Epiretinal ERM pucker, also known as macular pucker, is a condition. It forms a thin layer of scar tissue on the macula. This causes vision to become distorted and blurry. What is a macular membrane pucker? This ultimate guide explains what an epiretinal membrane is and how to treat it.
About 2% of people aged 50 and up get this condition. But, 20% of those aged 75 and older are affected. Both men and women are equally likely to get epiretinal ERM pucker.
At Liv Hospital, we know how vital clear vision is. We offer detailed evaluations and tailored treatment plans for epiretinal ERM.
Key Takeaways
- Epiretinal ERM pucker affects vision by causing distortion and blurring.
- The condition is more prevalent among individuals aged 50 and above.
- Both men and women are equally affected by epiretinal ERM pucker.
- Comprehensive evaluation is key for finding the best treatment.
- Personalized treatment strategies can help keep central vision clear.
Understanding Epiretinal Membrane Pucker
It’s important to understand epiretinal membrane pucker to diagnose and treat it. This eye condition, also known as macular pucker, forms a fibrous layer on the retina. It can cause vision problems.
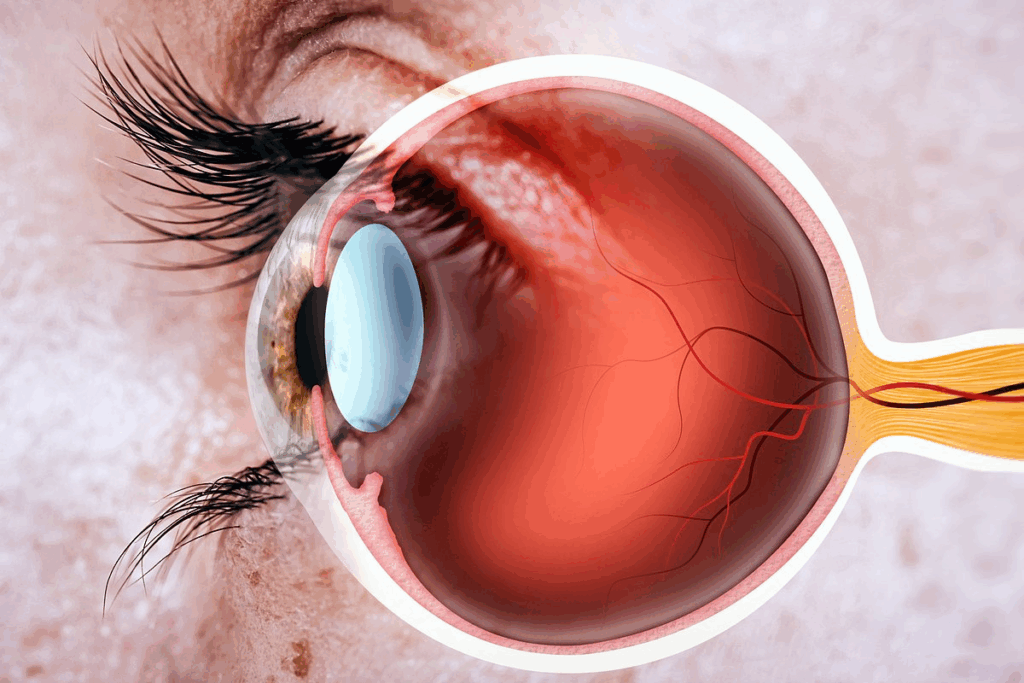
Definition and Pathophysiology
An epiretinal membrane (ERM) is a fibrocellular layer on the retina’s inner surface. It often happens with posterior vitreous detachment. This membrane can contract, making the retina wrinkle and causing vision distortion.
The process involves cells growing and forming membranes. Idiopathic epiretinal membrane is the most common type, making up about 95% of cases.
Prevalence and Demographics
Epiretinal membrane pucker affects about 2% of people over 50. By 75, this number jumps to 20%. Both men and women are equally likely to get it.
