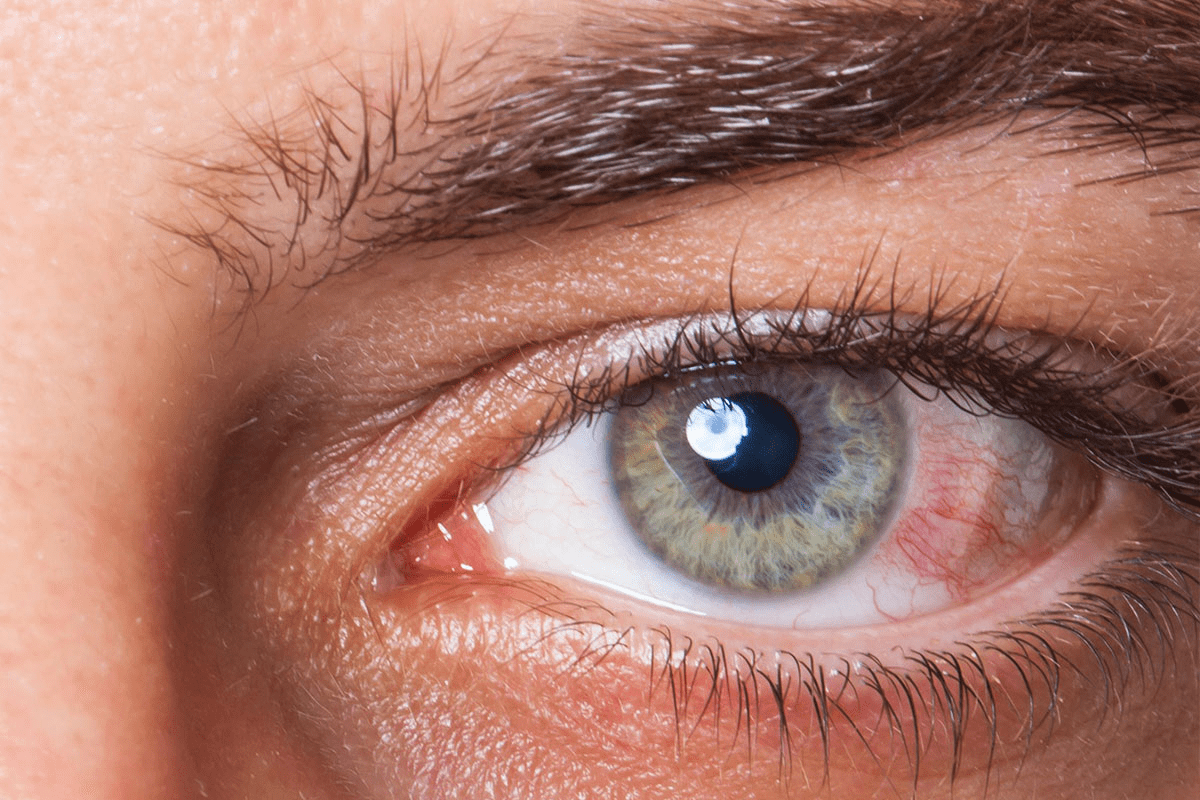
Double vision, or diplopia, is a common issue after a stroke. It affects about 60 percent of stroke patients. The American Academy of Ophthalmology says it happens when nerves controlling eye movement get damaged. This makes the eye muscles work wrong. Suffering from diplopia after stroke? This ultimate recovery guide explains why it happens, the best treatments, and if it will go away.
Seeing double can be scary and really affect your daily life. But, the good news is that many stroke survivors can get better. They do this through early diagnosis and a good rehabilitation plan.
Key Takeaways
- Double vision is a common complication after a stroke, affecting a significant percentage of patients.
- The condition occurs due to damage to the nerves controlling eye movement.
- Timely diagnosis and a good rehabilitation plan can lead to big improvements.
- Recovery varies greatly from person to person.
- Evidence-based treatment strategies are key for managing double vision.
What Happens to Vision After a Stroke
Many people see changes in their vision after a stroke. This can really affect their daily life. Almost two-thirds of those who survive a stroke face vision problems. These can be mild or very severe.
Strokes can cause many side effects, including vision issues. These problems can slow down a person’s recovery and lower their quality of life.
