The human body has a special relationship with its eyes. It keeps a balance between protecting and preventing damage. The eyes have immune privilege, meaning the immune system doesn’t attack them.Discussing the unique way eyes are protected from a systemic attack, or if your immune system found out about your eyes.
We look into how the eyes are protected from harm. This is key to keeping our vision safe. The eyes are very important for our health and sight.
The immune system’s interaction with the eyes is complex. If it gets out of balance, it can cause big problems. Knowing how the immune system and eyes work together is vital.
Key Takeaways
- The eyes exist in a state of immune privilege, protecting them from immune system damage.
- The immune system maintains a delicate balance between protection and damage prevention in the eyes.
- Dysregulation of the immune system’s interaction with the eyes can lead to serious complications.
- Ocular immune privilege is key for keeping our vision and health safe.
- Understanding the immune system’s interaction with the eyes is essential for appreciating ocular immune privilege.
The Unique Relationship Between Eyes and Immunity
The eyes and the immune system work together carefully. This balance is key to avoid damage and keep our vision clear. The eyes’ special design and function make this teamwork essential.
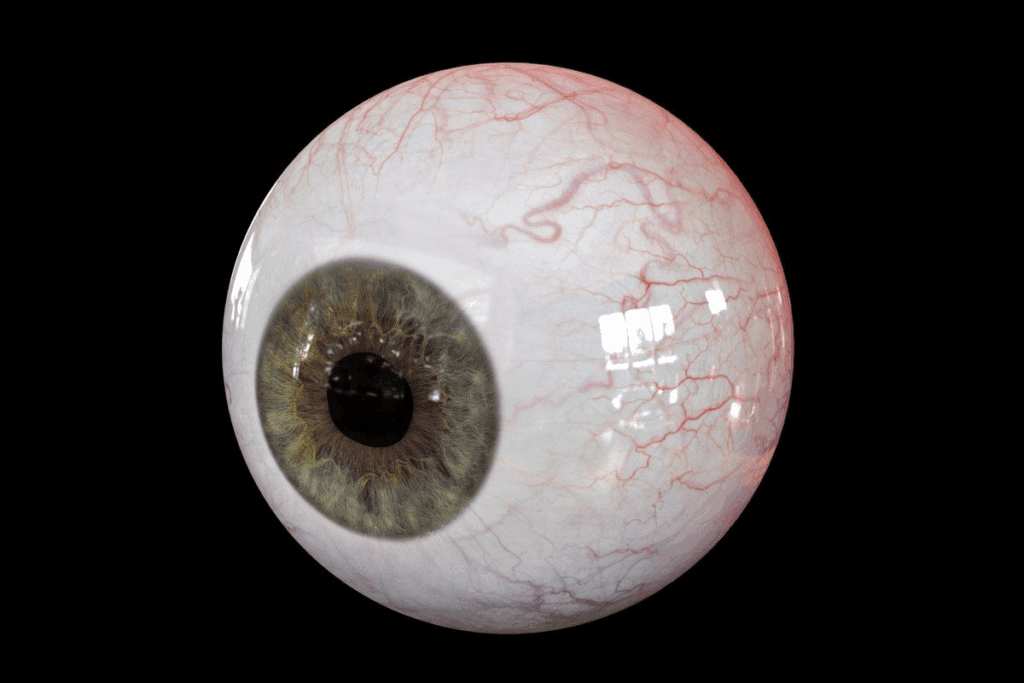
The Delicate Nature of Ocular Tissues
Ocular tissues are very sensitive and special. They can easily get hurt by the immune system. Keeping the eyes clear is vital for our sight, and any damage can be permanent.
The eye’s parts, like the cornea and retina, are vital for seeing but hard for the immune system to handle. The cornea, for example, has no blood vessels. This makes it less prone to inflammation but also limits its ability to get nutrients and immune cells.
Why Vision Preservation Requires Immune Regulation
The immune system must be carefully managed around the eyes to protect our vision. This careful balance is necessary to avoid autoimmune attacks and too much inflammation. We’ll look at how the body keeps this balance.
One important way is through “immune privilege.” This means some parts of the eye are shielded from the immune system’s full power. This protection is made possible by special molecules and cells that control the immune response in the eye.
Mechanism | Description | Effect on Immune System |
Immune Privilege | Protection of certain eye structures from immune responses | Reduces risk of autoimmune damage |
Anti-inflammatory Molecules | Presence of molecules like TGF-β that suppress inflammation | Minimizes inflammation and scarring |
Regulatory T Cells | T cells that modulate and suppress immune responses | Prevents excessive immune activation |
Understanding these mechanisms helps us see how closely the eyes and immune system are connected. This knowledge is vital for finding treatments for eye problems caused by the immune system and for keeping our vision sharp.
