Last Updated on November 26, 2025 by Bilal Hasdemir
Chemotherapy is a common cancer treatment that uses strong drugs to kill cancer cells, but exposure risks make people wonder if it’s safe to sleep next to someone with chemo.
It’s natural to want to be close and support a loved one during chemotherapy. But, it’s important to know the risks and take precautions to avoid exposure to chemotherapy drugs.
By keeping hygiene strict and knowing the risks, family members can make sure their loved one’s treatment area is safe.
Key Takeaways
- Understand the risks associated with chemotherapy exposure through bodily fluids.
- Maintain strict hygiene practices to minimize exposure.
- Be aware of the potential side effects of chemotherapy on family members.
- Take necessary precautions when caring for a loved one undergoing chemotherapy.
- Create a safe environment for cancer treatment at home.
Understanding Chemotherapy and Its Effects

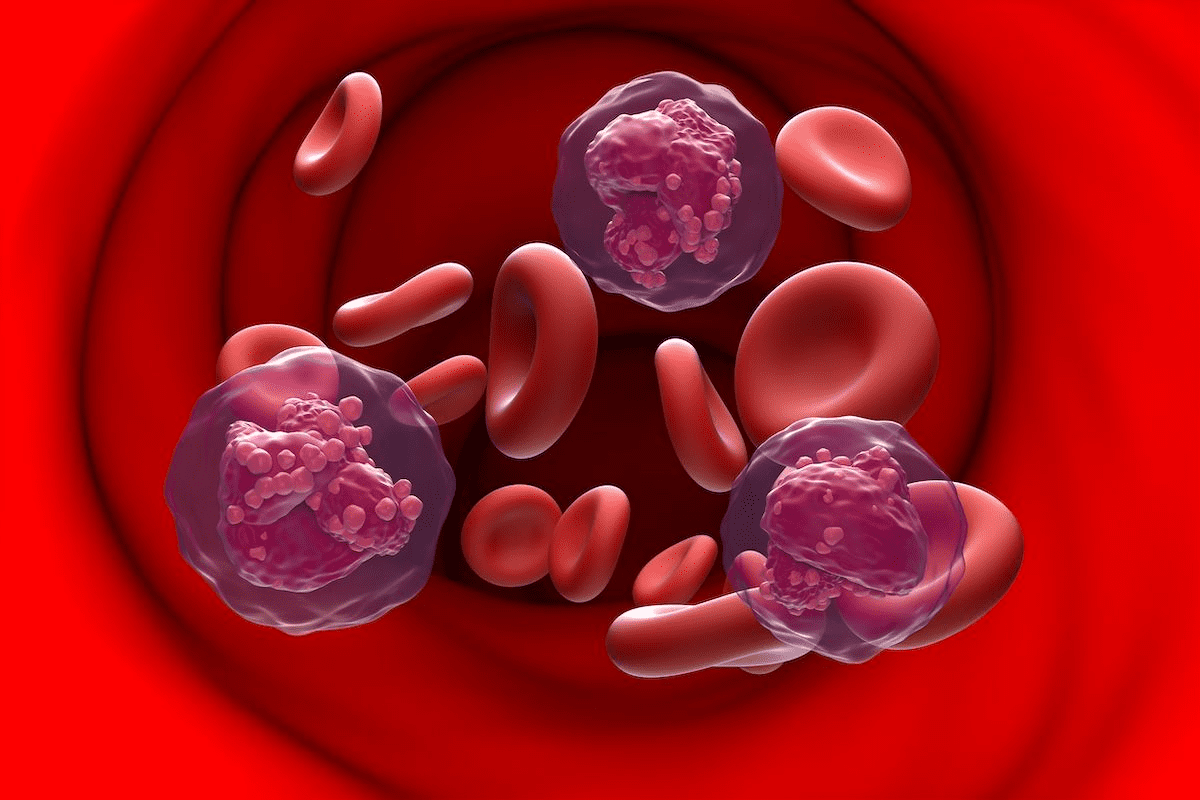
Chemotherapy is a key part of cancer treatment. It helps manage many types of cancer. It’s important for patients and their families to know about it. Chemotherapy uses strong drugs to fight cancer cells.
What is Chemotherapy and How Does It Work?
Chemotherapy is a treatment that uses drugs to kill cancer cells. It stops them from growing. The drugs can be given in different ways, based on the cancer and the patient’s health.
Chemotherapy targets cells that grow fast, like cancer cells. But it can also harm other fast-growing cells. This can cause side effects, like hair loss and digestive problems.
Common Types of Chemotherapy Administration
Chemotherapy can be given in several ways:
- Intravenous (IV) Chemotherapy: Given directly into a vein, this is common.