Common Visual Disturbances Following Stroke
Visual problems after a stroke vary from person to person. Some common issues are blurred vision, losing part of their field of vision, and being too sensitive to light. We will look at these problems in more detail.
Visual Disturbance | Description | Impact on Daily Life |
Blurred Vision | Lack of clarity in vision, making objects appear fuzzy. | Difficulty reading, watching TV, or recognizing faces. |
Loss of Peripheral Vision | Reduced ability to see objects or movement outside of direct line of sight. | Increased risk of accidents, difficulty navigating spaces. |
Sensitivity to Light | Increased sensitivity to light, potentially causing discomfort or pain. | Avoidance of bright environments, use of sunglasses indoors. |
The Specific Challenge of Double Vision
Double vision, or diplopia, is a big challenge. It happens when the eyes can’t line up right. This makes people see two images instead of one. It can be constant or come and go, depending on the cause.
Recovery times vary. Some people see improvements quickly, while others face long-term vision issues. Knowing the cause of visual problems is key to finding the right treatment.
Understanding Diplopia After Stroke

Double vision, or diplopia, is a common problem after a stroke. It can make everyday tasks hard. A stroke can mess with how the brain controls eye movements, causing this issue.
Definition and Mechanisms
Diplopia happens when nerves controlling eye movement get damaged. This makes the eye muscles work wrong, leading to seeing two images instead of one. Eye misalignment can be caused by muscle weakness or paralysis.
A 2019 study found that many visual problems after a stroke don’t go away. But, early and frequent vision therapy can help some people recover.
How Stroke Damages Eye Movement Control
A stroke can harm the brain parts that control eye movement. This includes the cranial nerve nuclei or their connections. This damage messes up the extraocular muscles, causing diplopia.
The impact on eye movement control varies with the stroke’s location and severity. For example, damage to the abducens nerve can make it hard to move the eye outward. Damage to the oculomotor nerve can affect eye movement in multiple directions.
Types of Double Vision Following Stroke
There are different kinds of double vision after a stroke, including:
- Horizontal diplopia: Seeing double images side by side.
- Vertical diplopia: Seeing double images one on top of the other.
- Torsional diplopia: Seeing double images that are tilted relative to each other.
Type of Diplopia | Description | Common Cause |
Horizontal Diplopia | Double images side by side | Abducens nerve damage |
Vertical Diplopia | Double images one on top of the other | Oculomotor nerve damage |
Torsional Diplopia | Double images tilted relative to each other | Trochlear nerve damage |
Knowing the type of diplopia and its cause is key to finding the right treatment.
Prevalence and Statistics
It’s key to know how common double vision is after a stroke. This issue affects many stroke survivors’ lives. It’s a big concern for both patients and doctors.
About 60 percent of stroke patients see double vision to some degree. This shows why fixing vision problems is vital in recovery.
How Common is Double Vision After Stroke
Visual problems are common after a stroke. Between 10% to 30% of TIA patients see double vision. This includes those who have had a mini-stroke.
Double vision happens when the brain can’t control eye movements. This is because the stroke hit areas that control how our eyes move. This can cause our eyes to not line up right, leading to double vision.
Risk Factors for Developing Visual Complications
Several things can make visual problems after a stroke more likely. These include:
- The type and location of the stroke
- The severity of the initial stroke
- Pre-existing conditions such as diabetes or hypertension
- The patient’s age and overall health status
Knowing these risk factors helps doctors create better recovery plans.
Risk Factor | Impact on Visual Complications |
Stroke Type and Location | Affects the areas of the brain responsible for eye movement control |
Severity of Initial Stroke | More severe strokes are associated with a higher incidence of visual disturbances |
Pre-existing Conditions | Conditions like diabetes can exacerbate visual complications |
“The high prevalence of double vision after stroke highlights the need for thorough vision rehabilitation programs to tackle these visual issues effectively.”
— Medical Expert, Neurologist
Knowing about double vision after a stroke helps doctors tailor treatments. This ensures stroke survivors get the care they need.
Can Double Vision After Stroke Resolve on Its Own?
Many stroke survivors wonder if double vision will go away by itself. The answer depends on how well the body can recover and how vision can improve.
Spontaneous Recovery Rates
Some people see their double vision improve without treatment. Studies show that recovery rates vary. Some people start to see better within a few months.
