Age-related macular degeneration (AMD) is a big problem for people over 60. It makes about 11 million Americans lose their vision. At Liv Hospital, we teach people about how some medicines can harm their eyes. We answer: what medication causes macular degeneration? This vital guide lists the top 7 drugs to avoid for your eye health.
Commonly prescribed medications like some blood pressure meds, anticoagulants, and anti-inflammatory drugs can raise AMD risk. It’s key to check your meds and treatment plans to keep your eyes safe.
Key Takeaways
- AMD affects about 11 million Americans and is a top cause of vision loss in those over 60.
- Some medicines can up the risk of getting AMD or make it worse.
- Medicines like some blood pressure meds, anticoagulants, and anti-inflammatory drugs are linked to AMD.
- It’s important to look at your meds and treatment plans to protect your vision.
- Liv Hospital focuses on a patient-centered approach to reviewing meds and keeping up with the latest clinical protocols.
Understanding Age-Related Macular Degeneration (AMD)
It’s important to know about age-related macular degeneration (AMD) as we get older. AMD affects the macula, which is key for clear vision. As more people live longer, AMD becomes a bigger health issue.
What is Macular Degeneration?
Macular degeneration means the macula gets worse, causing vision loss. The macula is a small but vital part of the eye. It helps us see things clearly. AMD can make it hard to read, drive, or even see faces.
Prevalence and Impact in the United States
In the U.S., AMD is a top reason for vision loss in older people. About 11 million people have it. As more Americans live longer, more will get AMD. This can really change their lives, making everyday tasks harder.
Types of AMD: Dry and Wet
AMD comes in two types: dry and wet. Dry AMD happens when drusen (deposits) build up under the macula. This causes slow vision loss. Wet AMD has abnormal blood vessels that leak, leading to quick vision loss. Knowing the type helps doctors choose the right treatment.
The Connection Between Medications and Macular Degeneration

There’s a complex link between some medications and macular degeneration. As we get older, the chance of getting age-related macular degeneration (AMD) goes up. Knowing how medicines affect this risk is key for both patients and doctors.
How Drugs Can Affect Retinal Health
Some medicines can harm the retina in different ways. This might up the risk of AMD or make it worse. For example, hydroxychloroquine and chloroquine, used for autoimmune diseases, can harm the retina.
Studies show that medicines can affect the retina in many ways. They might change how the retina works or interact with other drugs to increase AMD risk. Knowing how medicines affect the retina is vital for spotting risky ones.
Risk Factors and Medication Interactions
Looking at AMD risk factors means considering medicines and how they work together. Medicine interactions can greatly increase the risk of bad effects on the retina. For instance, mixing certain blood thinners with other drugs can raise the risk of retina bleeding.
Medication Category | Potential Risk | Interaction Risk |
Anticoagulants | Bleeding complications | High |
Antimalarials | Retinal toxicity | Moderate |
Corticosteroids | Intraocular pressure increase | Moderate to High |
Healthcare providers can make better choices about treatments by knowing the risks of medicines and their interactions. It’s important for patients to talk to their doctors about their medicines to check for any risks to their retina.
What Medication Causes Macular Degeneration? The Research Overview
Exploring medications linked to macular degeneration is key. Recent studies have shed light on several risk factors. This has sparked a lot of interest in the field.
Current Scientific Understanding
Research shows some meds might raise macular degeneration risk. This includes treatments for high blood pressure, heart disease, and depression. For example, some antihypertensive meds might increase AMD risk.
To grasp the current understanding, let’s look at some studies. Below is a table of medications linked to macular degeneration.
Medication Class | Specific Medication | Potential Risk |
Antihypertensives | Apresoline (Hydralazine) | Increased risk of AMD |
Anticoagulants | Warfarin (Coumadin) | Bleeding complications in wet AMD |
NSAIDs | Aspirin | Protective effects vs. bleeding risk |
Corticosteroids | Systemic corticosteroids | Potential retinal damage |
Limitations in Research
Current research offers insights but has its limits. Many studies rely on observational data, which can be biased. The complex interaction between meds and patient factors makes it hard to pinpoint causes.
