Pelvic organ prolapse is a common issue, affecting up to 50 percent of women who have given birth. Most of these women seek help after they turn 60. For elderly women experiencing discomfort and life-altering symptoms, finding effective treatment is key. It helps them regain their quality of life and independence. Management options for uterine prolapse treatment for elderly women, focusing on non-surgical and minimally invasive care.
At Liv Hospital, we use top-notch protocols and focus on the patient to manage prolapse in elderly women. We combine clinical skill with caring healthcare. We will explore the treatment options available, including both nonsurgical and surgical methods. This will help you understand how to manage uterine prolapse effectively.
Key Takeaways
- Pelvic organ prolapse affects up to 50 percent of parous women.
- Elderly women above 60 years represent the majority seeking treatment.
- Effective management is key to restore quality of life.
- Liv Hospital offers international-standard protocols and patient-centered care.
- Treatment options include nonsurgical and surgical methods.
Understanding Uterine Prolapse in Elderly Women

Elderly women face a higher risk of uterine prolapse. This condition happens when muscles and tissues weaken with age. It can make daily life hard, causing pain and discomfort.
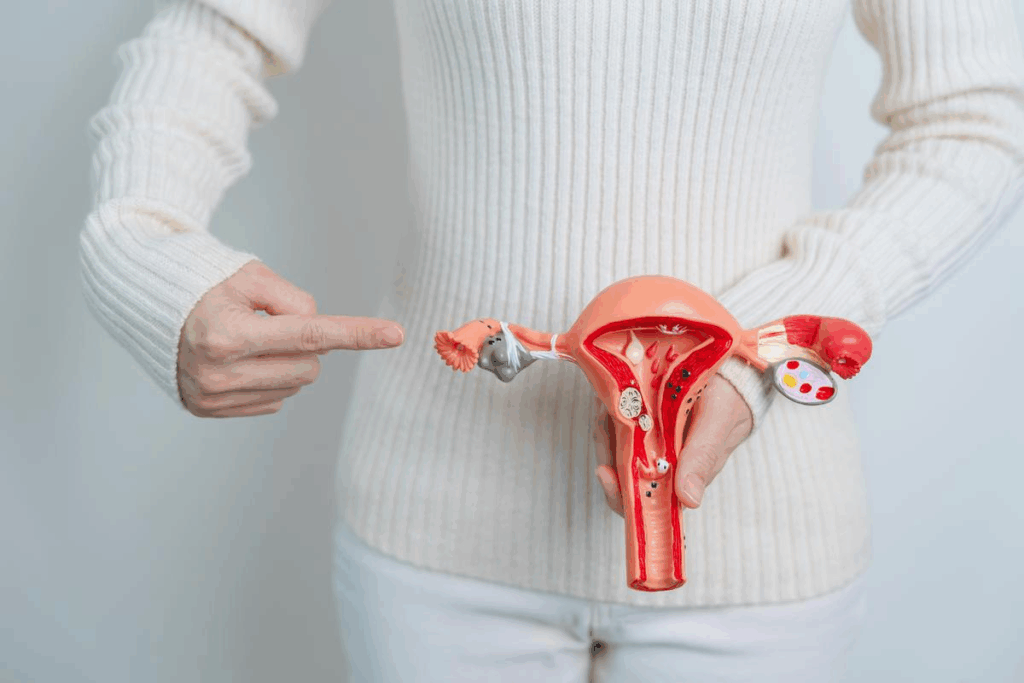
Definition and Types of Pelvic Organ Prolapse
Pelvic organ prolapse happens when the muscles and tissues that hold the pelvic organs weaken. This causes the organs to drop into the vagina. Uterine prolapse is when the uterus drops into the vaginal canal.
There are different stages of uterine prolapse. These stages range from mild to severe, affecting how much pain and discomfort a woman feels.
The types of pelvic organ prolapse include:
- Uterine prolapse
- Cystocele (bladder prolapse)
- Rectocele (rectal prolapse)
- Enterocele (small intestine prolapse)
Prevalence and Statistics in the Elderly Population
Studies show that pelvic organ prolapse gets more common with age. Women in their 80s see their doctors much more for this issue than younger women. The average age for surgery is around 60, showing elderly women often need surgery.
