous humor.
What role does slit lamp biomicroscopy play in detecting flare?
Slit lamp biomicroscopy is key for spotting flare. It lets doctors see the aqueous humor and check for protein leakage.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/32255392/