Pelvic organ prolapse, like uterine prolapse, is a big health issue for millions of women. If you feel a heavy or full feeling in your vagina after having a baby, you might be affected. Treatment guide detailing how to treat prolapsed uterus, covering non-surgical management and when surgery is needed. Treatment guide detailing how to treat prolapsed uterus, covering non-surgical management and when surgery is needed.
Symptoms include feeling heaviness, discomfort, or pressure in your lower tummy or vagina. You might also see or feel a bulge or lump inside your vagina. Knowing the signs and treatment options is key to getting your life back.
At places likeLiv Hospital, our teams give you personalized care. We’ll look at the latest research and medical advice to help you with prolapse symptoms.
Key Takeaways
- Pelvic organ prolapse is a common condition in women over 50.
- Symptoms include feelings of heaviness, discomfort, or pressure in the vagina.
- A bulge or lump in the vagina can be a sign of prolapse.
- Understanding signs and symptoms is key for effective treatment.
- Specialized healthcare centers offer personalized care for prolapse treatment.
Understanding Uterine Prolapse

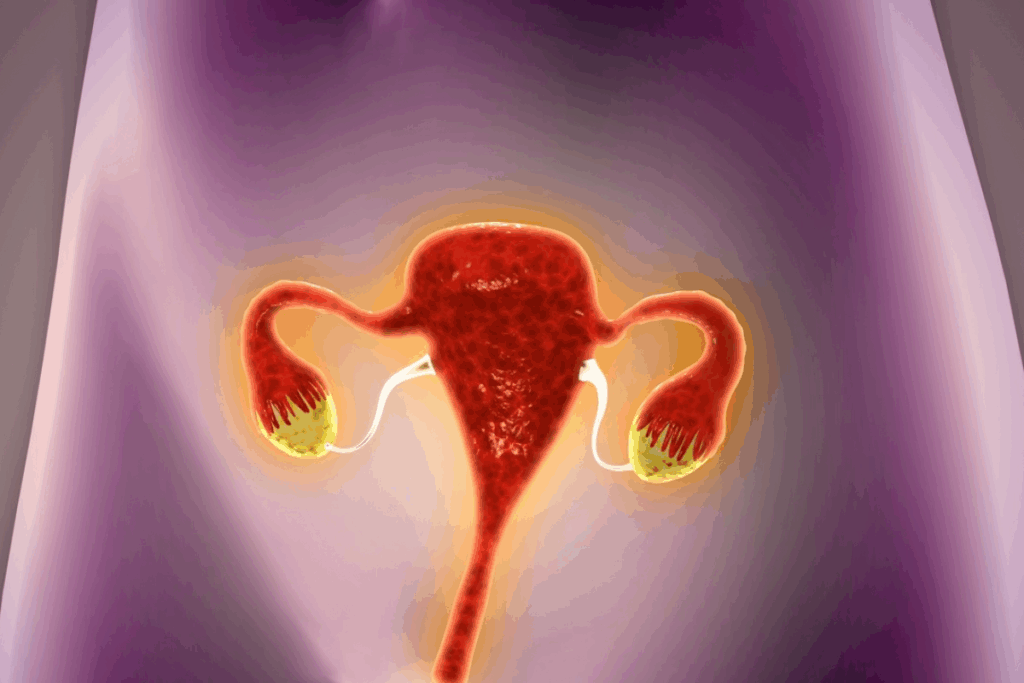
It’s important for women to know about uterine prolapse. This helps them spot symptoms early and get help fast. Uterine prolapse happens when the uterus falls into the vagina, leading to pain and other issues.
What Is a Prolapsed Uterus?
A prolapsed uterus, or uterine prolapse, is when the uterus falls into the vagina. This happens when the muscles and ligaments that hold it in place get weak.
