Last Updated on November 13, 2025 by
Managing sickle cell crisis well is key to easing patient pain and avoiding serious issues. Sickle cell disease is a genetic disorder that affects hemoglobin, causing crises and other problems.
We focus on quick pain relief, keeping patients hydrated, stopping infections, and watching for serious issues. Hydration therapy is very important in handling vaso-occlusive crises, making them less severe.
Healthcare teams use a team effort to tackle pain control in vaso-occlusive crises. This approach greatly helps patients. Our goal is to give full care that meets patients’ urgent needs and lowers the chance of future problems. By following the latest sickle cell crisis management priorities, we ensure patients receive safe, effective, and timely treatment.
Key Takeaways
- Rapid pain control is essential in managing a sickle cell crisis.
- Hydration therapy is critical for reducing the severity of vaso-occlusive crises.
- Infection prevention measures are vital to prevent complications.
- Close monitoring for possible complications is necessary.
- A multidisciplinary approach improves patient outcomes.
Understanding Sickle Cell Disease and Crisis
It’s important to know about sickle cell disease to manage its crises well. This genetic disorder affects millions, mainly in Africa, the Middle East, and parts of India. It changes hemoglobin, causing abnormal red blood cells and health problems.
Global Impact and Prevalence of Sickle Cell Disease
Sickle cell disease is a big health issue worldwide, hitting hard in some areas. Studies show it affects many people, with big implications for healthcare. It’s key for healthcare workers to understand it to help manage it.
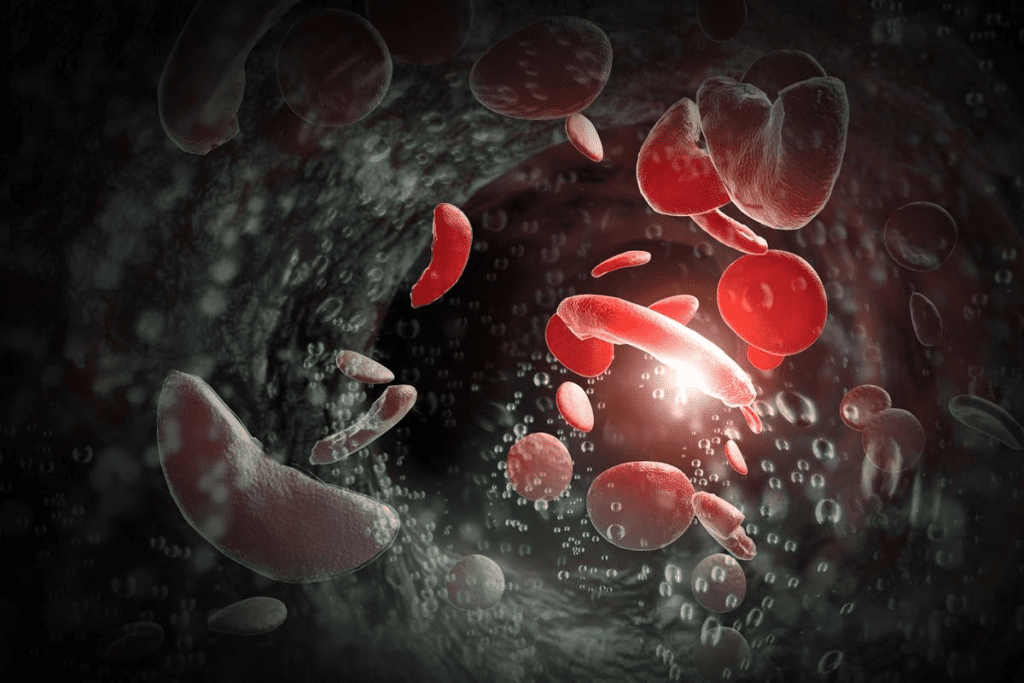
Pathophysiology of Vaso-Occlusive Crisis
A vaso-occlusive crisis happens when sickled red blood cells block blood vessels. This causes tissue ischemia and pain. It’s a major part of sickle cell disease and can be triggered by dehydration, infection, and extreme temperatures.