It gets more common with age. This makes regular eye checks very important for older adults. Risk factors include aging, posterior vitreous detachment, and some retinal diseases.
Natural History of the Condition
The way epiretinal membrane pucker progresses varies. Some people may not notice any symptoms. Others might see their vision get worse over time.
- Stable condition with minimal symptoms
- Gradual progression of visual distortion
- Potential for spontaneous improvement in some cases
Regular eye exams are key to managing symptoms. They help decide if treatment is needed.
Causes and Risk Factors of Macular Membrane Pucker

The causes of macular membrane pucker are complex. They include idiopathic, secondary, genetic, and environmental factors. Knowing these causes helps in diagnosing and treating the condition.
Idiopathic Epiretinal Membrane
Idiopathic epiretinal membrane is the most common type of macular membrane pucker. It makes up about 95 percent of cases. It often happens with posterior vitreous detachment (PVD), where the vitreous gel separates from the retina.
The exact reason for idiopathic epiretinal membrane is not known. But, it’s thought to be caused by the growth of fibrocellular material on the retina.
Key characteristics of idiopathic epiretinal membrane include:
- Association with aging and posterior vitreous detachment
- Presence of fibrocellular proliferation on the retinal surface
- Potential for causing visual distortion and blurring
Secondary Causes
While most cases of macular membrane pucker are idiopathic, secondary causes also play a role. These include:
- Diabetic retinopathy
- Retinal vascular diseases
- Ocular trauma
- Previous retinal surgery or laser photocoagulation
- Inflammatory conditions such as uveitis
These secondary causes can lead to epiretinal membranes through inflammation, retinal ischemia, and mechanical stress.
Genetic and Environmental Factors
Research is ongoing to understand the genetic and environmental factors of macular membrane pucker. There is no clear genetic link. But, certain environmental factors may contribute to the condition.
Potential environmental risk factors include:
- Aging
- Exposure to certain ocular conditions or diseases
- Previous ocular surgery or trauma
More studies are needed to understand how genetic and environmental factors interact in macular membrane pucker.
Recognizing Symptoms of Epiretinal Pucker
It’s important to know the signs of epiretinal pucker early. This helps in getting the right treatment and stopping vision loss. We’ll look at the common symptoms and how they affect daily life.
Visual Distortion (Metamorphopsia)
Visual distortion, or metamorphopsia, is a key sign. It makes straight lines look wavy. For example, text in a book might seem distorted, making it hard to read.
Central Vision Blurring
Central vision blurring is another big symptom. It can make it tough to do things that need clear vision, like reading, driving, or seeing faces.
Symptom Progression Timeline
How fast symptoms get worse can vary. Some people see their vision slowly get worse over time. Others might see a quicker drop. Knowing how symptoms progress helps in planning treatment.
Impact on Daily Functioning
Symptoms of epiretinal pucker can really affect daily life. Simple tasks like reading, cooking, or watching TV can become hard. Here are some common problems:
- It’s hard to read or do tasks that need clear vision.
- Driving or going up stairs can be tough because of distorted vision.
- Doing everyday things like cooking or using digital devices can be a struggle.
Understanding these symptoms and their effects helps people get the right medical help. This way, they can manage their condition better.
Diagnostic Procedures and Evaluation
To diagnose epiretinal membrane pucker, we use many ophthalmic tools. It’s key to know how severe it is to choose the right treatment.