Age Group | Prevalence of Pelvic Organ Prolapse |
40-49 years | 10% |
60-69 years | 30% |
80+ years | 50% |
Impact on Quality of Life
Uterine prolapse can make a woman feel heavy or uncomfortable in her lower abdomen or vagina. It can really affect her life, making daily tasks hard and causing emotional pain. Finding the right treatment is key to improving her life.
Healthcare providers need to understand uterine prolapse well. This is to give the right care and support to elderly women with this condition.
Risk Factors and Causes Specific to Elderly Women

Uterine prolapse in elderly women is caused by age, hormonal changes, and health issues. Knowing these factors helps in managing and treating the condition.
Age-Related Anatomical Changes
Women’s bodies change with age, affecting the risk of uterine prolapse. These changes include:
- Weakening of the pelvic floor muscles
- Loss of connective tissue strength and elasticity
- Changes in the pelvic organ support structures
These changes can weaken pelvic organ support, leading to prolapse. Women over 80 face a high risk of needing surgery for prolapse, showing how important these changes are.
Hormonal Factors in Post-Menopausal Women
Menopause lowers estrogen levels, affecting pelvic tissues and increasing prolapse risk. Estrogen keeps vaginal tissues strong and elastic. Without it, tissues thin and weaken, making prolapse more likely.
- Thinning and weakening of vaginal walls
- Reduced collagen production
- Decreased blood supply to the pelvic area
Hormonal changes play a big role in managing uterine prolapse in elderly women.
Comorbidities and Their Influence
Elderly women often face multiple health issues that affect prolapse risk. Conditions like chronic cough, constipation, and obesity raise intra-abdominal pressure. Diabetes can also slow healing and worsen health, making treatment harder.
It’s key to understand how these health problems interact with prolapse. This helps create a treatment plan that considers the patient’s overall health.
Diagnosis and Assessment Considerations
Diagnosing uterine prolapse requires a detailed clinical evaluation. This step is key to figuring out how severe the prolapse is. It helps decide the best treatment for older women.
Clinical Evaluation Process
Diagnosing uterine prolapse starts with a detailed medical history and physical exam. We look at symptoms like pelvic pressure and trouble with bowel movements. A pelvic exam helps us see how bad the prolapse is.
Key components of the clinical evaluation include:
- Patient history to identify risk factors and symptoms
- Pelvic examination to assess the prolapse
- Assessment of other pelvic organ prolapse
Grading Systems for Prolapse Severity
There are grading systems to measure how severe uterine prolapse is. The most used is the Pelvic Organ Prolapse Quantification (POP-Q) system. It gives a clear and precise measure of the prolapse.
Stage | Description |
0 | No prolapse |
I | The leading edge of the prolapse is >1 cm above the hymen |
II | The leading edge of the prolapse is ≤1 cm proximal or distal to the hymen |
III | The leading edge of the prolapse is >1 cm below the hymen but not beyond 2 cm less than the total vaginal length |
IV | Complete procidentia or vault prolapse, with the prolapse extending beyond 2 cm less than the total vaginal length |
Research shows that in older adults, 64.8 percent have stage II or greater pelvic organ prolapse. This highlights the need for accurate diagnosis and grading.
Special Diagnostic Challenges in Elderly Patients
Diagnosing uterine prolapse in older adults can be tough. This is due to other health issues, cognitive problems, and age-related changes. We must adjust our approach to meet these challenges.
For example, cognitive issues might make it hard for patients to report symptoms. So, we need to use different diagnostic methods.
When thinking about female prolapse operation or other treatments, knowing the recovery time is key. The prolapse operation recovery time varies based on the surgery and the patient’s health.
Conservative Uterine Prolapse Treatment for Elderly
For elderly women, there are non-surgical ways to treat uterine prolapse. These methods help ease symptoms and improve life quality without surgery.
Pessary Management and Selection
Pessary management is a key non-surgical treatment. A pessary is a device placed in the vagina to support the pelvic area. Choosing the right pessary is important, based on the prolapse’s severity and the patient’s health.
The selection process involves:
- Assessing the degree of prolapse
- Considering the patient’s vaginal anatomy
- Evaluating the patient’s ability to manage the pessary
Pelvic Floor Physical Therapy Adaptations
Pelvic floor physical therapy is also effective. It includes exercises to strengthen pelvic muscles. For elderly women, these exercises can be made easier to fit their physical abilities.