- Oral Chemotherapy: Taken by mouth, for some cancers.
- Topical Chemotherapy: Applied to the skin, for skin cancers.
| Administration Method | Description | Common Use |
| Intravenous (IV) | Directly into a vein | Most types of cancer |
| Oral | Taken by mouth | Specific types of cancer |
| Topical | Applied to the skin | Skin cancers |
It’s important to know how chemotherapy is given. Each way has its own benefits and side effects. Talking to a healthcare provider about these is crucial.
How Chemotherapy Medications Affect the Body
Chemotherapy drugs start a complex process in the body. They affect both the cancer cells and the patient’s health. It’s important to know how these drugs work to manage their effects and protect family members.
Immediate Physical Effects on Patients
Chemotherapy can cause many immediate physical effects. These effects depend on the drugs, dosage, and the patient’s health. Common effects include:
- Nausea and Vomiting: Many drugs cause nausea and vomiting. This can lead to dehydration and electrolyte imbalances if not managed.
- Fatigue: Patients often feel very tired, which can last throughout treatment.
- Hair Loss: Some drugs cause hair loss, not just on the scalp but also on other parts of the body.
Metabolic Processing and Excretion of Chemotherapy Drugs
After being given, chemotherapy drugs are broken down and then leave the body. Knowing this process helps understand how long the drugs stay active.
| Metabolic Process | Description | Timeline |
| Liver Metabolism | Chemotherapy drugs are processed in the liver, where they are broken down into metabolites. | Within hours to days |
| Renal Excretion | The kidneys filter out the metabolites, which are then excreted in the urine. | Several days |
| Fecal Excretion | Some chemotherapy drugs or their metabolites are excreted through the stool. | Several days to weeks |
Chemotherapy drugs stay in the system for different lengths of time. Most are greatly reduced within 48 to 72 hours after treatment. But, the exact time can depend on the drugs used and the patient’s metabolism.
Potential Risks of Secondary Exposure to Chemotherapy
Living with or caring for someone getting chemotherapy can be risky. Chemotherapy waste can be in urine, vomit, and sweat. This poses a risk to family members and caregivers.
Understanding Drug Excretion After Treatment
Chemotherapy drugs leave the body in urine, bowel movements, and sweat. How fast and how they leave depends on the treatment type, dosage, and the person’s health.
Key factors influencing drug excretion include:
- The type and dosage of chemotherapy drugs
- The patient’s metabolic rate and overall health
- The method of chemotherapy administration (e.g., intravenous, oral)
Knowing these factors helps assess and reduce the risk of secondary exposure.
Symptoms of Second-Hand Chemotherapy Exposure
Secondary exposure to chemotherapy can cause symptoms in those around the patient. These symptoms are usually mild and similar to the patient’s but less severe.
Possible symptoms of second-hand chemotherapy exposure may include:
- Nausea or loss of appetite
- Fatigue or general feeling of being unwell
- Hair loss or changes in hair texture
These symptoms can also have other causes. If you’re worried, it’s best to talk to a .
Chemotherapy Precautions for Family Members at Home
To keep your home safe during chemotherapy, family members need to follow certain steps. Chemotherapy drugs can get out through urine, stool, sweat, and saliva. This means household members might be exposed to these drugs.
General Safety Guidelines for Household Members
Following simple hygiene steps can help reduce exposure. Washing hands thoroughly after using the toilet, before eating, and after touching the patient or their bodily fluids is key. Also, use gloves when handling bodily fluids or cleaning up after the patient.
When it comes to laundry and cleaning, there are precautions too. Washing clothing and bedding separately from other laundry helps prevent contamination. Using a dedicated toilet for the patient, if possible, and cleaning the toilet seat and handle after each use also helps reduce exposure.
Duration of Precautionary Measures After Treatment
The length of time you need to take these precautions depends on the chemotherapy type and the patient’s health. Generally, the first 48-72 hours after treatment are the most critical. This is because the body excretes the most chemotherapy drugs during this time.
| Precautionary Measure | Duration | Importance Level |
| Washing Hands | Throughout treatment | High |
| Using Gloves | First 48-72 hours | High |
| Separate Laundry | Throughout treatment | Medium |
| Dedicated Toilet | First 48-72 hours | High |
By following these guidelines, family members can lower their exposure to chemotherapy drugs. This makes your home safer for everyone.
Is It Safe to Sleep Next to Someone Receiving Chemotherapy?
Sharing a bed with someone getting chemotherapy depends on several things. Chemotherapy uses strong drugs to fight cancer. These drugs can affect the body in different ways.