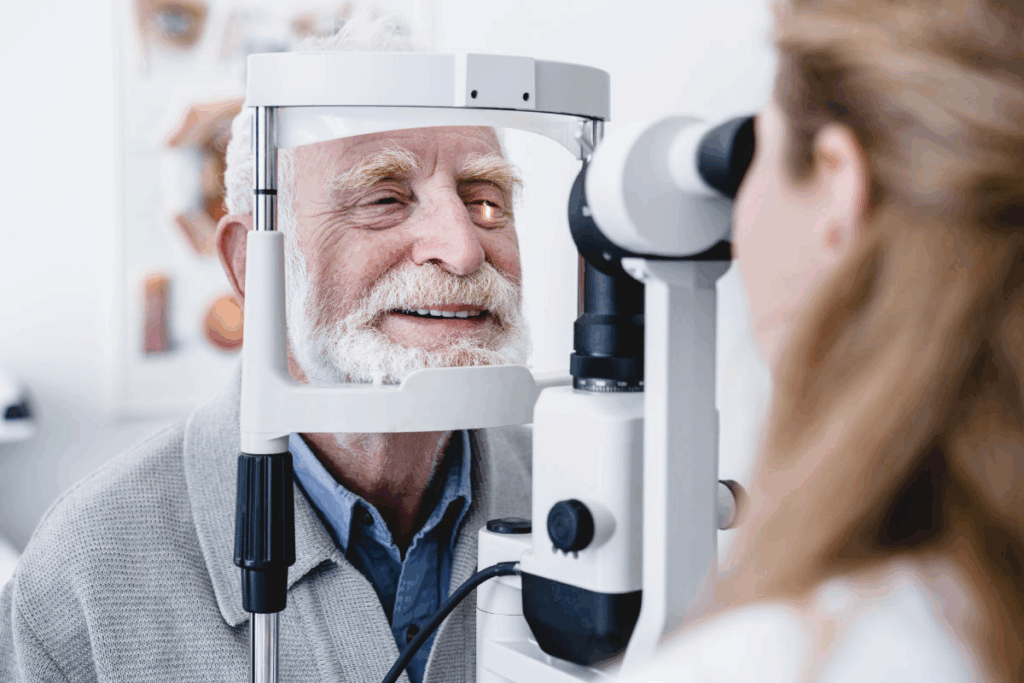
Comprehensive Eye Examination
First, we do a full eye check. This includes talking about your health, checking how well you see, and looking closely at your retina and macula. Visual acuity testing shows how much the condition affects your vision.
Optical Coherence Tomography (OCT)
Optical Coherence Tomography (OCT) is a test that shows the retina’s details without hurting you. It’s vital for spotting epiretinal membrane pucker. It lets us see the retinal layers and any membranes or distortions.
Fluorescein Angiography
Fluorescein angiography helps us see the retina’s blood vessels. It checks for leaks or lack of blood flow linked to epiretinal membrane pucker. We inject a dye that makes the blood vessels glow.
Amsler Grid Testing
Amsler grid testing is a simple way to find vision problems from epiretinal membrane pucker. You look at a grid with a dot in the middle and tell us if you see any oddities. It helps us see how it affects your central vision.
By using these tests together, we can accurately find out if you have epiretinal membrane pucker. This helps us decide the best way to treat it.
Severity Classification of Macular Membrane Pucker
It’s key for eye doctors to know how serious macular membrane pucker is. They use many factors to figure out its severity.
Grading Systems
There are different ways to measure how bad macular membrane pucker is. These methods look at the size and thickness of the membrane. They also check how much the retina is distorted.
- Membrane Size and Thickness: Bigger and thicker membranes usually mean worse symptoms.
- Retinal Distortion: How much the retina is bent and if there are folds or detachments matters a lot.
Visual Acuity Measurements
Measuring how well you can see is very important. It shows how much macular membrane pucker affects your vision.
Visual acuity tests show how much central vision loss and distortion there is. This helps doctors decide the best treatment.
Anatomical Considerations
Changes in the retina, like cystoid macular edema or thickening, also play a big role. These changes help doctors understand how serious the condition is.
Functional Impact Assessment
It’s important to see how macular membrane pucker affects daily life. Doctors look at how it makes tasks like reading, driving, and recognizing faces hard.
“Accurate classification of macular membrane pucker severity is critical for determining the most appropriate treatment strategy and improving patient outcomes.”
— Expert Opinion
Doctors use all these factors to understand how serious the condition is. Then, they can make treatment plans that fit each patient’s needs.