Knowing how these crises work is key to finding good ways to manage them. The blockage of blood vessels leads to acute pain episodes, a big challenge in managing the disease.
Triggers and Risk Factors for Acute Crisis
Finding out what triggers acute crises is important for preventing them. Common causes include dehydration, infections, and extreme temperatures. People with sickle cell disease are also at risk of oxygen desaturation, which can start a crisis.
Managing these risks with preventive care and quick action is vital. It helps lessen how often and how bad these crises are.
Understanding sickle cell disease’s global impact, how it works, and what triggers it helps healthcare providers. They can then create detailed plans to meet the complex needs of those with this condition.
Sickle Cell Crisis Management Priorities
When a patient comes in with a sickle cell crisis, quick action is key. We start by checking how bad the crisis is and what might have caused it. We also look for any serious problems.
Initial Assessment and Triage
Our first step is a fast and accurate check-up. We look at the patient’s past health, current symptoms, and what might have triggered the crisis. Important parts of this check-up are:
- Checking how much pain the patient is in and other symptoms
- Looking for signs of serious problems like acute chest syndrome or splenic sequestration
- Going over the patient’s medical history, including past crises and treatments
Emergency Department Protocol
Our plan for handling a sickle cell crisis in the emergency room includes a few main steps. Hydration is very important because it helps blood flow better and lowers sickled red blood cells. We also focus on pain management, using both opioid and non-opioid pain relievers as needed. We also watch for and treat any complications, like infections.
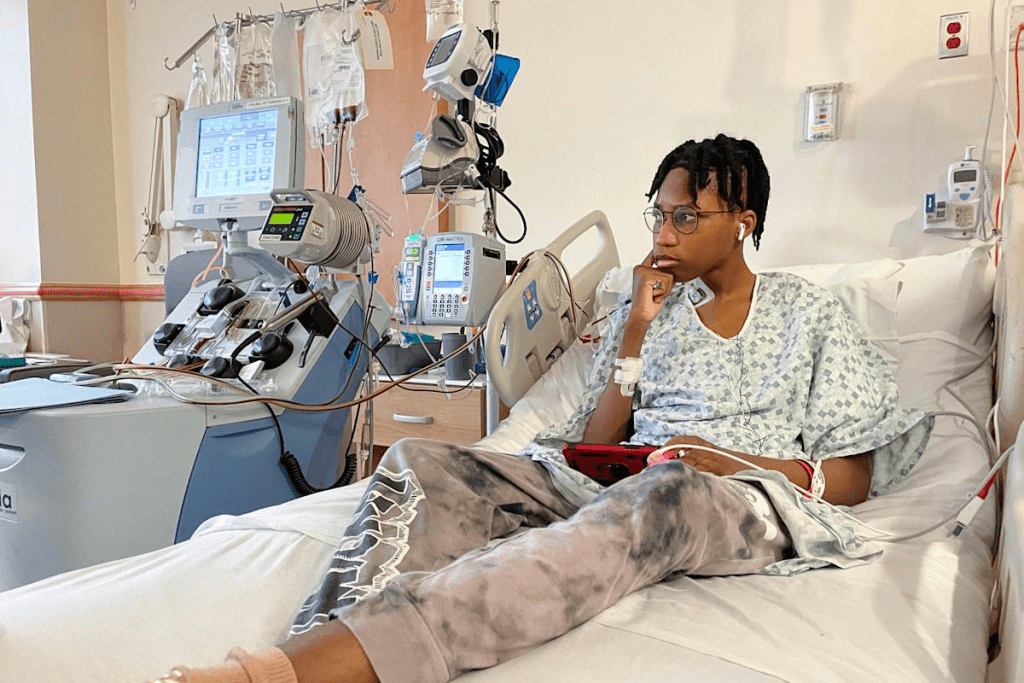
Patient Monitoring and Assessment
Keeping a close eye on the patient is vital in managing a sickle cell crisis. We watch their vital signs, pain levels, and overall health closely. We adjust our treatment plan as needed. Important parts of monitoring include:
- Regular checks on pain and how well the pain relief is working
- Watching for signs of complications or if things are getting worse
- Changing hydration and other support as needed
By following this plan, we can manage sickle cell crises well and help patients get better. Our focus on quick assessment, emergency room protocol, and constant monitoring helps us give the best care to these patients.
