Last Updated on November 27, 2025 by Saadet Demir
Edema Papillare Papilledema Guide: Key Facts, Causes, and Treatment
Edema papillare, also known as papilledema, is a serious medical condition. It causes swelling of the optic disc due to high intracranial pressure. We know how important it is to act fast to avoid losing vision forever. Learn about edema papillare (papilledema). This guide provides 5 key facts, explains the causes, and management options.
At Liv Hospital, we focus on our patients and use the latest medical knowledge. We work together to check and treat papilledema well. Our team is dedicated to giving top-notch care to patients from around the world.
It’s key to know what causes and how to manage edema papillare. We’ll look at five important facts about it. This will help us understand it better.

Key Takeaways
- Papilledema is a serious medical condition requiring immediate attention.
- Elevated intracranial pressure is the primary cause of optic disc swelling.
- Prompt evaluation and treatment can prevent permanent vision loss.
- A complete team effort is needed for effective management.
- Liv Hospital is committed to delivering world-class healthcare for international patients.
Understanding Papilledema: Definition and Medical Significance
Papilledema is a condition where the optic disc swells. It’s a sign of high pressure inside the skull. We’ll look into what it means, its terms, and why it’s so serious.
Clinical Definition and Terminology
Papilledema is when the optic disc swells because of high pressure in the skull. This happens when pressure goes through the optic nerve sheath to the space around the brain. It makes the optic nerve fibers swell and push forward.
Doctors call it papilledema when swelling is because of high skull pressure. It’s not just swelling of the optic disc. It’s swelling because of high pressure.
The Serious Nature of Optic Disc Swelling
Papilledema is a big worry because it can mean serious problems like brain tumors or cerebral venous thrombosis. Finding and treating the cause quickly is key to avoid vision loss.
“Papilledema is a red flag for potentially life-threatening conditions, and its presence necessitates a thorough investigation into its cause.”
Optic disc swelling is very serious. It means we need to act fast and check the patient well. This is to give the best care possible.
Condition | Characteristics | Clinical Significance |
Papilledema | Swelling of the optic disc due to increased ICP | Indicator of potentially life-threatening conditions |
Optic Disc Edema | Swelling of the optic disc from various causes | May or may not be related to ICP |
The Pathophysiology Behind Edema Papillare
Edema papillare’s pathophysiology is complex. It involves the relationship between intracranial pressure and optic nerve function. Knowing this is key to diagnosing and treating the condition.
Mechanism of Optic Nerve Fiber Engorgement
Intracranial pressure increases and affects the optic nerve sheath. This causes the optic nerve fibers to swell. This swelling blocks the flow of axoplasm in the ganglion cell axons, leading to swelling of the optic disc.
Key factors contributing to optic nerve fiber engorgement include:
- Increased intracranial pressure
- Transmission of pressure to the optic nerve sheath
- Impaired axoplasmic transport
Transmission of Intracranial Pressure
Intracranial pressure is transmitted to the optic nerve, a key part of edema papillare. This pressure moves through the subarachnoid space around the optic nerve.
“The optic nerve is surrounded by a subarachnoid space that is continuous with the intracranial subarachnoid space, allowing for the transmission of intracranial pressure.”
The Subarachnoid Space Connection
The subarachnoid space is vital in edema papillare’s pathophysiology. It connects the intracranial space to the space around the optic nerve. This connection allows pressure to be transmitted, leading to edema papillare.
Pathophysiological Mechanism | Description |
Optic Nerve Fiber Engorgement | Engorgement of optic nerve fibers due to increased intracranial pressure |
Transmission of Intracranial Pressure | Pressure transmission through the subarachnoid space to the optic nerve |
Subarachnoid Space Connection | Connection between intracranial and optic nerve subarachnoid spaces facilitating pressure transmission |
Key Fact #1: Bilateral Presentation and Development Timeline
It’s important to know about the bilateral nature and timeline of edema papillare. This helps in diagnosing and managing it well. We’ll look at why it’s often seen in both eyes, how it progresses, and what affects its development.
Why Edema Papillare is Nearly Always Bilateral
Edema papillare, or papilledema, is swelling of the optic disc due to high pressure inside the skull. It’s nearly always bilateral, affecting both eyes. This is because the optic nerve sheaths and the skull space communicate, allowing pressure to spread to both nerves.