Conservative Management Strategies
Epiretinal membrane pucker can often be managed without surgery. We focus on observation, rehabilitation, and using adaptive measures. This is best for patients with mild symptoms or those not ready for surgery.
Observation Protocols
Watching the condition closely is key in managing epiretinal membrane pucker. Regular eye exams help us see if surgery is needed. We suggest eye exams every 6 to 12 months, including:
- Visual acuity testing
- Optical Coherence Tomography (OCT) imaging
- Amsler grid testing
These tests help us understand how the condition affects vision. They also help us spot any changes that might need a different approach.
Visual Rehabilitation Techniques
Helping patients adapt to vision changes is important. Techniques include:
- Eccentric viewing training
- Visual therapy to improve eye movement and coordination
- Low vision aids to enhance remaining vision
These methods can make a big difference. They help patients do daily tasks better and stay independent.
Adaptive Devices and Tools
Adaptive devices and tools also help patients cope with symptoms. Examples include:
Device/Tool | Purpose |
Magnifying glasses | Enhance near vision |
Large print materials | Facilitate reading |
Smartphone apps for low vision | Provide assistive technology for daily tasks |
These tools can greatly improve life for those with epiretinal membrane pucker.
Monitoring Disease Progression
Keeping a close eye on the condition is vital. We use clinical assessments and imaging to track changes. This helps us decide when surgery might be needed.
By using a detailed conservative management plan, we can help patients with epiretinal membrane pucker. This improves their vision and overall quality of life.
Surgical Treatment Options
For those with severe epiretinal membrane pucker, surgery can help restore vision. It’s considered when symptoms greatly affect daily life and other treatments don’t work.
Vitrectomy Procedure
The main surgery for epiretinal membrane pucker is pars plana vitrectomy. We remove the vitreous gel to reach the retina. Then, we carefully take out the membrane with fine tools. The surgery is done under local anesthesia to reduce pain.
We use vitreoretinal surgical instruments to avoid harming the eye. These tools help us work precisely inside the eye, making the surgery safer and more effective.
Membrane Peeling Techniques
Membrane peeling is key in treating epiretinal membrane pucker. We use special dyes to highlight the membrane during surgery. This helps us remove it fully and safely.
We then carefully peel the membrane off the retina with microforceps. This step needs great care to avoid retinal tears or other issues.
Surgical Instruments and Technology
New tools and technologies have improved vitreoretinal surgery. High-resolution imaging systems and precise instruments help us remove the membrane safely.
Intraoperative OCT is also used more often. It allows us to see the retina in real-time during surgery. This helps confirm the membrane’s removal and checks the retina’s condition.
Patient Selection Criteria for Surgery
Choosing the right patients for surgery is important. We look at how much symptoms affect daily life and if other eye problems exist. Those with severe vision problems or worsening conditions are usually good candidates.
We do a thorough check before surgery to see if the eye is healthy enough. This includes a detailed eye exam and imaging to understand the extent of the problem.
Post-Surgical Recovery and Rehabilitation
After surgery, it’s important to follow a recovery plan. This plan includes rest, physical therapy, and taking medicine as directed. It also means avoiding activities that could harm the eye.
Recovery time varies based on the surgery type and the patient’s health. It’s key to stick to the doctor’s advice to ensure a smooth healing process. This helps avoid complications and ensures the best possible outcome.
Rehabilitation is a big part of the recovery. It includes exercises and therapy to help the eye heal and regain strength. These steps are vital for a full recovery and to prevent future problems.
Managing medicine is also a big part of recovery. It’s important to take all prescribed medications as directed. This helps control pain, prevent infection, and supports healing.
Visual recovery is another important aspect. It involves regaining clear vision and adjusting to any changes in vision. This can take time and patience, but it’s essential for a full recovery.
Overall, post-surgical recovery and rehabilitation are critical for a successful outcome. By following the doctor’s advice, managing medicine, and participating in rehabilitation, patients can ensure a smooth and effective recovery.