Most studies focus on specific groups, not the whole patient population. More research is needed to fully understand the link between meds and macular degeneration.
How to Interpret Medication Risks
Assessing medication risks involves looking at many factors. Patients should talk to their doctors about their risk based on their health, meds, and lifestyle.
Doctors can help patients weigh medication benefits against risks. This way, patients can make informed decisions about their treatment. Understanding the research helps patients manage their eye health better.
Blood Pressure Medications: Vasodilators and AMD Risk
Some blood pressure drugs, like vasodilators, might affect AMD risk. Vasodilators widen blood vessels to improve blood flow. But, their effect on the retina and AMD risk is being studied.
Apresoline (Hydralazine): Mechanism and Concerns
Apresoline, or Hydralazine, is a vasodilator for high blood pressure. It relaxes blood vessels for better blood flow. But, its effect on the retina has raised concerns.
Mechanism: Hydralazine relaxes blood vessel muscles. This can lower blood pressure but might affect retina blood flow.
Loniten (Minoxidil): Impact on Retinal Blood Flow
Loniten, or Minoxidil, is a strong vasodilator for severe hypertension. It changes blood flow a lot. Research shows it might affect AMD risk.
Retinal Blood Flow Concerns: Minoxidil’s effect on retinal blood flow can harm the retina, worsening AMD.
Statistical Evidence: 20% vs 8.2% Risk Comparison
Studies show the AMD risk difference between vasodilator users and non-users. One study found a 20% AMD risk increase in vasodilator users, versus 8.2% in controls.
Medication | AMD Risk Increase | Control Group Risk |
Apresoline (Hydralazine) | 18% | 8.2% |
Loniten (Minoxidil) | 22% | 8.2% |
It’s important to know how blood pressure drugs affect AMD risk. Vasodilators like Apresoline and Loniten help with hypertension but might increase AMD risk. So, careful monitoring is needed.
Anticoagulant Medications: Warfarin and Bleeding Complications
Anticoagulant drugs like Warfarin can affect AMD, raising bleeding risks. These drugs stop blood clots, which can be deadly. But, they can also increase bleeding in AMD patients.
Warfarin (Coumadin): How It Works
Warfarin, or Coumadin, stops blood clotting by affecting liver production. It’s good for preventing blood clots but can cause bleeding. This is a big worry for AMD patients with fragile blood vessels.
It’s vital for Warfarin users to get regular blood tests. These tests check if their blood is clotting right. This balance is key to avoid both clotting and bleeding problems.
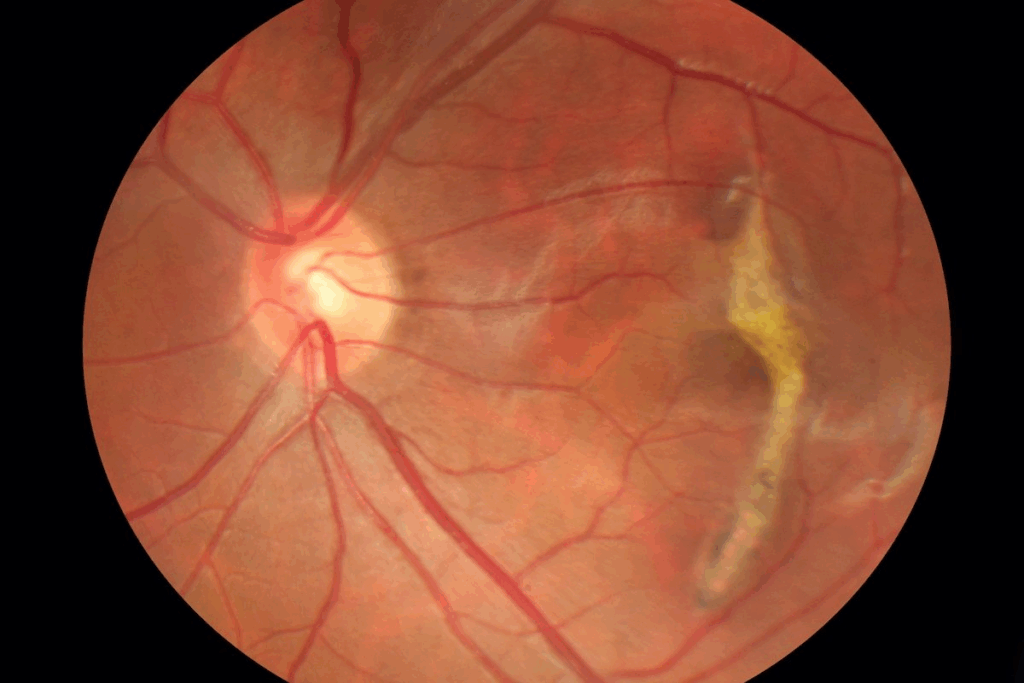
Impact on Wet AMD Progression
Wet AMD has blood vessels growing under the macula, leading to fluid leaks and retina damage. Anticoagulants like Warfarin can make this worse by increasing the chance of bleeding.