Key statistics on spontaneous recovery include:
- Up to 50% of patients may see some improvement in the first month.
- But, the chance of getting better drops after six months.
Timeframes for Natural Improvement
How long it takes for double vision to improve can differ a lot. It depends on the stroke’s severity, where the brain was damaged, and the person’s health.
Starting treatment early and doing rehabilitation often can help recovery. Research shows that early and frequent vision therapy can help, even when recovery seems unlikely.
Research on Vision Recovery Post-Stroke
Many studies have looked into how vision can recover after a stroke. They found that a team effort in treatment is key. This includes medical care and vision therapy.
Notable findings include:
- The brain’s ability to change and adapt, helping vision recover.
- Rehabilitation programs can make a big difference in recovery.
- It’s important to keep checking and changing treatment plans for the best results.
Understanding how recovery can happen helps doctors give better advice and plan treatments.
Recovery Timeline Expectations
Knowing how long it takes to get better from double vision after a stroke is key. The time it takes to recover depends on the stroke type, where it happened, how much eye damage there is, your overall health, and how well you do in rehab.
Early Recovery Phase (First Month)
In the first month, your body starts to heal. Some people might see their double vision get better on its own. The brain can try to fix itself best in the early days after a stroke. But, how much you can recover varies a lot from person to person.
Intermediate Recovery (1-6 Months)
Between one and six months, you might see some more progress, but it might be slower. Starting vision therapy and rehab early can really help. It’s important to work with your doctors to make a rehab plan that fits you.
Long-Term Outcomes (Beyond 6 Months)
After six months, the chance for big improvements might get smaller. But, some people can keep getting better. At this point, finding ways to adapt and keeping up with rehab is key. People who can’t get rid of double vision might find help with special glasses or other tools.
Recovering from double vision after a stroke is a unique journey. The type and location of the stroke, how much vision is affected, and your health all affect how long it takes. By understanding these things and working with your healthcare team, you can make the most of your recovery.
Factors That Influence Vision Recovery
How well double vision goes away after a stroke depends on several key factors. Knowing these can help both patients and doctors plan better treatments. This can lead to better results.
Stroke Type and Location
The type and where the stroke happens greatly affect vision recovery. Strokes in areas that control eye movement can cause double vision. Ischemic strokes and hemorrhagic strokes have different effects on recovery. The brain area affected also matters, as some are more linked to eye movement.
Severity of Initial Vision Impairment
The first vision problem’s severity is a big factor in recovery. Those with mild double vision might do better than those with severe issues. The type of double vision and how it changes with eye movement also helps predict recovery.
Patient Age and Overall Health
A patient’s age and health are key in predicting recovery. Younger patients with fewer health problems usually do better. Age-related health issues can make recovery harder, so they’re important to consider.
Timing of Rehabilitation Interventions
When rehabilitation starts is very important for treating double vision after a stroke. Starting treatment early can make a big difference. Studies show that acting quickly can help the brain recover better.
Understanding these factors helps doctors give better predictions and create specific treatment plans. This can help address double vision after a stroke more effectively.
Diagnosing and Assessing Post-Stroke Diplopia
Diagnosing diplopia after a stroke starts with a detailed vision check. This step helps us understand how much the vision problem affects the patient’s daily life.
Comprehensive Vision Evaluation
At the heart of diagnosing post-stroke diplopia is a thorough vision check. This includes looking at the patient’s medical history, checking how well they can see, and examining how their eyes move. We use this info to find out why the double vision is happening and how to treat it.
The check-up usually includes:
- Visual acuity tests to see how sharp the vision is
- Cover tests to check if the eyes are aligned
- Ocular motility tests to see how well the eyes move
- Pupillary function tests to check the pupils’ reaction
Specialized Tests for Eye Movement Disorders
Special tests are needed to find out why someone has double vision after a stroke. These might include:
- Electrooculography (EOG) to see the electrical activity of the eye muscles
- Videooculography (VOG) to track eye movements closely
- Prism and cover tests to measure the angle of deviation
These tests help us figure out the eye movement problem. They guide us in creating a treatment plan that targets the issue.