Factors That Determine Sleeping Safety
Several things affect how safe it is to sleep next to someone getting chemotherapy. These include:
- The type of chemotherapy being given
- How the chemotherapy is given (e.g., through an IV or by mouth)
- The specific drugs used in the treatment
- The patient’s overall health and how their body works
- The steps taken by the patient and others at home
Knowing these factors is key to understanding the risks of secondary exposure to chemotherapy.
A study in the Journal of Oncology shows why it’s important to know how chemotherapy drugs work. It says, “chemotherapy drugs can be found in urine, stool, and to a lesser extent, sweat and saliva”
“Chemotherapy drugs can be found in the urine and feces of patients for up to 48 hours after treatment.”
Recommended Sleeping Arrangements During Treatment
To lower risks, some precautions can be taken:
| Precaution | Description |
| Sleeping in Separate Beds | Consider sleeping in separate beds, especially during the first few days after chemotherapy treatment. |
| Using Protective Barriers | Using mattress protectors and waterproof bedding can help minimize exposure to bodily fluids. |
| Maintaining Hygiene | Regularly washing hands and maintaining good hygiene practices can reduce the risk of secondary exposure. |
By knowing what makes sleeping safe and taking precautions, people can lower risks. This way, they can still be close and intimate during chemotherapy treatment.
Bodily Fluid Precautions After Chemotherapy
After chemotherapy, it’s key to handle bodily fluids safely. This is for the patient’s and their family’s health. Chemotherapy waste can be in different bodily fluids, so careful handling is needed.
Managing Exposure to Urine and Stool
Urine and stool are big sources of chemotherapy waste. To avoid exposure, wear gloves when touching bedpans or toilet seats. If you can, use a separate toilet or clean the seat and area well with soap and water after each use.
Precautionary measures include flushing the toilet twice after use and washing hands well afterward. For those using diapers, it’s best to double-bag soiled diapers and throw them away in a covered trash can.
Sweat, Saliva, and Sexual Contact Considerations
Chemotherapy drugs can also be in sweat and saliva, but in smaller amounts. Precautions are needed when touching these fluids. Avoid sharing utensils or personal items that might have saliva on them.
Sweat may also have traces of chemotherapy. While the risk is lower, it’s still good to wash clothes and bedding often. For sexual contact, use barrier methods like condoms during and after treatment to reduce exposure.
By following these guidelines, families can lower the risks of secondary exposure to chemotherapy through bodily fluids. Keeping a clean environment and following these precautions is crucial for safety.
Different Types of Chemotherapy and Their Varying Risk Levels
It’s important for family members and caregivers to know about the different types of chemotherapy. Each type has its own risk level for secondary exposure.
Intravenous vs. Oral Chemotherapy Safety Differences
Chemotherapy can be given in two main ways: intravenous (IV) and oral. Intravenous chemotherapy goes straight into the bloodstream through a vein. This method can be more effective for some cancers but also increases the risk of secondary exposure through bodily fluids.
Oral chemotherapy is taken by mouth as pills or liquids. It’s easier for patients but still carries risks of secondary exposure, especially if there are spills or vomiting. The risk depends on the drug and dosage.
| Chemotherapy Type | Administration Method | Risk Level of Secondary Exposure |
| Intravenous | Directly into a vein | Higher due to higher drug concentrations |
| Oral | Oral ingestion | Variable, depending on drug and dosage |
Specific Drugs That Require Extra Precautions
Some chemotherapy drugs are riskier for secondary exposure. For example, cyclophosphamide and doxorubicin can be found in bodily fluids. It’s crucial to follow healthcare provider guidelines for handling these fluids and waste.
Healthcare providers can give detailed information on the risks of specific chemotherapy drugs. They can also provide tips on how to reduce exposure. This might include wearing protective gear, washing hands well, and following special laundry instructions for clothes and bedding.
Time Periods When Extra Caution is Needed
When a family member starts chemotherapy, it’s key to know when to be extra careful. Chemotherapy uses strong drugs to fight cancer. These drugs are vital for the patient but can be risky for others if not handled right.
The First 48-72 Hours After Treatment
The first 48-72 hours after chemotherapy are very important. During this time, the body is dealing with the drugs, and there’s more of them in the patient’s fluids.
It’s important to be careful with fluids like urine, stool, and vomit. They might have chemotherapy drugs or their leftovers. Wearing gloves, using a special toilet, or cleaning well any contaminated surfaces can help avoid exposure.
Cumulative Effects During Treatment Cycles
Chemotherapy is given in cycles, with breaks in between. The longer the treatment goes, the more risk there is of exposure to these drugs.