“The risk of subretinal hemorrhage is a significant concern in patients with wet AMD, and anticoagulation therapy may further elevate this risk.”
Research shows that anticoagulants can make wet AMD worse. This is because of the higher risk of bleeding.
Subretinal Hemorrhage Risk and Vision Loss
Subretinal hemorrhage is a severe AMD complication. It causes sudden vision loss. Anticoagulants make this risk even higher because they prevent blood from clotting well.
Quick medical help is critical for anyone with sudden vision changes. Fast action can help save vision.
NSAIDs and Their Double-Edged Effect on AMD
NSAIDs, like Aspirin, have both good and bad effects on AMD. It’s important to understand this complex relationship. This knowledge helps doctors make better choices for their patients.
Aspirin: Protective Effects vs. Bleeding Risk
Aspirin is a common NSAID with anti-inflammatory and antiplatelet properties. It might help protect against AMD by reducing inflammation. But, Aspirin can also increase the risk of bleeding, which is a big concern for AMD patients.
Risk vs. Benefit Analysis: Research on Aspirin and AMD shows mixed results. Some studies suggest it might protect against AMD, while others point out the bleeding risk. Finding a balance between these factors is key.
Other Common NSAIDs and Their Impact
NSAIDs like ibuprofen and naproxen are also used for their anti-inflammatory effects. Their impact on AMD is not as well-studied as Aspirin’s. But, they work in similar ways, which could affect AMD risk.
- Ibuprofen: Some studies suggest it might have a neutral effect on AMD, though more research is needed.
- Naproxen: Limited data are available on naproxen’s specific impact on AMD, necessitating further investigation.
Special Concerns When Combined with Anticoagulants
When NSAIDs are taken with anticoagulants, the risk of bleeding goes up. This is a big worry for AMD patients, as it increases the chance of subretinal hemorrhage.
Medication Combination | Bleeding Risk Level | AMD Risk Consideration |
Aspirin + Warfarin | High | Increased risk of subretinal hemorrhage |
Ibuprofen + Anticoagulant | Moderate to High | Potential for increased AMD progression |
Naproxen + Anticoagulant | Moderate to High | Limited data, cautious use recommended |
Clinical Considerations: Doctors need to think carefully before prescribing NSAIDs to AMD patients, even more so when combined with anticoagulants. It’s important to watch for signs of bleeding and AMD progression.
Corticosteroids: Inflammation Control at a Cost
The link between corticosteroids and Age-related Macular Degeneration (AMD) is a growing area of study. Corticosteroids are powerful anti-inflammatory drugs used for many conditions, including eye diseases.
They can be given in different ways: through the body (systemically) or directly to the eye (ocularly). Each method has its own uses and side effects. Knowing the difference between systemic and ocular corticosteroids is key to understanding their impact on AMD.
Systemic and Ocular Corticosteroids
Systemic corticosteroids, like prednisone, treat many inflammatory diseases. They can affect the eye, possibly changing how AMD progresses.
Ocular corticosteroids are applied directly to the eye to treat conditions like uveitis or macular edema. They can reduce eye inflammation but might also harm the retina.
Mechanisms of Possible Retinal Damage
Studies show corticosteroids can harm the retina in several ways. They can change gene expressions related to inflammation and oxidative stress, leading to retinal damage.