Pain Control Strategies in Vaso-Occlusive Crisis
Managing pain well is key in treating vaso-occlusive crises for sickle cell disease patients. It’s a complex task that needs a mix of strategies to tackle different pain types during a crisis.
Opioid Administration and Dosing
Opioids are vital for severe pain in vaso-occlusive crises. The right opioid and dose depend on the patient’s past experiences, pain level, and opioid tolerance. Intravenous opioids work fast and can be adjusted easily in acute settings.
It’s important to watch patients closely for respiratory depression when giving opioids. Always have naloxone ready as an antidote for overdose. The aim is to control pain well without harming the patient.
Non-Opioid Analgesics and Adjuvants
Non-opioid drugs and adjuvants are also key in pain management. Nonsteroidal anti-inflammatory drugs (NSAIDs) help reduce pain and the need for opioids. Adjuvants like gabapentin or pregabalin help with neuropathic pain.
- NSAIDs cut down inflammation and pain.
- Adjuvants like gabapentin tackle neuropathic pain.
- Using both can lower opioid doses and side effects.
Patient-Controlled Analgesia Considerations
Patient-controlled analgesia (PCA) is great for severe pain in vaso-occlusive crises. PCA lets patients give themselves pain relief as needed. This can lead to better pain control and less opioid use.
When using PCA, it’s vital to set the right lockout times and watch for pain control and side effects. Teaching patients and healthcare providers how to use PCA safely is essential.
- Check if the patient can use PCA well.
- Watch for signs of respiratory depression.
- Change PCA settings as needed for pain relief and side effects.
Hydration Therapy and Supportive Care
Hydration therapy is key in caring for patients with sickle cell crisis. It helps make blood less thick, making it easier for oxygen to reach tissues. We focus on giving fluids through an IV, oxygen, and keeping electrolytes balanced.
Intravenous Fluid Management
IV fluids are vital in treating a sickle cell crisis. Normal saline is often the first choice. We figure out how much fluid a patient needs based on their weight and health. The goal is to hydrate well without too much fluid.
- Patients with severe dehydration might get an initial fluid bolus.
- We adjust maintenance fluids based on how the patient is doing and fluid loss.
- Watching urine output helps us see if hydration is enough.
Oxygen Supplementation Guidelines
Oxygen is also very important, mainly for those with low oxygen levels or acute chest syndrome. We use supplemental oxygen to keep oxygen levels high. Deciding to use oxygen depends on how the patient is doing and oxygen levels.
- Use oxygen through nasal cannulas or face masks as needed.
- Keep oxygen saturation above 95%.
- Check if oxygen is needed regularly.
Electrolyte Balance and Monitoring
Keeping electrolytes balanced is also critical. We watch potassium and sodium levels closely. Electrolyte imbalances can cause serious problems, like heart rhythm issues.
In summary, hydration therapy and supportive care are essential for sickle cell crisis management. By managing IV fluids, oxygen, and electrolytes, we can greatly improve patient care.
Advanced Interventions for Complications
Advanced interventions are key in managing sickle cell disease complications. They are essential for patients in a sickle cell crisis.
Blood Transfusion Therapy Indications
Blood transfusions are vital for some sickle cell disease complications. They help by reducing the concentration of red blood cells that can sickle. This is critical for acute chest syndrome, stroke prevention, and severe anemia.
Doctors decide on transfusions based on the patient’s hemoglobin level and symptoms.
Management of Acute Chest Syndrome
Acute chest syndrome is a serious complication of sickle cell disease. It involves a new lung issue, fever, and breathing problems. We treat it aggressively with oxygen, pain management, and antibiotics. Blood transfusions help prevent further issues.
Infection Prevention and Antibiotic Therapy
Preventing infections is key in managing sickle cell disease. Patients face a higher risk due to immune system problems. We stress the need for vaccination and prophylactic antibiotics. Quick treatment with antibiotics is vital when infections happen.