Key factors contributing to a prolapsed uterus include:
- Weakened pelvic floor muscles
- Previous childbirth, specially vaginal delivery
- Age-related hormonal changes
- Chronic strain or pressure on the pelvic muscles
Prevalence Among Women
About 40% of women will face some degree of pelvic organ prolapse in their lives. This number goes up with age, hitting nearly 50% of women between 50 and 79.
“Pelvic organ prolapse is a significant health issue affecting women’s quality of life, specially in older age groups.”
Knowing how common uterine prolapse is shows why it’s key to spread awareness. It’s important to talk about how to prevent it and what treatments are available.
Degrees of Uterine Prolapse
Uterine prolapse is divided into different levels based on how far the uterus falls. Knowing these levels helps doctors figure out the best treatment.
Degree of Prolapse | Description |
First Degree | The uterus is displaced but remains within the vagina. |
Second Degree | The uterus has descended to the point where it is at or near the hymen. |
Third Degree (Procidentia) | The uterus has protruded outside the vagina. |
Knowing the degree of prolapse is key for doctors to choose the right treatment.
Common Causes and Risk Factors

Knowing the common causes and risk factors of uterine prolapse helps women prevent it and get the right treatment. Uterine prolapse happens when the muscles and ligaments that hold the uterus up get weak. This causes the uterus to slip into or come out of the vagina.
Childbirth and Vaginal Delivery
Childbirth, mainly vaginal delivery, is a big risk for uterine prolapse. The muscles and ligaments that support the pelvic organs can stretch or tear during vaginal delivery. Having multiple vaginal deliveries raises this risk even more. Women who have had many vaginal deliveries should talk to their healthcare provider about how to prevent it.
Age-Related Hormonal Changes
As women get older, hormonal changes, like the drop in estrogen during menopause, can lead to uterine prolapse. Estrogen keeps the pelvic muscles and ligaments strong and elastic. When estrogen levels go down, these tissues can weaken, making prolapse more likely. Women should talk to their healthcare provider about hormone therapy or other treatments to lower this risk.
Chronic Strain and Pressure
Long-term strain and increased pressure on the pelvic floor can also cause uterine prolapse. Things like chronic coughing, being overweight, and heavy lifting can put extra pressure on the pelvic muscles and ligaments. This can weaken their support for the uterus over time. It’s important to manage these conditions to lower the risk of prolapse.
By understanding these causes and risk factors, women can take steps to prevent uterine prolapse or manage its symptoms. It’s key to be aware of these factors and talk to a healthcare provider about any concerns.
Recognizing the Signs of Uterine Prolapse
Knowing the signs of uterine prolapse is key to managing it well. Women with this condition often have symptoms that affect their daily life.
What Does a Prolapse Feel Like?
A prolapse can feel like a heavy or dragging sensation in the vagina or pelvis. Some say it feels like something is falling out. Others feel pressure in the pelvic area.
These feelings can be mild or very strong. They might get worse when you stand for a long time or do physical activities.
Some women feel discomfort during sex or a feeling of incompleteness when they go to the bathroom. It’s important to talk about these feelings with your doctor.
Visual and Physical Symptoms
Visual and physical signs of uterine prolapse include vaginal bulging or a noticeable lump. In severe cases, the uterus can bulge outside the vagina. Other symptoms might be urinary incontinence, trouble emptying the bladder, or constipation.
Women might also feel pelvic pain or lower back pain. These could be related to the prolapse or other health issues. It’s important to see a doctor to figure out the best treatment.
By understanding and identifying these signs and symptoms, women can take proactive steps towards managing uterine prolapse and improving their overall well-being.
Prolapse Symptoms After Childbirth
It’s important for new moms to know the signs of prolapse after delivery. Childbirth can weaken the pelvic floor muscles, leading to uterine prolapse. We’ll look at symptoms, why they happen, and when they might show up.
Postpartum Prolapse Warning Signs
Women should watch for warning signs after childbirth. Feeling vaginal heaviness or pressure, noticing a bulge in the vagina, and discomfort during activities are common. Medical Expert, a urogynecologist, says it’s key to catch these signs early for proper care.