They can also raise intraocular pressure (IOP), which is a risk factor for glaucoma and AMD progression.
Monitoring Recommendations for Long-term Users
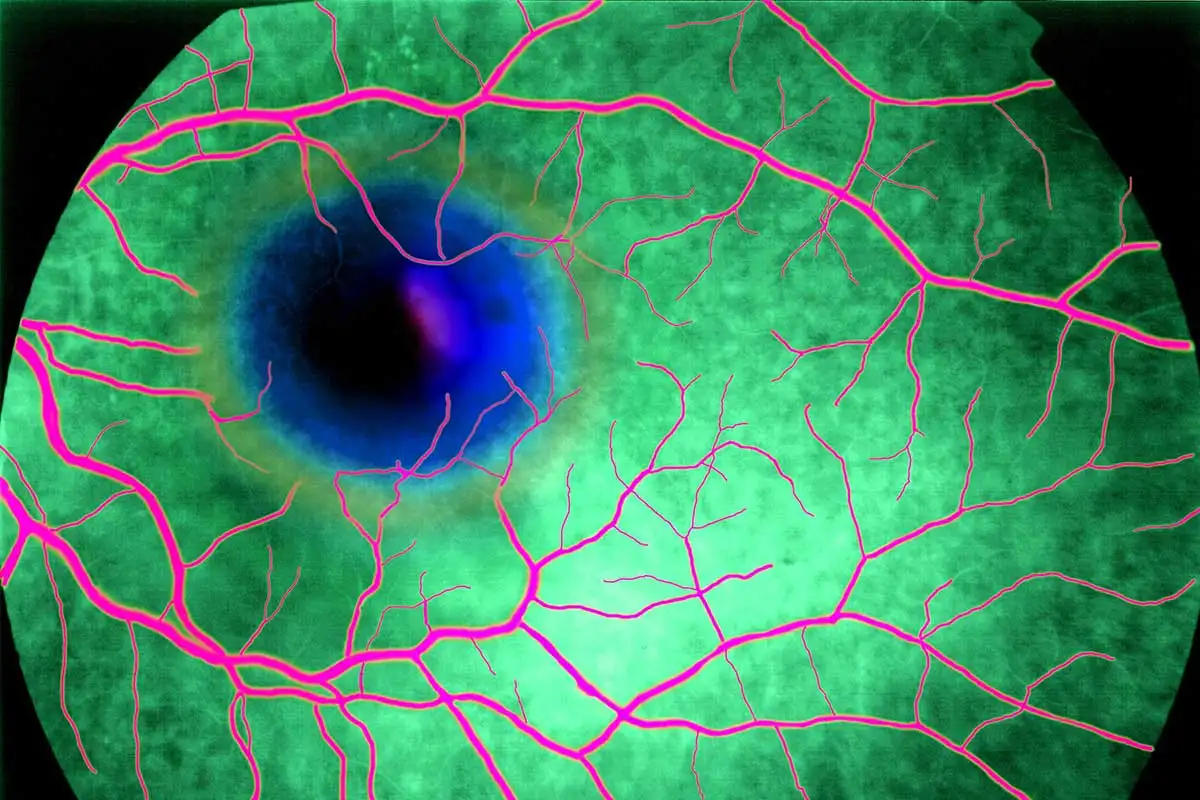
People on long-term corticosteroids need regular eye checks. This includes detailed eye exams, retinal imaging, and tests of visual function.
We advise patients to talk to their doctor about their medication. Discuss the risks and benefits of corticosteroids for their eye health.
Monitoring Aspect | Recommendation | Frequency |
Comprehensive Eye Exam | Assess overall eye health, including IOP measurement | At least annually |
Retinal Imaging | Use OCT to monitor retinal changes | Every 6-12 months |
Visual Function Assessment | Evaluate visual acuity and field | At each visit |
PDE5 Inhibitors: Beyond Erectile Dysfunction
PDE5 inhibitors, like Viagra and Cialis, are used for erectile dysfunction. They might also affect eye health. This has led to research on their impact on Age-related Macular Degeneration (AMD).