Hydroxyurea Therapy for Crisis Reduction
Hydroxyurea can reduce sickle cell crises and improve outcomes. It boosts fetal hemoglobin, making red blood cells less likely to sickle. We consider it for patients with frequent crises or severe disease.
These advanced interventions greatly improve sickle cell disease management. They enhance patient outcomes and quality of life.
Conclusion: Multidisciplinary Approach to Sickle Cell Crisis
Managing a sickle cell crisis well needs a team effort. This includes quick pain relief, staying hydrated, preventing infections, and caring for patients. It’s key to work together to better the lives of those with sickle cell disease.
A team of healthcare experts is vital for sickle cell crisis care. The NHLBI’s 2014 guidelines support this. They say a team approach ensures patients get all the care they need.
By working together and focusing on patient care, we can make a big difference. This approach improves outcomes and quality of life for those with sickle cell disease.
FAQ’s:
What are the priority management strategies for sickle cell crisis?
Managing sickle cell crisis focuses on quick pain relief, keeping the body hydrated, and preventing infections. It also involves watching for serious complications like acute chest syndrome.
How is pain control managed in a vaso-occlusive crisis?
Pain control in vaso-occlusive crisis uses opioids, non-opioid pain relievers, and patient-controlled analgesia. Each patient gets a care plan tailored to their needs.
What is the role of hydration therapy in managing sickle cell crisis?
Hydration therapy, like intravenous fluids, is key in managing sickle cell crisis. It helps prevent dehydration and keeps electrolyte levels balanced.
When is oxygen supplementation necessary in sickle cell disease?
Oxygen is needed in sickle cell disease when there’s low oxygen or acute chest syndrome. It helps tissues get enough oxygen.
What are the key components of emergency department protocols for sickle cell crisis?
Emergency department protocols for sickle cell crisis include quick assessment and triage, monitoring, pain relief, hydration, and infection prevention.
How is acute chest syndrome managed in sickle cell disease?
Managing acute chest syndrome involves oxygen, pain relief, hydration, and blood transfusions. Antibiotics are also used to fight off infections.
What is the role of blood transfusion therapy in managing sickle cell crisis?
Blood transfusions help manage sickle cell crisis by reducing sickled red blood cells. This lowers the risk of complications like acute chest syndrome.
How can infection be prevented in patients with sickle cell disease?
Preventing infections in sickle cell disease includes antibiotics, vaccines, and teaching patients to recognize early signs of infection. Quick treatment is also key.
What is the importance of a multidisciplinary approach in managing sickle cell crisis?
A team effort is vital in managing a sickle cell crisis. It involves healthcare providers, patients, and families working together for better care and outcomes.
How does hydroxyurea therapy help in reducing sickle cell crises?
Hydroxyurea therapy reduces sickle cell crises by lowering the number of painful episodes. It may also lower the risk of acute chest syndrome and other serious issues.
References
- National Heart, Lung, and Blood Institute. (2014). The Management of Sickle Cell Disease. Retrieved from https://www.nhlbi.nih.gov/sites/default/files/media/docs/SCD_Report_508_FINAL.pdf
- American Society of Hematology. (2020). Guideline on Sickle Cell Disease: Management of Acute and Chronic Pain. Retrieved from https://www.hematology.org/guidelines/sickle-cell-disease
- Centers for Disease Control and Prevention. (2024). Emergency Department Visits for Painful Crises. Retrieved from https://www.cdc.gov/ncbddd/sicklecell/painful-crises-emergency-visits.html
- The American Academy of Pediatrics. (2021). Clinical Practice Guideline for Sickle Cell Disease. Pediatrics, 147(S1), S1-S48. Retrieved from https://publications.aap.org/pediatrics/article/147/Supplement_1/e20172605/181650/Clinical-Practice-Guideline-for-Sickle-Cell-Disease
- U.S. National Library of Medicine. (2023). Acute Pain Management in Pediatric Sickle Cell Crisis. Pediatric Emergency Care, 39(1), 1-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10303862/