Progression Timeline: Hours to Weeks
The timeline for edema papillare can vary, from hours to weeks. It depends on how fast the pressure inside the skull goes up. Quick increases, like with brain injuries or sudden bleeding, can cause it to develop fast. Slow increases, like with tumors, may take longer.
Factors Affecting Development Rate
Several things can change how fast edema papillare develops. These include the underlying cause of the pressure, how fast the pressure goes up, and the anatomy of the optic nerve sheath. Knowing these helps doctors predict how it will progress and plan the best treatment.
Key Fact #2: Common Causes of Edema Papillare
It’s important to know what causes edema papillare to treat it well. This condition makes the optic disc swell. It often happens when there’s too much pressure inside the skull.
Brain Tumors and Space-Occupying Lesions
Brain tumors and other growths in the brain can cause edema papillare. These growths take up space in the skull, raising pressure. As they grow, they can push on the brain, causing swelling.
It’s key to find and treat these growths quickly to avoid more problems.
Intracranial Hemorrhages
Bleeding in the brain can also lead to edema papillare. This bleeding can quickly raise pressure inside the skull. The size and place of the bleed affect how bad the swelling will be.
Meningitis and Other Infections
Infections like meningitis can cause inflammation and high pressure in the brain. This can swell the optic disc. It’s important to treat these infections fast to avoid lasting brain damage.
Cerebral Venous Thrombosis
A blood clot in the brain’s veins can block blood flow and raise pressure. This can cause swelling in the optic disc. Doctors need to be careful and use imaging to diagnose this condition.
Other issues like hydrocephalus and idiopathic intracranial hypertension can also cause edema papillare. Knowing all these causes helps doctors take better care of patients.
Key Fact #3: Epidemiology and Risk Factors
Epidemiological studies have shed light on the risk factors associated with edema papillare. Understanding this condition is key to identifying at-risk populations and developing targeted interventions.
General Population Incidence
The incidence of papilledema in the general population is relatively low. Studies show that in the U.S., it affects about 0.9 per 100,000 people. But, this rate can change based on the population studied.
Increased Risk in Women with Obesity
Obesity, mainly in women of childbearing age, is a significant risk factor for edema papillare. Women aged 20 to 44 with overweight or obesity face a higher risk, at 13 per 100,000. This highlights the need to monitor and manage obesity to prevent this condition.
Age and Gender Distribution
The distribution of edema papillare varies by age and gender. It’s most common in women of childbearing age, suggesting a link to hormonal factors. Knowing these patterns helps clinicians identify patients at higher risk.
Other Contributing Risk Factors
Other factors also increase the risk of developing edema papillare. These include conditions that raise intracranial pressure, like cerebral venous thrombosis and meningitis. Understanding these risk factors is vital for early diagnosis and effective management.
Risk Factor | Incidence Rate | Population |
General Population | 0.9 per 100,000 | U.S. Population |
Obesity in Women (20-44 years) | 13 per 100,000 | Women aged 20-44 with overweight or obesity |
By grasping these epidemiological trends and risk factors, healthcare providers can better spot individuals at risk for edema papillare. They can then use the right preventive and therapeutic strategies.
Key Fact #4: Visual Function and Disease Progression
It’s important to know how edema papillare affects your vision. This condition causes swelling in the optic disc. It can harm your eye health and vision quality.
Initial Preservation of Visual Acuity
At first, people with edema papillare might not see any big changes. Their vision might seem fine. But, this doesn’t mean the problem is not serious or won’t get worse.
Warning Signs of Visual Deterioration
As edema papillare gets worse, you might notice some signs. These include vision that gets dim or blurry for a short time. You might also see blind spots in your field of vision. It’s important to watch for these signs to catch problems early.
Mechanisms of Permanent Vision Loss
Long-term vision loss can happen in edema papillare. This is because high pressure in the brain can damage the optic nerve. This damage comes from problems with how cells move and get oxygen. Knowing how this works helps doctors find better treatments.
Timeline of Visual Changes
How fast vision changes in edema papillare can differ for everyone. Things like the cause of the condition and how fast pressure builds up play a role. Seeing a doctor regularly and acting fast is important to avoid losing your sight forever.