Complications and Management
Surgery for epiretinal membrane pucker helps but comes with risks. Knowing these risks is key for good care and management.
Surgical Complications
Operations for epiretinal membrane pucker can cause problems like retinal detachment, cataracts, and endophthalmitis. Retinal detachment is a serious issue that needs quick action. We do our best to avoid these problems, but it’s important for patients to know they can happen.
A detailed study on the risks of vitreoretinal surgery shows the need for careful surgery and aftercare. Below is a table of common complications and how to handle them.
Complication | Management Strategy |
Retinal Detachment | Immediate surgical intervention, vitreoretinal surgery |
Cataract Formation | Cataract surgery when necessary |
Endophthalmitis | Intravitreal antibiotics, vitreous tap |
Recurrence Rates and Risk Factors
Epiretinal membrane pucker can come back after surgery, with varying rates. Risk factors include not removing all of the membrane and pre-existing eye conditions. We check each patient to see who might be at higher risk.
Managing Persistent Symptoms
Some patients may keep feeling symptoms like visual distortion or blurring after surgery. Managing these symptoms often involves visual therapy and special devices. We help patients create a plan that meets their needs.
Secondary Interventions
If symptoms or recurrence happen, we might need to do more surgery or treatments. We talk to patients about these options and what they mean.
Knowing about possible complications and having a plan helps us give the best care for patients with epiretinal membrane pucker.
Conclusion: Prognosis and Future Directions
The outlook for people with epiretinal membrane pucker is good. This is thanks to better vitrectomy and macular pucker surgeries. About 80-90% of patients see their vision improve and distortions lessen after surgery.
Looking ahead, we’re working on making surgeries even better. We’re also exploring new technologies to help patients more. Our goal is to make treatments more effective and reduce the chance of problems coming back.
As we learn more about epiretinal membrane pucker, we’ll get better at diagnosing and treating it. This means doctors will have more effective ways to help patients. Patients will likely see better results from their surgeries and treatments.
FAQ
What is epiretinal membrane pucker?
Epiretinal membrane pucker, also known as macular pucker, is a condition. It happens when a layer of fibrous tissue forms on the retina’s surface. This causes visual distortion and blurred vision.
What are the symptoms of epiretinal membrane pucker?
Symptoms include visual distortion, where straight lines appear wavy or bent. Blurred central vision also affects daily functioning.
How is epiretinal membrane pucker diagnosed?
A detailed eye examination is needed. This includes a dilated eye exam and imaging like Optical Coherence Tomography (OCT).
What are the treatment options for epiretinal membrane pucker?
Treatment options include watching it closely or surgery. Surgery involves removing the vitreous gel and the membrane.
What is the vitrectomy procedure for epiretinal membrane pucker?
The vitrectomy procedure removes the vitreous gel and the membrane. This allows the surgeon to access the retina and improve vision.
What is the recovery process after surgery for epiretinal membrane pucker?
Recovery involves immediate care, activity limits, and medication. The time it takes to see improvement varies.
What are the possible complications of surgical treatment for epiretinal membrane pucker?
Possible complications include surgical issues, recurrence, and persistent symptoms. These can be managed with further treatments.
Can epiretinal membrane pucker recur after surgery?
Yes, it can recur after surgery. The rate of recurrence varies based on individual factors.
How effective is surgery in improving vision for epiretinal membrane pucker?
Surgery improves vision in 80-90% of patients. It reduces visual distortions significantly.
What is the natural progression of epiretinal membrane pucker?
Its progression varies. Some cases stay the same, while others worsen, causing more visual distortion.
Are there any risk factors for developing epiretinal membrane pucker?
Yes, age is a risk factor, more common in those over 50. Posterior vitreous detachment also increases the risk.
Can epiretinal membrane pucker be managed conservatively?
Yes, mild cases can be managed without surgery. This includes watching it closely and using visual aids.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK560703/