Understanding Ocular Immune Privilege

Our eyes are protected by a complex system called ocular immune privilege. This system is key to understanding how our immune system works with eye tissues without harm. It’s not just a passive state; it’s an active process. It involves many parts of the immune system working together to protect our vision.
Definition and Evolutionary Advantage
Ocular immune privilege means the eye can avoid damage from the immune system. This is vital for keeping our vision safe, as immune responses in the eye can cause harm. The eye’s ability to avoid immune damage is a big advantage in evolution.
The eye is like the brain and testes in being “immune-privileged.” This means the immune system is controlled to prevent too much inflammation and damage in these areas. For the eye, this control is essential to keep the delicate structures needed for vision.
Historical Perspective on Eye Immunity Research
Research on ocular immune privilege has a long history, spanning decades. Early studies aimed to understand why the eye could accept foreign grafts without a strong immune reaction. These studies helped build our current understanding of ocular immune privilege.
The idea of immune privilege was first seen in corneal transplantation. It was noticed that corneal grafts were often accepted by the host’s immune system, unlike grafts elsewhere. This led to more research into the mechanisms behind ocular immune privilege.
If Your Immune System Found Out About Your Eyes
The immune system does know about the eyes and works to protect them. The eyes are not alone; they have a special connection with the immune system. This connection is key to keeping our vision healthy.
Debunking the “Hidden Eyes” Myth
The idea that the eyes are hidden from the immune system is wrong. The truth is, the eyes are not isolated. They have a special bond with the immune system that helps protect and preserve vision.
The eyes have developed complex ways to talk to the immune system. This is important for stopping infections and keeping the eye’s delicate tissues safe.
How Your Immune System Recognizes Yet Tolerates Eye Tissues
The immune system can spot eye tissues but doesn’t attack them. This is key for keeping the eyes healthy and working right.
Several things help the immune system be gentle with the eyes. For example, the eye has special factors that calm down the immune system. The eye’s unique shape also helps keep it safe from the immune system.
Mechanism | Description | Function |
Immunosuppressive Factors | Presence of factors like TGF-β in the ocular environment | Suppresses immune response against eye tissues |
Ocular Anatomy | Unique structure of the eye limiting exposure to immune cells | Reduces the likelihood of autoimmune reactions against the eye |
Blood-Retinal Barrier | Selective permeability controlling the exchange between blood and retina | Protects the retina from harmful substances and immune cells |
It’s important to understand how the immune system deals with the eyes. This knowledge helps us find new ways to treat eye problems caused by the immune system. By learning more about the eye and immune system connection, we can protect our vision better.
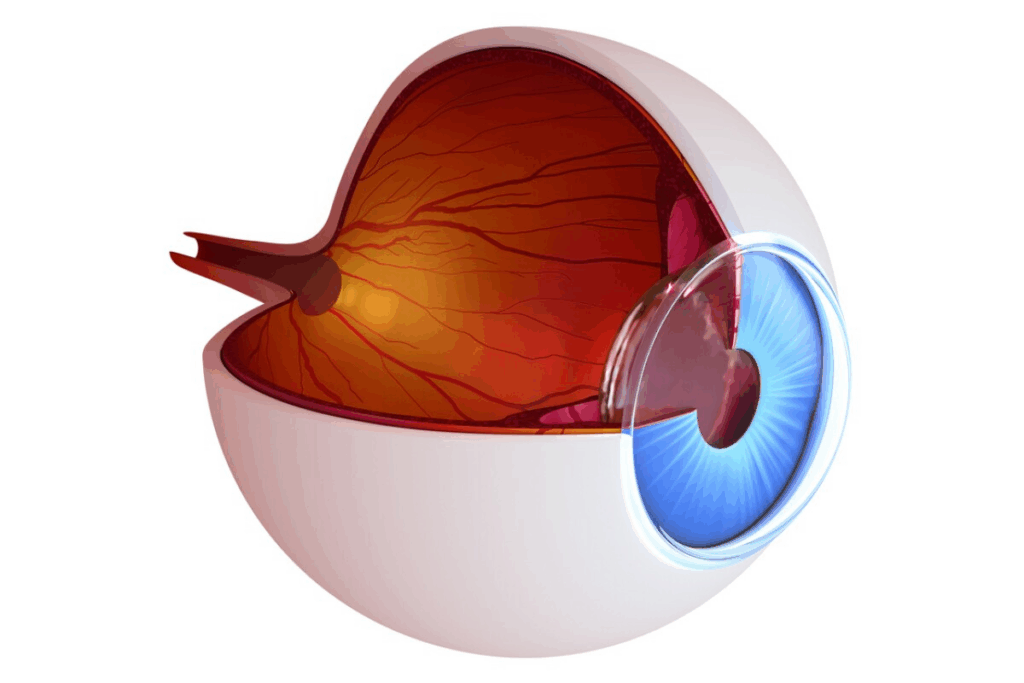
The Blood-Retinal Barrier: Nature’s Gatekeeper
The blood-retinal barrier is a key part of keeping our eyes safe. It controls what can get into the retina. This helps keep our vision clear and free from immune problems.