Even if your vision seems okay at first, ignoring edema papillare can lead to permanent vision loss. You might start to notice blind spots or see double. High pressure in the brain can also cause double vision. So, it’s key to watch for these signs and get help right away.
Key Fact #5: Diagnostic Approaches
To accurately diagnose edema papillare, healthcare professionals use various methods. The diagnostic process is key to finding the cause and choosing the right treatment.
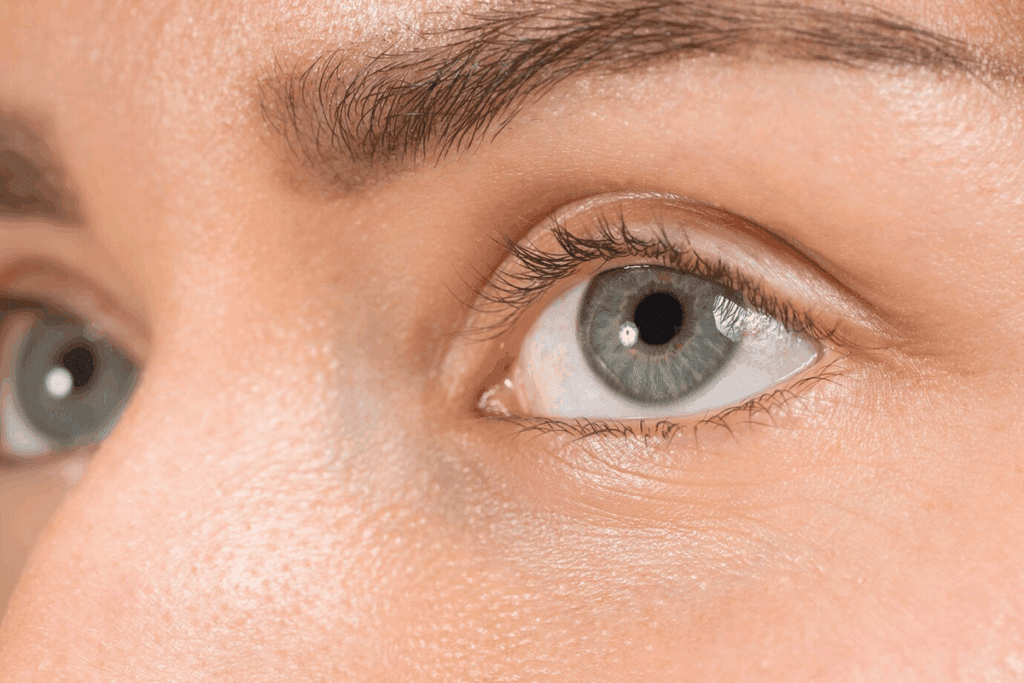
Ophthalmoscopic Examination
The first step is an ophthalmoscopic examination. This lets doctors see the optic disc and check for swelling. It helps them understand the optic nerve’s condition.
Neuroimaging Techniques
Neuroimaging techniques like MRI and MRV are important. They help find the cause of edema papillare. These tools spot lesions and other issues that might be causing symptoms.
- MRI (Magnetic Resonance Imaging) shows detailed brain and orbit images.
- MRV (Magnetic Resonance Venography) is great for finding cerebral venous thrombosis.
Lumbar Puncture and CSF Pressure Measurement
A lumbar puncture measures cerebrospinal fluid (CSF) pressure. It’s often high in edema papillare patients. This test helps diagnose and understand the condition’s cause.
Visual Field Testing
Visual field testing checks how edema papillare affects vision. It spots blind spots or sensitivity loss. This helps doctors know how severe it is and what treatment to use.
Using these methods, doctors get a full picture of edema papillare. This lets them manage it effectively for each patient.
Clinical Presentation and Symptoms
Edema papillare shows different symptoms in patients. This makes it hard to diagnose and treat. Each person may have a unique set of symptoms.
Headache Characteristics
Headaches are a common symptom. They often get worse in the morning and can be triggered by position. These headaches can be severe and are a significant source of discomfort for patients. They happen because of increased pressure inside the skull.