Monitoring Vision Changes Over Time
Keeping an eye on how vision changes is key to seeing if treatment is working. We usually have regular check-ups to:
- Check for any changes in visual symptoms
- Adjust the treatment plan if needed
- Offer ongoing support and advice
By watching for changes, we can quickly adjust the treatment. This helps ensure the best outcome for the patient.
Test | Purpose | Benefit |
Visual Acuity Testing | Assess sharpness of vision | Helps determine the impact of diplopia on daily activities |
Electrooculography (EOG) | Record electrical activity of eye muscles | Provides detailed information on eye movement disorders |
Prism and Cover Testing | Measure the angle of deviation | Guides the development of a targeted treatment plan |
A leading neurologist once said,
“Diagnosing post-stroke diplopia needs a careful approach. It combines clinical checks with special tests to find the cause and plan treatment.”
By taking this detailed approach, we can accurately diagnose and assess post-stroke diplopia. This sets the stage for effective treatment and recovery.
Treatment Options for Diplopia After Stroke
Recovering from double vision after a stroke involves trying different treatments. These include medical care and vision therapy. Diplopia can make daily tasks hard, so finding the right treatment is key.
Medical Interventions
Medical treatments are important for managing double vision after a stroke. Prism glasses are often used to align images seen by each eye. This can reduce or get rid of double vision. Sometimes, Botox injections are used to relax eye muscles and improve alignment.
Other treatments might include medicines for underlying conditions. It’s important to work with a healthcare provider to find the best treatment for each person.
Vision Therapy Techniques
Vision therapy is also a big part of treating double vision after a stroke. Vision therapy exercises help retrain eye muscles. This improves eye movement and coordination.
Studies show vision therapy can greatly help patients with double vision. We use eye exercises and visual training programs. These are tailored to each patient’s needs and progress. Our goal is to improve visual function and reduce double vision symptoms.
By mixing medical treatments with vision therapy, we offer a full treatment plan for double vision after a stroke. Our focus is on personalized care. We make sure each patient gets the best treatment for their needs.
Vision Rehabilitation Programs
Recovering from stroke-induced diplopia often means joining vision rehabilitation programs. These programs help people regain their vision and improve their life quality.
Neuro-Optometric Rehabilitation
Neuro-optometric rehabilitation is a key part of these programs. It uses specific exercises to improve vision, mainly for those with vision problems from stroke or brain injuries.
This method trains the brain to handle visual information better. It’s customized for each person and can greatly improve their vision and comfort.
Multidisciplinary Approach to Recovery
A multidisciplinary approach is essential in vision rehabilitation. A team of experts, including optometrists, ophthalmologists, occupational therapists, and sometimes neurologists, work together. They address all aspects of visual dysfunction.
- Optometrists and ophthalmologists treat visual acuity and eye movement issues.
- Occupational therapists help patients adjust to their vision limitations and improve daily tasks.
- Neurologists offer insights into the neurological side of vision and manage related conditions.
Frequency and Duration of Therapy
The frequency and duration of therapy vary by person. It depends on the severity of vision loss, overall health, and how well they respond to therapy.
Therapy usually includes several sessions a week, lasting 30 to 60 minutes each. The program can last from a few months to a year or more, based on progress and needs.
Evidence for Rehabilitation Effectiveness
Research proves that vision rehabilitation programs are effective for stroke-related diplopia. Studies show big improvements in visual acuity, eye movement, and life quality for participants.
One study found that neuro-optometric rehabilitation greatly helped patients. They saw big improvements in their symptoms and abilities compared to those without therapy.
Adaptive Solutions for Persistent Double Vision
Adaptive solutions offer hope for those struggling with persistent double vision after a stroke. Several strategies can help alleviate its impact and improve quality of life.
Optical Devices and Prism Glasses
One effective approach to managing double vision is through the use of optical devices, like prism glasses. These glasses can correct double vision by aligning the images seen by each eye.
Prism Glasses: Prism glasses have prisms that refract light. This helps align the images seen by each eye. It can significantly reduce or eliminate double vision.
Type of Optical Device | Description | Benefit |
Prism Glasses | Glasses with prisms to align images | Reduces double vision |
Specialized Lenses | Lenses designed for specific vision needs | Improves visual clarity |
Patching Techniques
Patching techniques involve covering one eye to eliminate double vision. This can be a temporary solution until other treatments take effect.