Anatomical Structure and Cellular Components
The blood-retinal barrier is made up of tight junctions. These are between the cells of the retinal vessels and the retinal pigment epithelial cells. These tight junctions block most molecules and cells from getting into the retina.
Pericytes and astrocytes help keep the barrier strong. They are important for keeping the barrier working right.
Selective Permeability and Immune Cell Regulation
The barrier lets good stuff through but keeps bad stuff out. This is key for the eyes to stay healthy. It also controls how immune cells move, stopping too much inflammation.
This barrier is essential for our vision. If it breaks down, it can cause eye diseases. So, it’s vital for our eye health.
Absence of Conventional Lymphatic Drainage
The eyes are special organs that don’t need traditional lymphatic drainage to work. This is key to understanding how the immune system and eyes interact.
Alternative Pathways for Antigen Presentation
Even without traditional lymphatic vessels, the eyes aren’t cut off from the immune system. They have special ways to send antigens to lymph nodes. This is important for keeping the immune system in check and avoiding eye damage.
The meningeal lymphatic vessels help drain antigens from the central nervous system, including the eyes. They play a big role in clearing out harmful substances and guiding the immune response.
How This Limits Immune System Activation
The eyes’ lack of traditional lymphatic drainage means they don’t easily trigger a strong immune response. This helps avoid inflammation and damage to the eyes. This controlled immune response is vital for keeping vision clear.
The eye’s unique structure and its ability to suppress immune reactions also protect it. This balance between the eye’s anatomy and its immune environment is critical for eye health.
Immunosuppressive Factors in the Ocular Environment
The eye has special protection against the immune system. This protection is thanks to various immunosuppressive factors. These factors stop the immune system from harming the eye’s delicate tissues. This helps keep our vision clear.
Transforming Growth Factor-Beta (TGF-β) Mechanisms
Transforming Growth Factor-Beta (TGF-β) is key in the eye’s protection. It helps control the immune system and keeps the eye safe from harm.
TGF-β works in several ways to keep the immune system in check:
- It slows down T cell activity and growth.
- It stops the release of harmful cytokines.
- It helps create regulatory T cells.
This way, TGF-β prevents the immune system from attacking the eye.
Alpha-Melanocyte Stimulating Hormone and Other Neuropeptides
Alpha-melanocyte stimulating hormone (α-MSH) is another important protector in the eye. It has strong anti-inflammatory effects. This helps keep the eye’s immune system in balance.
α-MSH does several things to protect the eye:
- It reduces harmful cytokines.
- It stops immune cells from getting active.
- It boosts anti-inflammatory cytokines.
Other neuropeptides like vasoactive intestinal peptide (VIP) and calcitonin gene-related peptide (CGRP) also help control the immune response in the eye.
Fas Ligand Expression and Apoptosis Induction
Fas ligand (FasL) is found on some eye cells. It makes immune cells that have Fas on them die. This keeps harmful immune cells away from the eye.
FasL helps protect the eye by:
- Causing immune cells to die.
- Keeping the eye’s tissues safe.
- Stopping the immune system from overreacting.
Immunosuppressive Factor | Mechanism of Action | Effect on Immune Response |
TGF-β | Suppresses T cell activation, inhibits pro-inflammatory cytokines, promotes regulatory T cells | Prevents autoimmune reactions |
α-MSH | Suppresses pro-inflammatory cytokines, inhibits immune cell activation, promotes anti-inflammatory cytokines | Reduces inflammation and immune responses |
FasL | Induces apoptosis in Fas-bearing immune cells | Eliminates potentially damaging immune cells |
In summary, the eye has many immunosuppressive factors. These work together to protect the eye and keep our vision safe. Understanding these factors is key to treating eye diseases caused by the immune system.
When Protection Fails: Autoimmune Eye Diseases
When the immune system fails, autoimmune eye diseases can happen. These diseases threaten our vision and eye health. They occur when the immune system can’t tolerate eye tissues, leading to inflammation and damage.