Some key adaptations include:
- Modified Kegel exercises
- Pelvic floor strengthening with resistance
- Biofeedback techniques to enhance muscle control
Lifestyle Modifications for Elderly Patients
Lifestyle changes are important for managing uterine prolapse. We suggest several changes to help alleviate symptoms and prevent them from getting worse.
These modifications include:
- Maintaining a healthy weight to reduce pressure on the pelvic floor
- Avoiding heavy lifting and bending
- Managing chronic coughing and constipation
By using these non-surgical treatments, elderly women with uterine prolapse can see big improvements in their symptoms and life quality.
Surgical Treatment Options and Considerations
When other treatments don’t work, surgery is a key option for older women with uterine prolapse. Surgery can greatly improve their life by easing symptoms and supporting the pelvic organs.
Choosing surgery is a big decision. It depends on the patient’s health, how bad the symptoms are, and the risks and benefits of the surgery.
Vaginal Approaches for Elderly Patients
Vaginal surgeries are often chosen for older patients because they are less invasive and have quicker recovery times. These surgeries can be done with local anesthesia, which is safer for those with health issues.
The colpocleisis is a common vaginal surgery for older women who are not sexually active. It closes the vaginal canal to support the uterus. It’s a simple procedure with low risks.
Laparoscopic and Minimally Invasive Techniques
Laparoscopic and other minimally invasive surgeries are also used for uterine prolapse. They use smaller cuts and often cause less pain and faster recovery than open surgery.
We use laparoscopic sacrohysteropexy and similar methods to support the uterus with mesh. These require special skills but give good results for the right patients.
Weighing Risks and Benefits in Advanced Age
For older patients, it’s important to think carefully about surgery. Surgery can help a lot, but we must consider the patient’s health and how well they might recover.
Research shows that older patients can recover well from prolapse surgery. Most are fully recovered in 6 months. But every case is different. We work with each patient to find the best treatment for them.
We look at the patient’s age, health, and what they want. This helps us choose the right surgery and plan for their care after surgery. We aim for the best results for each patient.
Preoperative Preparation for Elderly Prolapse Patients
Getting ready for surgery is key for elderly women with uterine prolapse. A detailed plan is needed to meet their special needs and improve surgery results.
Medical Optimization Before Surgery
Medical optimization is vital before surgery. We check the patient’s medical history for any risks. Managing chronic conditions like diabetes and hypertension is important to avoid complications.
We also look at the patient’s medications to avoid any bad reactions with anesthesia. This helps us adjust medications safely for the surgery.
Anesthesia Considerations
Anesthesia is a big part of preparing elderly patients for surgery. We look at their health and history to pick the best anesthesia. The right anesthesia choice is key to safety and comfort during surgery.
Our anesthesiologists team up with the surgical team. They create a plan that fits the patient’s needs and considers any risks.
Patient Education and Expectation Management
Teaching patients and managing their expectations is important. We explain the surgery process to them. This reduces anxiety and prepares them for surgery.
We also talk about what surgery can and can’t do. This includes discussing benefits, risks, and other treatment options.
Recovery and Postoperative Care
The recovery after uterine prolapse surgery is key, more so for older women. It needs a detailed care plan. This includes hospital stay, home care, activity limits, and long-term check-ups.
Hospital Stay and Immediate Recovery Period
Right after surgery, a hospital stay is common. It lets doctors watch for problems and manage pain. How long you stay depends on the surgery and your health.
Key considerations during the hospital stay include:
- Monitoring for signs of infection or bleeding
- Managing postoperative pain
- Ensuring mobility to prevent deep vein thrombosis
- Providing patient education on postoperative care instructions
Home Care and Activity Restrictions
After leaving the hospital, older women need to follow certain rules. They should avoid heavy lifting, bending, or hard work.
Home care tips:
- Maintain a clean and safe environment to reduce the risk of infection
- Follow a balanced diet to support healing
- Stay hydrated by drinking plenty of water
- Gradually increase activity levels as advised by healthcare providers
Long-term Follow-up Schedule
Having a long-term follow-up plan is vital. It helps track your healing and tackles any issues. You’ll see your healthcare provider regularly.