Visual Disturbances
Visual disturbances are also a big part of edema papillare. Patients might see temporary vision loss or blurred vision. These visual disturbances can significantly impact a patient’s quality of life.
Associated Neurological Symptoms
Patients may also have other symptoms like nausea and vomiting. These symptoms are linked to the cause of edema papillare, like increased pressure in the skull.
Asymptomatic Presentation Possibilities
Some patients with edema papillare may not show symptoms at first. It’s important to get regular eye exams to catch it early.
Watch for these symptoms:
- Headaches that worsen in the morning
- Transient visual obscurations
- Blurred vision
- Nausea and vomiting
Differential Diagnosis of Edema Papillare
To correctly diagnose Edema Papillare, we must look at other reasons for optic disc swelling. Finding the right diagnosis is key for treating patients with suspected Edema Papillare. Many conditions can look like Edema Papillare, making diagnosis tricky.
Pseudopapilledema
Pseudopapilledema looks like optic disc swelling but isn’t real. It can happen due to optic disc drusen or being very nearsighted. Accurate diagnosis is vital to tell pseudopapilledema apart from true Edema Papillare.
- Optic disc drusen
- Hyperopia
- Other conditions that may cause pseudopapilledema
Optic Neuritis
Optic neuritis is an inflammation of the optic nerve. It can cause vision loss and swelling of the optic disc. While it shares some symptoms with Edema Papillare, the causes and treatments are different. Prompt diagnosis is key to avoid permanent vision loss.
Anterior Ischemic Optic Neuropathy
Anterior ischemic optic neuropathy (AION) happens when blood flow to the optic nerve stops suddenly. This leads to swelling of the optic disc and vision loss. AION can be caused by either blood vessel problems or other reasons, each needing different treatments.
- Arteritic AION
- Non-arteritic AION
Diagnostic Challenges and Pitfalls
Diagnosing Edema Papillare and differentiating it from other conditions is hard. Common mistakes include misreading tests or missing other causes of optic disc swelling. Careful clinical evaluation and the right diagnostic tools are critical.
Grading Systems and Classification
Healthcare professionals use grading systems like the Frisen Scale to understand edema papillare’s severity. These systems help assess the condition’s impact and guide treatment.
The Frisen Scale
The Frisen Scale is a key grading system for papilledema. It grades papilledema from 0 to 5. Each grade has specific criteria, helping doctors track changes accurately.
Key features of the Frisen Scale include:
- Grade 0: Normal optic disc
- Grade 1: Minimal blurring of the nasal margin
- Grade 2: Moderate blurring of the margins
- Grade 3: Obscuration of the margins
- Grade 4: Elevation of the entire optic disc
- Grade 5: Severe papilledema with dome-shaped morphology
Modified Frisen Scale
Some doctors use a modified Frisen Scale. This version includes more criteria or detailed descriptions of optic disc changes. It allows for a more precise assessment of papilledema severity.
Clinical Significance of Grading
Grading papilledema with the Frisen Scale or its modifications is very important. It helps track disease progression and treatment response. Accurate grading is key to effective management.
Documentation Standards
Following documentation standards is essential when using grading systems like the Frisen Scale. Clear and consistent documentation ensures all healthcare providers are informed about the condition’s severity and any changes.
Best practices for documentation include:
- Using a standardized grading system
- Recording the grade at each examination
- Noting any changes or progression
- Including relevant clinical findings and symptoms
Management Strategies and Treatment Options
Managing edema papillare needs a full plan that tackles the root causes and relieves symptoms. We will look at the different ways to manage this condition.
Addressing Underlying Causes
The first step is to find and treat the cause. This could be a brain tumor, cerebral venous thrombosis, or idiopathic intracranial hypertension. Treating the cause is key to lowering pressure in the brain and easing symptoms.
- Brain tumors might need surgery or radiation.
- Cerebral venous thrombosis is treated with blood thinners.
- Idiopathic intracranial hypertension uses drugs to lower pressure.
Medical Management
Medical care is vital in lowering brain pressure and managing symptoms. Acetazolamide is a common drug that helps by reducing fluid in the brain.
Other medical strategies include:
- Keeping an eye on symptoms like headaches and vision problems.
- Using corticosteroids to reduce swelling.