These conditions show how delicate the balance is between immune protection and tolerance in the eyes. It’s important to understand these diseases to find effective treatments.
Experimental Autoimmune Uveitis as a Research Model
Experimental autoimmune uveitis (EAU) is a key research model for autoimmune eye diseases. It’s created in animal models to mimic human uveitis. This helps researchers study the immune system’s role in these diseases.
Studies on EAU have found important factors in autoimmune uveitis. They’ve shown that autoreactive T cells and certain cytokines play a big role. This knowledge helps us understand human autoimmune eye diseases better and find new treatments.
- Identification of autoreactive T cells as primary effectors
- Role of cytokines such as IFN-γ and IL-17 in disease progression
- Potential for therapeutic intervention at multiple stages of the immune response
Sympathetic Ophthalmia: When One Eye Affects the Other
Sympathetic ophthalmia is a rare but serious condition. It causes inflammation in one eye to spread to the other. This shows how some autoimmune eye diseases can affect the whole body.
The exact cause of sympathetic ophthalmia is not fully understood. But it’s thought to be an autoimmune response against eye tissues. Quick treatment is key to prevent vision loss in both eyes.
Key aspects of sympathetic ophthalmia include:
- Association with penetrating eye injuries or surgeries
- Bilateral granulomatous inflammation
- Importance of early diagnosis and aggressive immunosuppressive therapy
Vogt-Koyanagi-Harada Disease and Systemic Manifestations
Vogt-Koyanagi-Harada (VKH) disease is a multisystem autoimmune disorder. It mainly affects melanin-containing tissues, including the eyes. It’s characterized by bilateral uveitis and can also affect the nervous system and skin.
VKH disease shows how the immune system can affect different parts of the body. Managing VKH disease requires treating both the eyes and the rest of the body.
Treatment for VKH disease usually includes high-dose corticosteroids and immunosuppressive agents. These help control inflammation and prevent damage to tissues.
Common Eye Conditions With Immune Involvement
Immune dysregulation affects many eye conditions, impacting vision and quality of life. These conditions show how the immune system and eye health are connected.
Dry Eye Disease and Surface Inflammation
Dry eye disease is caused by inflammation on the eye’s surface. The immune system is key in its development, with inflammatory cytokines disrupting the tear film and damaging the cornea. It’s not just about not having enough tears, but also about immune processes.
Anti-inflammatory treatments are now a mainstay in managing dry eye disease. This shows how important it is to control the immune system in treating this condition.
Allergic Conjunctivitis Mechanisms
Allergic conjunctivitis is caused by allergens like pollen or dust mites. The release of histamine and other mediators from mast cells causes itching, redness, and swelling. Knowing how the immune system works in allergic conjunctivitis is key to finding effective treatments.
Treatments often aim to target the immune response with antihistamines or mast cell stabilizers. This shows how important it is to manage the immune system in treating this condition.
Age-Related Macular Degeneration and Complement Activation
Age-related macular degeneration (AMD) is a leading cause of vision loss in older adults. It has a significant immune component. Complement activation is involved in AMD, with certain genetic variants increasing the risk.
Research into AMD’s immune mechanisms has led to new treatments. This includes anti-complement therapies, showing promise for immune-targeted treatments.
Scleritis and Rheumatoid Arthritis Connection
Scleritis is a severe inflammatory eye disease linked to systemic autoimmune conditions like rheumatoid arthritis (RA). The immune system’s role in scleritis involves autoantibody production and immune complex deposition, causing inflammation and damage to the sclera.
The link between scleritis and RA highlights the need to consider systemic immune dysregulation. This is important in diagnosing and managing eye inflammatory conditions.
Diagnosing the Immune-Related Eye Disorders
Diagnosing immune-related eye disorders is complex. It involves looking at symptoms, warning signs, and using advanced tests. Getting the diagnosis right is key to treating the condition and saving vision.
Clinical Presentation and Warning Signs
Immune-related eye disorders show up in different ways. It’s important to know the signs. Symptoms like redness, pain, blurred vision, or sensitivity to light can point to problems like uveitis or scleritis.
Early signs might include floaters, flashes of light, or changes in how well you see. If you notice these, seeing a doctor quickly is important. Early treatment can make a big difference.
“The key to managing immune-related eye disorders lies in early detection and appropriate management, which can significantly improve patient outcomes and quality of life.”
Advanced Diagnostic Techniques
Modern tests are essential for diagnosing these disorders. They include:
- Optical Coherence Tomography (OCT): Gives detailed images of the retina and choroid, spotting structural changes.
- Fluorescein Angiography: Checks the health of retinal blood vessels, finding leaks or blockages.