Follow-up care may include:
- Physical examinations to assess healing
- Discussion of any symptoms or concerns
- Adjustment of postoperative care plans as necessary
- Guidance on resuming normal activities
Following a detailed care plan helps older women recover better from uterine prolapse surgery. It lowers the chance of problems and boosts their life quality.
Managing Complications and Recurrence
Managing complications and recurrence is key for treating uterine prolapse in elderly women. After surgery, patients face challenges that need careful attention.
Common Complications in Elderly Patients
Elderly patients face higher risks after uterine prolapse surgery. These risks include:
- Infection: Bacterial infections can happen after surgery, needing quick antibiotic treatment.
- Bleeding: Too much bleeding can occur during or after surgery, needing close watch.
- Mesh Complications: Mesh used in repair can cause problems like mesh erosion or pain.
Healthcare providers must know these risks and take steps to prevent them.
Strategies for Preventing Recurrence
Preventing recurrence is vital in managing uterine prolapse. Several strategies can help:
- Lifestyle Modifications: Keeping a healthy weight, avoiding heavy lifting, and managing chronic coughing can lower recurrence risk.
- Pelvic Floor Physical Therapy: Exercises to strengthen the pelvic floor muscles can support the pelvic organs.
- Pessary Use: Some patients find using a pessary helps manage symptoms and prevent recurrence.
When to Consider Reoperation vs. Conservative Management
Choosing between reoperation or conservative management depends on several factors. These include the severity of symptoms, the patient’s health, and any complications.
Reoperation might be needed if prolapse recurs and affects the patient’s quality of life. On the other hand, conservative management strategies like lifestyle changes and pessary use might be better for those with mild symptoms or who can’t have surgery.
Healthcare providers must evaluate each patient’s situation carefully. This helps decide the best approach for managing complications and preventing recurrence.
Conclusion: Optimizing Care for Elderly Women with Uterine Prolapse
For elderly women with uterine prolapse, care needs a full plan. This plan should include both non-surgical and surgical methods. Knowing about the condition, its causes, and treatment choices helps doctors give better care.
Good care starts with checking the patient’s health fully. This includes looking at any other health issues and how aging affects their body. Doctors must think about the pros and cons of each treatment option. They should also consider what the patient wants and values.
By focusing on the patient, we can make care better for elderly women with uterine prolapse. This approach helps them feel better physically and emotionally. It also lets them stay independent and enjoy a better life.
FAQ
What is the average age for prolapse surgery?
Prolapse surgery is usually for post-menopausal women. We look at each person’s health and well-being to decide when to operate.
What are the treatment options for uterine prolapse in elderly women?
Elderly women have several options. These include pessaries, physical therapy, and surgery. Surgery can be vaginal or laparoscopic.
How long is the recovery time for prolapse surgery?
Recovery time varies by surgery type and individual. Most people recover in weeks to months. We guide each patient on care and activity limits.
What are the risks associated with uterine prolapse surgery in elderly women?
Surgery risks include anesthesia issues, infection, and bleeding. We assess each patient’s health and discuss risks and benefits.
Can a prolapsed bladder be treated without surgery?
Yes, a prolapsed bladder can be treated without surgery. Options include pessaries, physical therapy, and lifestyle changes. We tailor treatment to each patient’s needs.
What is the recovery time from uterine prolapse surgery?
Recovery time depends on surgery type and individual factors. We offer personalized care and activity advice for a smooth recovery.
How effective is pelvic floor physical therapy for uterine prolapse?
Pelvic floor physical therapy is effective for uterine prolapse. It works best with other treatments. We create a treatment plan for each patient.
What are the benefits of laparoscopic surgery for uterine prolapse?
Laparoscopic surgery has benefits like smaller incisions and less pain. It also leads to faster recovery. We use these techniques for better outcomes.
How can I prevent recurrence of uterine prolapse after surgery?
Prevent recurrence by staying healthy, avoiding heavy lifting, and doing pelvic floor exercises. We also guide on post-op care and follow-ups.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://pubmed.ncbi.nlm.nih.gov/17367675/


