As treatment goes on, it’s important to keep up with safety rules. This means washing hands often and being careful with the patient’s fluids.
| Time Period | Precautions Needed | Reason |
| First 48-72 hours after treatment | Handle bodily fluids with care, use gloves, dedicated toilet | Higher concentration of chemotherapy drugs in bodily fluids |
| During treatment cycles | Continue good hygiene practices, frequent hand washing | Cumulative effect of chemotherapy increases risk of exposure |
Special Considerations for Vulnerable Household Members
Household members, especially pregnant women, young children, and the elderly, need extra care when a family member is getting chemotherapy. They might be more at risk from secondary exposure to chemotherapy.
Precautions for Pregnant Women and Young Children
Pregnant women and young children are very sensitive. Pregnant women should take extra precautions to avoid chemotherapy drugs. Young children, being curious and not always clean, are also at risk of getting exposed.
To keep them safe, pregnant women and young children’s caregivers should follow strict hygiene guidelines. This includes washing hands often and avoiding contact with the patient’s fluids. It’s best to limit their time with the patient during and right after treatment.
Elderly Family Members and Those with Compromised Immunity
Elderly family members and those with weak immune systems are also at risk. These individuals should be closely monitored for any signs of illness or bad reactions.
For their safety, keep them away from the patient during treatment. Don’t share personal items. Make sure they practice good hygiene. Caregivers should watch closely for any signs of trouble or health issues.
Creating a Safe Home Environment During Treatment
Keeping your home safe during chemotherapy is key for everyone’s health. It’s important to take steps to avoid exposure to chemotherapy agents. This helps both the patient and their family stay safe.
Bathroom Sanitation Protocols
Bathroom cleanliness is a top priority. If you can, use a separate toilet while getting chemotherapy. If not, clean the toilet with a disinfectant after each use.
- Flush the toilet with the lid down to prevent aerosolization of chemotherapy drugs.
- Clean the toilet seat, handle, and surrounding areas with a bleach-based cleaner.
- Wash hands thoroughly after using the bathroom.
Laundry and Household Cleaning Guidelines
Laundry and cleaning are also vital for a safe home. Clothes and bedding of chemotherapy patients should be washed alone. This helps prevent cross-contamination.
- Wash contaminated laundry in hot water with a mild detergent.
- Avoid shaking or handling contaminated laundry excessively to prevent spreading chemotherapy residue.
- Clean surfaces that may have come into contact with chemotherapy drugs or bodily fluids with a disinfectant.
By following these steps, families can greatly lower the risks of chemotherapy exposure at home.
Emotional Aspects of Physical Distancing During Treatment
Chemotherapy treatment often requires families to stay apart. This can make people feel lonely and isolated. Being away from a loved one can be very hard.
Maintaining Intimacy While Following Safety Protocols
Even with physical distance, families can stay emotionally close. Simple actions like regular phone calls or video chats help. Sharing meals together, even from a distance, also keeps the bond strong.
Showing love without risking safety is key. Sending messages, making small gifts, or just being in the same room can help. These actions show love and care without breaking safety rules.
Communication Strategies for Families
Good communication is vital during this time. Families should talk openly about their feelings and needs. Having a routine for regular updates keeps everyone connected.
It’s also important to let the person getting treatment decide how to communicate. This makes them feel more in charge and understood.
Key Communication Strategies:
- Regularly scheduled calls or video chats
- Open discussion of feelings and needs
- Involvement in care decisions
- Use of technology to stay connected
| Strategy | Benefit |
| Regular Check-ins | Maintains emotional connection |
| Open Discussion | Enhances understanding and empathy |
| Involvement in Care | Gives the patient a sense of control |
By using these strategies, families can stay emotionally connected even when physically apart. This helps them get through the tough times of chemotherapy together.
When to Consult Healthcare Providers About Exposure Concerns
Knowing when to talk to healthcare providers about chemotherapy exposure is key. Family members and caregivers worry about their safety when caring for someone getting treatment.
Signs That Warrant Medical Attention
After being exposed to chemotherapy, watch for signs that mean you need to see a . These include:
- Unusual fatigue or weakness
- Nausea or vomiting
- Dizziness or headaches
- Skin rashes or irritation
If you notice any of these symptoms, see a healthcare provider right away. They can check you out and tell you what to do next.
Questions to Ask Your Oncology Team
When you talk to healthcare providers about exposure worries, have questions ready. Some important ones to ask are:
- What are the specific risks from the chemotherapy being used?
- How can we reduce exposure to chemotherapy drugs or bodily fluids?
- What safety steps should we take when doing laundry, cleaning, or using the bathroom?
- Are there any specific signs or symptoms we should watch for?