- Changing lifestyle, like losing weight, for obese patients.
Surgical Interventions
Surgery is sometimes needed to manage edema papillare. Surgical options include:
- Optic nerve sheath fenestration to ease pressure on the optic nerve.
- Ventriculoperitoneal shunting to lower pressure by moving fluid.
- Removing or shrinking tumors when they cause the problem.
Monitoring Protocols
Regular checks are key to adjusting treatment. This includes:
- Eye exams to watch for swelling.
- Brain scans to track the cause.
- Lumbar punctures to measure pressure.
With a detailed management plan, we can lower brain pressure, ease symptoms, and help patients get better.
Complications and Long-term Prognosis
It’s important to know the complications and long-term outlook of edema papillare. If not treated, it can cause permanent vision loss. This happens because of high pressure inside the brain that damages the nerve layer.
This condition makes vision worse over time. It affects both the field of vision and central vision. We need to understand these factors to give the best care.
Potential Complications if Left Untreated
Not treating edema papillare can lead to severe vision loss. The high pressure can harm the optic nerve. This can cause:
- Permanent visual field defects
- Impairment of central visual acuity
- In some cases, complete blindness
So, it’s key to catch and treat it early to avoid these problems.
Prognosis Based on Etiology
The outlook for edema papillare depends on why it happens. For example:
- People with IIH might have a different outcome than those with tumors.
- Treating the cause well is important for a good outcome.
Knowing the cause helps us plan the best treatment and guess the outcome.
Quality of Life Considerations
Edema papillare can really affect a person’s life, mainly if it hurts their vision. We should think about:
- Helping patients adjust to vision loss
- Supporting them emotionally
- Changing their lifestyle to fit their new vision
By focusing on these areas, we can make life better for those with edema papillare.
Recurrence Rates and Prevention
How often edema papillare comes back depends on the cause and the first treatment. To prevent it, we can:
- Watch the brain pressure in at-risk patients
- Manage conditions like IIH or blood clots in the brain
- See doctors regularly to catch any signs of coming back early
Using these methods can lower the chance of it coming back and help long-term results.
Conclusion
We’ve looked into edema papillare, a condition where the optic disc swells due to high pressure inside the skull. It’s important to manage this condition well to avoid losing vision and to help patients get better.
Healthcare providers need to know about the causes, signs, and how to treat edema papillare. By fixing the root cause, using the right treatments, and keeping a close eye on the patient, we can avoid serious problems. This helps patients live better lives.
Handling papilledema needs a full plan, from quick diagnosis to the right treatment and constant checks. This way, we can lower the chance of vision loss and better the lives of those with edema papillare.
FAQ
What is edema papillare?
Edema papillare, also known as papilledema, is a condition. It causes the optic disc to swell. This happens because of increased pressure inside the skull.
What are the common causes of edema papillare?
Common causes include brain tumors and intracranial hemorrhages. Meningitis, cerebral venous thrombosis, and other conditions also lead to increased pressure.
Is edema papillare always bilateral?
Yes, edema papillare is nearly always bilateral. It affects both eyes, though the severity can differ.
How is edema papillare diagnosed?
Diagnosis involves an ophthalmoscopic examination. Neuroimaging techniques like MRI and MRV are also used. A lumbar puncture to measure CSF pressure and visual field testing are part of the diagnosis.
What are the symptoms of edema papillare?
Symptoms include headaches and visual disturbances. These can be transient visual obscurations. Some cases may have no symptoms at all.
How is the severity of edema papillare graded?
The Frisen Scale grades the severity from 0 to 5. It is based on specific ophthalmoscopic features.
What is the management strategy for edema papillare?
Management involves treating the underlying cause. Medical management with medications like acetazolamide is used. Surgical interventions may be necessary. Monitoring protocols are also part of the management.
What are the potentially severe complications of untreated edema papillare?
Untreated edema papillare can lead to severe vision loss. This can be permanent. Timely diagnosis and treatment are critical.
Can edema papillare recur?
Yes, recurrence is possible. Understanding the cause and implementing preventive strategies are key for long-term management.
How does edema papillare affect visual function?
Initially, visual acuity may be preserved. But, if left untreated, it can lead to permanent vision loss. Early intervention is essential.