- Ultrasonography: Helps see what’s going on in the back of the eye when it’s hard to see.
These tools, along with a detailed check-up and patient history, help doctors make the right diagnosis. This leads to a good treatment plan.
By using symptoms, warning signs, and modern tests, we can better diagnose and treat immune-related eye disorders. This improves care for patients.
Treatment Approaches for Immune-Mediated Eye Diseases
Managing immune-mediated eye diseases requires a detailed treatment plan. The right treatment depends on the disease, its severity, and the patient’s health.
Corticosteroids: Benefits and Limitations
Corticosteroids are key in treating immune-mediated eye diseases. They have strong anti-inflammatory effects. They can be applied topically, injected, or taken orally, based on the disease and its location.
They quickly reduce inflammation and prevent tissue damage. But, long-term use can cause side effects like cataracts, high eye pressure, and systemic issues.
Conventional Immunosuppressants and Antimetabolites
For long-term treatment or when corticosteroids don’t work, conventional immunosuppressants and antimetabolites are used. These include drugs like methotrexate, azathioprine, and cyclosporine.
These drugs suppress the immune system, reducing inflammation and stopping disease progression. It’s important to monitor for side effects like myelosuppression and increased infection risk.
Biologics and Targeted Molecular Therapies
Biologic agents are a newer treatment option. They target specific parts of the immune response. Examples include TNF-alpha inhibitors like infliximab and adalimumab, and other monoclonal antibodies.
Biologics offer targeted therapy with fewer side effects compared to traditional drugs. But, they are expensive and may raise the risk of infections.
Local vs. Systemic Treatment Considerations
Choosing between local and systemic treatment depends on the disease’s extent and severity. Local therapies, such as intravitreal injections or topical treatments, are preferred for their targeted action and reduced side effects.
Systemic treatments are needed for diseases with significant systemic involvement or when local therapies are not enough. The choice between local and systemic approaches balances effectiveness with the risk of adverse effects.
Treatment Approach | Benefits | Limitations |
Corticosteroids | Rapid anti-inflammatory effect | Potential for significant side effects with long-term use |
Conventional Immunosuppressants | Effective for long-term control | Risk of myelosuppression and infections |
Biologics | Targeted therapy with fewer systemic side effects | High cost and potentially increased risk of infections |
Conclusion
It’s important to understand how the immune system and eyes work together. This balance is key to keeping our vision clear. The eyes have a special protection called ocular immune privilege.
This protection helps keep the eyes safe from damage caused by the immune system. It’s a vital part of eye health.
We’ve looked at how the eyes keep their immune system in check. This includes the blood-retinal barrier and special factors that stop immune attacks. These work together to protect our vision.
Learning more about ocular immune privilege helps us understand how the immune system and eyes interact. This knowledge is important for finding new treatments for eye diseases. It also helps improve care for patients.
By understanding ocular immune privilege, we can better protect our vision. This knowledge helps us keep our eyes healthy and our vision clear.
FAQ
Does the immune system recognize the eyes?
Yes, the immune system knows about the eyes. It has ways to protect them from harm. The eyes and the immune system have a special relationship that keeps them safe.
What is ocular immune privilege?
Ocular immune privilege is a special protection for the eyes. It includes the blood-retinal barrier and other factors. These help keep the eyes safe from damage.
Can the immune system attack the eyes?
Yes, in some cases, the immune system can harm the eyes. This can lead to diseases like uveitis and Vogt-Koyanagi-Harada disease.
What happens if the immune system discovers the eyes?
The immune system already knows about the eyes. It protects them. But, if it gets out of balance, it can cause damage and vision loss.
How does the blood-retinal barrier regulate immune cell movement?
The blood-retinal barrier controls who gets into the eyes. It keeps out harmful cells and molecules. This helps prevent inflammation and damage.
What are immunosuppressive factors in the ocular environment?
Immunosuppressive factors in the eyes include TGF-β and alpha-melanocyte stimulating hormone. They help keep the eyes safe from the immune system.
Are there any common eye conditions that involve immune system dysregulation?
Yes, conditions like dry eye disease and age-related macular degeneration involve the immune system. They can be linked to diseases like rheumatoid arthritis.
How are immune-related eye disorders diagnosed?
Doctors use symptoms and advanced tests to diagnose these disorders. Early detection is key to preventing vision loss.
What are the treatment approaches for immune-mediated eye diseases?
Treatments include corticosteroids and biologics. The right treatment depends on the disease and the patient’s health.
Can the immune system be modulated to protect the eyes?
Yes, we can develop therapies to protect the eyes. Research is ongoing to understand how to keep the eyes safe from the immune system.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2945205/