By asking these questions and knowing the risks, family members and caregivers can stay safe while helping their loved one through treatment.
Common Misconceptions About Chemotherapy Exposure
It’s important to know the truth about chemotherapy exposure to clear up myths and keep everyone safe. Many people, like family and caregivers, worry about being near someone getting chemotherapy.
Myths vs. Facts About Secondary Exposure
Some think you can get exposed to chemotherapy just by touching or eating with someone who’s getting it. But studies show this risk is very low. Chemotherapy drugs mainly leave the body through urine, stool, and vomit. The biggest risk is touching these fluids directly.
Another myth is that all chemotherapy drugs are equally risky. But, the truth is different drugs have different risks. For example, some drugs might be more in urine, while others could be in sweat or saliva.
| Myth | Fact |
| Chemotherapy exposure can occur through casual contact. | The risk is mainly associated with direct contact with bodily fluids. |
| All chemotherapy drugs pose the same risk. | Different chemotherapy agents have varying risk levels. |
Understanding the Real vs. Perceived Risks
People often think the risk of getting exposed to chemotherapy is higher than it really is. This can make them take too many precautions or feel too safe. It’s key to follow the advice of healthcare experts to keep risks low and support the patient well.
Here’s a table to show the difference between real and perceived risks:
| Activity | Real Risk | Perceived Risk |
| Sharing a meal | Low | High |
| Touching patient’s vomit | High | High |
| Sleeping next to the patient | Low to Moderate | High |
Knowing the facts and taking the right steps can help reduce risks from chemotherapy exposure. This way, we can support patients better while staying safe.
Conclusion
Chemotherapy precautions are key for family members to stay safe and help at home. Knowing how chemotherapy works and taking steps to protect yourself is important. This way, you can make a safe space for your loved ones who are going through treatment.
Family members can lower the risks of getting sick by following safety tips. This includes managing body fluids and keeping the home clean. It’s also important to know the specific precautions for different chemotherapy types and to ask healthcare providers for advice.
By being careful and aware of the risks, family members can support their loved ones at home. This approach helps you care for your family while keeping yourself safe. It’s a way to balance support and safety.
FAQ
What is chemotherapy and how does it work?
Chemotherapy is a treatment for cancer that uses drugs. It targets cells that grow fast, like cancer cells, and stops them from making more.
How is chemotherapy administered?
Chemotherapy can be given in different ways. This includes IV infusion, pills, and creams. The choice depends on the cancer type, the drugs, and the patient’s health.
What are the immediate physical effects of chemotherapy on patients?
Chemotherapy can cause nausea, vomiting, and fatigue right away. It can also lead to hair loss and changes in appetite. These effects differ based on the drugs and how each person reacts.
How long do chemotherapy drugs stay in the body?
Chemotherapy drugs can stay in the body for days to weeks. This depends on the drug type and how fast the body breaks it down. It’s important to follow safety rules during this time.
What are the symptoms of second-hand chemotherapy exposure?
Symptoms of exposure to chemotherapy drugs can include nausea and dizziness. These are rare and mostly seen in those who are around drugs a lot, like healthcare workers.
How can I minimize exposure to chemotherapy drugs at home?
To reduce exposure, follow safety tips. Wear gloves when handling fluids, use a closed toilet lid, and wash clothes separately. Sleeping in different beds and staying clean can also help.
Is it safe to sleep next to someone receiving chemotherapy?
It’s safe to sleep next to someone getting chemotherapy if you take precautions. It’s best to sleep in separate beds, especially in the first 48-72 hours after treatment.
How long should I take precautions after chemotherapy treatment?
The time you need to take precautions varies. It depends on the chemotherapy type and how you react. Usually, precautions are needed for 48-72 hours after treatment.
Are there specific chemotherapy drugs that require extra precautions?
Yes, some chemotherapy drugs need extra care. These are very toxic or have a high risk of exposure. Your oncology team can tell you what precautions you need.
How can I maintain intimacy while following safety protocols?
To stay close, try holding hands or giving hugs. Schedule video or phone calls. Talking about your feelings and concerns with your partner is also important.
When should I consult my healthcare provider about exposure concerns?
Talk to your healthcare provider if you’re worried about exposure. They can answer your questions about safety and risks. They can also help if you have symptoms.
What are some common misconceptions about chemotherapy exposure?
Some people think all chemotherapy drugs are very toxic. They also believe exposure is always dangerous. But, the risks really depend on the drug and how much you’re exposed to.
How can I create a safe home environment during chemotherapy treatment?
To make your home safe, follow bathroom and laundry rules. Discuss your treatment with your oncology team for personalized advice.