Visual Side Effects of Viagra, Cialis, and Levitra
Some users of PDE5 inhibitors experience visual side effects. These can include color vision changes, blurred vision, and light sensitivity. For example, Viagra can cause a blue-tinged vision in some people.
These side effects are usually short-lived. But, they have led to research on their long-term effects on the retina.
Connection to AMD Pathways
Research on PDE5 inhibitors and AMD has shown mixed results. Some studies suggest they might improve blood flow to the eyes, helping AMD patients. But, others worry they could worsen retinal conditions.
The exact way PDE5 inhibitors affect AMD is not clear. More research is needed to understand this.
Guidelines for Patients with Existing Eye Conditions
Patients with eye conditions like AMD should talk to an eye doctor before using PDE5 inhibitors. A thorough eye exam is important to weigh the risks and benefits.
It’s key to watch for vision changes and adjust AMD treatment plans as needed. Patients should also know the risks and benefits of PDE5 inhibitors for their eye health.
By being cautious and informed, we can help patients make the right choices for their treatment.
Prostaglandin Analogs: Glaucoma Treatment Concerns
Prostaglandin analogs are used to treat glaucoma. But, they might affect age-related macular degeneration (AMD). It’s key to know how these drugs work and what they mean for patients.
Latanoprost and Similar Medications
Latanoprost is a common drug for glaucoma. It helps by making more fluid leave the eye, lowering pressure. But, research has looked into how Latanoprost affects eye blood flow and macular health. Other drugs like bimatoprost and travoprost work in similar ways but might affect the retina differently.
Effects on Ocular Blood Flow and Macular Health
Studying how prostaglandin analogs affect eye blood flow is important. These drugs might change blood flow to the retina, affecting AMD patients. It’s unclear if these drugs help or hurt AMD, and more research is needed.
Balancing Glaucoma Control and AMD Risk
It’s hard to manage glaucoma without worrying about AMD. For those with glaucoma and AMD risk, regular checks and a detailed treatment plan are vital. This might include changing medications, making lifestyle changes, and eye exams to watch for AMD signs. Knowing the risks and benefits of these drugs helps doctors care for patients better.
Hydroxychloroquine and Chloroquine: Antimalarials with Retinal Toxicity
Hydroxychloroquine and Chloroquine are key in managing autoimmune diseases. But, they can cause serious eye problems. These drugs have been used for many years to treat diseases like rheumatoid arthritis and lupus.
Autoimmune Disease Treatments and Eye Health
These drugs work well against autoimmune diseases because they reduce inflammation. Yet, long-term use can harm the retina, leading to permanent vision loss. The risk of retinal damage is a significant concern that needs constant monitoring.
It’s important to think about the risks of these medications, even more so for those with eye problems. We must balance the benefits of treating autoimmune diseases with the risks to eye health.
Cumulative Damage and Dose-Dependent Risk
The risk of eye damage from Hydroxychloroquine and Chloroquine grows with time and dose. Studies show that the risk jumps up after a certain amount is taken. Regular monitoring is key to catch early signs of eye damage.
- Cumulative dose threshold: The risk increases substantially after a cumulative dose of 1000g or more of Hydroxychloroquine.
- Dose-dependent risk: Higher daily doses increase the risk of retinal toxicity.
- Duration of use: Longer treatment durations are associated with a higher risk.
Required Screening Protocols
To lower the risk of eye damage, regular check-ups are vital for those taking Hydroxychloroquine and Chloroquine. Annual screenings are advised for most, but the schedule can change based on individual risks.
“Regular retinal screening is critical for early detection of hydroxychloroquine retinopathy. Automated visual field testing and spectral-domain optical coherence tomography are recommended as part of the screening protocol.” – American Academy of Ophthalmology
Patients on these drugs should get full eye exams. This includes:
- Visual field testing to detect any changes in retinal sensitivity.
- Spectral-domain optical coherence tomography (SD-OCT) to assess retinal structure.
- Fundus autofluorescence imaging to identify early signs of retinal toxicity.
Following these screening steps can help reduce the risk of vision loss from Hydroxychloroquine and Chloroquine.
Safer Alternatives and Risk Reduction Strategies
There are safer ways to lower AMD risk. For those at risk, managing medications is key. We look at other options, supplements, and lifestyle changes for better eye health.