Benefits of Patching: Patching can be very helpful for individuals with severe double vision. It provides immediate relief.
Environmental Modifications
Making certain changes to one’s environment can also help manage double vision. This might include adjusting lighting, using visual aids, or rearranging living spaces.
Environmental Adjustments: Simple changes, such as improving lighting or reducing clutter, can make a big difference in daily life.
Assistive Technology
Various assistive technologies are available to help individuals with double vision. These can range from specialized software to devices that aid in navigation.
By exploring these adaptive solutions, individuals with persistent double vision can find effective ways to manage their condition. This can improve their overall quality of life.
Living with Long-Term Visual Changes
Double vision after a stroke can make daily tasks hard. But, there are ways to make it easier. It takes patience, adapting, and sometimes medical help and lifestyle changes.
Coping Strategies for Daily Activities
Even simple tasks can be tough with double vision. But, there are ways to make it better. For example, an eye patch can help by blocking one eye’s view.
Also, making your environment better can help. This means better lighting and less clutter. It makes moving around easier.
Adaptive techniques are also helpful. Prism glasses or other devices can help align images. Occupational therapy can teach you how to do daily tasks despite vision problems.
“The key to managing double vision is not just treating the symptoms, but also adapting your lifestyle to accommodate your visual needs.”
Psychological Impact and Support Resources
Double vision can also affect your mind. It can make you feel frustrated, anxious, or sad. It’s important to recognize these feelings and get help.
Support groups, online or in-person, are great for sharing and learning. Professional counseling can also help you cope with emotional challenges.
When to Seek Additional Medical Help
Some people may not get better from double vision after a stroke. If it doesn’t go away or gets worse, see a doctor. They can find out why and help you.
Going back to your doctor regularly is important. They can check how you’re doing and change your treatment if needed. With the right help, you can manage double vision better.
Conclusion: The Outlook for Recovery from Stroke-Related Double Vision
Knowing the causes and treatments for double vision after a stroke is key. The recovery chances depend on several things. These include the stroke type and how well the patient does in rehab.
The recovery outlook also depends on how bad the vision problem was, the patient’s age, and health. A good treatment plan can really help. This plan includes medical care, vision therapy, and finding ways to adapt.
Recovery time can vary, but most progress happens in the first six months. Yet, with ongoing therapy, some people might see more improvement later.
By understanding what affects recovery and using a team approach to treatment, we can help patients with double vision after a stroke. This way, we offer the best chance for recovery.
FAQ
Does double vision after a stroke always go away?
No, double vision after a stroke doesn’t always go away. Recovery chances depend on the stroke type, location, and severity. Your overall health also plays a role.
How long does it take for double vision to improve after a stroke?
Recovery time for double vision after a stroke varies. Some see improvement in the first month. Others may take months or longer.
What are the risk factors for developing double vision after a stroke?
Risk factors include the stroke’s location and severity. Age and overall health also matter. Certain strokes, like those affecting the brainstem, are more likely to cause double vision.
Can vision therapy help improve double vision after a stroke?
Yes, vision therapy can help. Eye exercises and prism lenses can improve eye alignment. This reduces double vision symptoms.
Are there any adaptive solutions for persistent double vision?
Yes, there are many solutions. Optical devices, patching techniques, and environmental changes can help. Assistive technology also offers support.
Is double vision a sign of a stroke?
Double vision can be a stroke symptom. Look for sudden onset and other symptoms like weakness or numbness. Seek medical help immediately if you experience sudden double vision.
How is post-stroke diplopia diagnosed?
Diagnosing post-stroke diplopia involves a detailed vision evaluation. This includes a medical history, visual acuity tests, and eye movement disorder assessments.
What is neuro-optometric rehabilitation?
Neuro-optometric rehabilitation is a vision therapy type. It aims to improve vision and reduce double vision symptoms after a stroke. It involves a team effort with optometrists and other healthcare professionals.
Can double vision affect daily activities?
Yes, double vision can impact daily tasks. Reading, driving, and tasks needing visual attention can be challenging. Vision therapy and adaptive solutions can help manage these issues.
When should I seek additional medical help for double vision after a stroke?
Seek additional medical help for persistent or worsening double vision. Your healthcare provider can assess your condition. They will recommend further treatment or interventions as needed.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC6402759