Some might also have trouble controlling their urine or emptying their bladder. These issues can be linked to prolapse. The severity and timing of these symptoms can vary.
Why Your Vagina Feels Heavy After Delivery
Feeling vaginal heaviness after childbirth can be scary. This is often due to weakened pelvic floor muscles from pregnancy and childbirth. These muscles can stretch or tear, causing a prolapse where organs bulge into the vagina.
A study shows that vaginal delivery strains the pelvic floor, increasing prolapse risk. This strain weakens tissues around the uterus, leading to prolapse.
Timeline for Postpartum Prolapse Development
The time it takes for postpartum prolapse to develop varies. Some notice symptoms right after delivery, while others may not until months or years later.
Several factors affect this timeline. These include the extent of pelvic floor damage during delivery, overall health, and past surgeries or multiple pregnancies.
“The onset of prolapse symptoms can be immediate or delayed, making ongoing awareness and monitoring critical for new mothers.”
Knowing the symptoms and timeline helps women manage the postpartum period. They can seek medical help if they notice concerning signs.
How to Know If You Have a Prolapse
Knowing if you have a prolapse means being aware of its signs and symptoms. It also means knowing when to see a doctor. A prolapsed uterus happens when the uterus falls out of place. This usually happens because the pelvic muscles and ligaments are weak.
Self-Assessment Techniques
To check if you might have a prolapse, follow these steps:
- Look for any unusual feelings or heaviness in your pelvic area.
- Check if you see any bulges or protrusions from your vagina.
- Notice if you have trouble with urination or bowel movements.
- Pay attention to any pain or discomfort during sex.
While checking yourself can give clues, it’s important to see a doctor for a sure diagnosis.
When to Consult a Healthcare Provider
You should see a doctor if you have:
- Constant or severe pelvic pain.
- Trouble controlling your urination or bowel movements.
- A visible bulge or protrusion from your vagina.
- Pain or discomfort during sex.
A doctor can check your symptoms and give you the right diagnosis and treatment.
Diagnostic Procedures and Tests
Tests for prolapse might include:
- A pelvic exam to see how bad the prolapse is.
- Looking at your medical history to find risk factors.
- Bladder and urine tests to check for other issues like incontinence.
These tests help doctors understand how serious the prolapse is. They then create a treatment plan for you.
How to Treat Prolapsed Uterus: Non-Surgical Options
Women with uterine prolapse have many non-surgical options to regain comfort and confidence. These treatments can manage symptoms effectively without surgery.
Pelvic Floor Physical Therapy
Pelvic floor physical therapy is a top choice for treating prolapse. It strengthens muscles that support the uterus, bladder, and bowel. This can greatly reduce symptoms.
A physical therapist can create a personalized program. This may include Kegel exercises, biofeedback, and more.
“Physical therapy has been a game-changer for many women dealing with prolapse,” notes a pelvic health specialist. “It’s a non-invasive approach that can significantly improve symptoms and quality of life.”
Benefits of Pelvic Floor Physical Therapy | Description |
Strengthens Support Muscles | Helps in supporting the prolapsed uterus |
Improves Bladder Control | Reduces symptoms of urinary incontinence |
Enhances Overall Pelvic Health | Contributes to better pelvic floor function |
Pessaries and Support Devices
Pessaries are medical devices that support the uterus. They come in different shapes and sizes. They are a good option for those who don’t want surgery.
Types of Pessaries:
- Ring pessaries
- Gellhorn pessaries
- Donut pessaries
Each type is used for different levels of prolapse. Ring pessaries are for mild to moderate cases, while Gellhorn pessaries are for more severe cases.
Lifestyle Modifications for Symptom Relief
Changing your lifestyle can help manage prolapse symptoms. Losing weight, avoiding heavy lifting, and practicing good bowel habits can help. Also, exercises that strengthen the core and pelvic muscles are beneficial.