Alternative Medication Options for High-Risk Patients
High-risk patients can find safer meds. For example, those on hydroxychloroquine should watch their eyes closely. If possible, switch to safer options.
Some safer choices include:
- Switching to antimalarial drugs with less eye harm.
- Adjusting treatments for high blood pressure or glaucoma to lower AMD risk.
Nutritional Supplements for Eye Protection
Supplements can help keep your eyes healthy. Some vitamins and minerals slow AMD’s growth.
Nutritional Supplement | Benefit for AMD |
Omega-3 fatty acids | Supports retinal health |
Lutein and Zeaxanthin | Protects macular region |
Vitamin C and E | Antioxidant properties |
Lifestyle Modifications to Support Macular Health
Changing your lifestyle can also help with AMD risk. This includes adjusting meds and taking supplements.
- Quit Smoking: Stopping smoking can lower AMD risk a lot.
- Dietary Changes: Eat more leafy greens and omega-3s.
- Regular Exercise: Stay active to keep blood vessels healthy.
- Protecting Eyes from UV Light: Wear sunglasses with UV protection.
By making these changes, you can manage AMD risk and keep your vision sharp.
Conclusion: Balancing Medication Needs and Eye Health
Certain medications can raise the risk of age-related macular degeneration (AMD). It’s important to think about how medications affect eye health. We need to weigh the benefits of medications against the risks to our eyes.
Knowing how medications and AMD are linked helps us take action. We can look into other medications or supplements for our eyes. For example, if you’re on Apresoline, talk to your doctor about other blood pressure meds.
Managing AMD risk means watching how medications interact with each other. Regular eye checks are key. This helps catch any eye problems early.
Working with doctors, we can lower AMD risk and stay healthy. It’s all about finding the right balance between medication and eye care. This keeps our vision sharp and our lives full.
FAQ
What is Age-related Macular Degeneration (AMD)?
AMD is a condition that affects the macula, the part of the retina. It leads to vision loss in older adults.
What medications can cause Macular Degeneration?
Some medications, like Apresoline and Warfarin, can raise the risk of Macular Degeneration. Also, corticosteroids, PDE5 inhibitors, prostaglandin analogs, and antimalarials like Hydroxychloroquine can increase this risk.
How do blood pressure medications affect AMD risk?
Certain blood pressure medications, such as vasodilators, can increase AMD risk. They alter retinal blood flow.
Can Warfarin cause vision loss in AMD patients?
Yes, Warfarin can increase the risk of subretinal hemorrhage and vision loss in patients with wet AMD.
Are NSAIDs safe for patients with AMD?
NSAIDs have a dual effect on AMD. They may protect against AMD but can also increase bleeding risks, mainly when used with anticoagulants.
What are the risks of using corticosteroids for AMD patients?
Corticosteroids can cause retinal damage and increase AMD progression risk, mainly with long-term use.
Can PDE5 inhibitors like Viagra cause AMD?
PDE5 inhibitors, like Viagra, may have visual side effects and could be linked to AMD. More research is needed to confirm this.
How do prostaglandin analogs affect AMD risk?
Prostaglandin analogs used in glaucoma treatment can affect ocular blood flow and macular health. This may increase AMD risk.
What are the risks of using Hydroxychloroquine and Chloroquine?
Hydroxychloroquine and Chloroquine can cause retinal toxicity. The risk is cumulative and dose-dependent, requiring regular screening.
Are there safer alternatives for patients at high risk of AMD?
Yes, there are alternative medications, nutritional supplements, and lifestyle changes that can help reduce AMD risk.
What medications cause macular degeneration?
Medications that can cause macular degeneration include certain blood pressure medications, anticoagulants, corticosteroids, PDE5 inhibitors, prostaglandin analogs, and antimalarials.
Are there any drugs linked to macular degeneration?
Yes, several drugs have been linked to macular degeneration, including Apresoline, Warfarin, and Hydroxychloroquine.
Can medications cause macular degeneration?
Yes, certain medications can increase the risk of macular degeneration. It’s important to discuss risks and benefits with your healthcare provider.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6210876/