Lifestyle Tips:
- Maintain a healthy diet rich in fiber
- Stay hydrated to prevent constipation
- Avoid smoking to reduce coughing
- Engage in regular, gentle exercise
By combining these lifestyle changes with other non-surgical treatments, women can see big improvements in their symptoms and quality of life.
Surgical Treatments for Uterine Prolapse
For women with severe uterine prolapse, surgery can help. It’s considered when other treatments don’t work well. Surgery aims to fix the pelvic floor and improve life quality.
Types of Reconstructive Procedures
Reconstructive surgery fixes the uterus and vagina support. There are several types, including:
- Uterine suspension: This suspends the uterus to prevent further prolapse.
- Vaginal vault suspension: Attaches the vagina top to a stable structure.
- Sacrocolpopexy: Uses mesh to attach the vagina to the sacrum.
These surgeries can be done through the abdomen, vagina, or laparoscopically.
Minimally Invasive Options
Minimally invasive surgery has changed uterine prolapse treatment. It has smaller cuts, less pain, and faster healing. Sacrocolpopexy is a key example, using mesh for support.
Procedure | Description | Benefits |
Sacrocolpopexy | Attachment of vagina to sacrum using mesh | High success rate, durable support |
Laparoscopic Uterine Suspension | Minimally invasive suspension of the uterus | Less postoperative pain, quicker recovery |
Recovery Process and Expected Outcomes
Recovery from uterine prolapse surgery varies. It includes some discomfort, managed with pain meds. Full recovery takes weeks to months.
Women can expect better symptoms and life quality. But, surgery has risks and complications. Talk to a healthcare provider about these.
When Surgery Is Recommended
Surgery is recommended for severe prolapse. It’s for when symptoms bother a lot and other treatments fail.
- The prolapse is severe and symptomatic.
- Non-surgical treatments have failed to provide relief.
- The woman is significantly bothered by her symptoms and desires a more definitive treatment.
Women should talk to their healthcare provider about surgery. This helps make an informed decision.
Managing Prolapse Complications
Uterine prolapse can make daily life tough for women. It can cause urinary, bowel, and sexual problems. These issues can really lower a woman’s quality of life.
Urinary Issues and Solutions
Urinary incontinence is a big problem with uterine prolapse. Management strategies include Kegel exercises. These exercises help the muscles around the bladder and urethra get stronger. Sometimes, surgery is needed to fix the problem.
Here are some ways to handle urinary issues:
- Pelvic floor physical therapy to strengthen supporting muscles
- Use of pessaries or other support devices to alleviate pressure on the bladder
- Lifestyle modifications, such as dietary changes and bladder training
Bowel Dysfunction
Bowel problems like constipation and fecal incontinence can happen with uterine prolapse. Effective management includes diet changes, bowel training, and sometimes physical therapy.
Bowel Dysfunction Issue | Management Strategy |
Constipation | Dietary changes, increased fluid intake, and bowel habits training |
Fecal Incontinence | Pelvic floor physical therapy, biofeedback, and bowel habits training |
Sexual Function and Intimacy Concerns
Uterine prolapse can affect sex and intimacy. Addressing these concerns needs a full plan. This includes counseling, physical therapy, and sometimes surgery to fix discomfort and improve sex life.
We suggest talking to a healthcare provider. They can help create a plan to tackle sexual and intimacy problems caused by prolapse.
Living with Prolapse: Long-Term Management
Living with uterine prolapse can be tough, but the right strategies can help. Women can stay active with the right approach. It’s about understanding the condition, making lifestyle changes, and knowing how to prevent it.
Emotional Impact and Mental Health
Uterine prolapse can deeply affect women’s mental health. It’s important to recognize these feelings and seek help. Counseling and support groups offer a safe place to share and learn.
The emotional effects of prolapse vary. Some may feel anxious or depressed, while others feel relieved after diagnosis and treatment. Talking openly with healthcare providers is key to dealing with these feelings.
Daily Activities and Exercise Modifications
Managing daily activities and exercise is critical for women with prolapse. Some activities can make the condition worse. For example, avoiding heavy lifting and bending helps reduce strain.
Exercise needs to be modified too. While exercise is good, activities that strain the pelvic floor should be avoided. Instead, low-impact exercises like yoga or swimming are better. They keep you healthy without making the prolapse worse.
Activity | Recommendation |
Heavy Lifting | Avoid or minimize |
High-Impact Aerobics | Replace with low-impact exercises |
Yoga or Swimming | Recommended |
Preventive Strategies for Women at Risk
Preventive strategies are key for women at risk of prolapse. Pelvic floor exercises, like Kegels, strengthen the muscles. Keeping a healthy weight and managing chronic coughing or constipation also help.
Women at risk or with prolapse should regularly review their lifestyle choices with their healthcare provider. This ensures they’re taking the right steps to prevent it from getting worse.
By following these strategies, women can manage uterine prolapse and improve their life quality. It’s about making informed choices and working with healthcare providers to tackle the condition.
Conclusion
Managing prolapse well needs a mix of medical help, lifestyle changes, and ongoing support. We’ve looked at different treatments, both non-surgical and surgical, to help understand how to treat a prolapsed uterus.
Women can manage prolapse by knowing its causes, spotting its signs, and getting the right medical care. We’ve shown how important it is to use a variety of treatments. This includes pelvic floor physical therapy, pessaries, and making lifestyle changes.
It’s key for women to know their bodies and get medical help if they notice prolapse symptoms. With the right treatment and support, managing prolapse is possible. This can greatly improve daily life, leading to a better understanding of how to treat prolapse comprehensively.
FAQ
What does a prolapse feel like?
A prolapse can feel like a heavy or pressured feeling in the pelvic area. It might feel like something is falling out of the vagina. Some women might see a bulge or lump.
What are the symptoms of prolapse after childbirth?
After childbirth, symptoms of prolapse include feeling heavy or pressured in the pelvic area. You might also notice vaginal bleeding or discharge. A visible bulge or lump in the vagina is another sign. Some women face urinary or bowel problems too.
Why does my vagina feel heavy after delivery?
A heavy vagina after delivery might be due to a prolapse. This is when the pelvic organs move into the vagina. It happens because the pelvic floor muscles get weakened during childbirth.
Can bladder prolapse cause constipation?
Bladder prolapse itself doesn’t directly cause constipation. But, it can lead to bowel problems, including constipation. This is because the displacement of pelvic organs puts pressure on the rectum.
How do I know if I have a prolapse?
To find out if you have a prolapse, see a healthcare provider. They can do a physical exam and tests to check your pelvic organs. This will help them see if you have a prolapse.
What are the treatment options for a prolapsed uterus?
Treatment for a prolapsed uterus includes non-surgical methods. These are pelvic floor physical therapy, pessaries, and lifestyle changes. There are also surgical options like reconstructive procedures and minimally invasive surgery.
Do prolapses hurt?
Some women with a prolapse might feel discomfort, pain, or pressure in the pelvic area. Others might not feel any pain. The pain level can vary based on the prolapse’s severity and individual factors.
Can a prolapse cause smelly urine?
A prolapse itself doesn’t directly cause smelly urine. But, urinary tract infections (UTIs) might be more common. These can make urine smell strong. If you notice unusual urine smells, see a healthcare provider.
How can I manage prolapse complications?
Managing prolapse complications involves treating urinary and bowel issues. It also includes addressing sexual function concerns. This can be done through lifestyle changes, non-surgical treatments, and sometimes surgery.
What preventive strategies can women at risk use?
Women at risk of prolapse can prevent it by maintaining a healthy weight. They should do pelvic floor exercises and avoid heavy lifting. Managing chronic coughing or straining also helps reduce the risk.
References
https://my.clevelandclinic.org/health/diseases/16030-uterine-prolapse
































