Last Updated on November 26, 2025 by Bilal Hasdemir
Ovarian cancer is a complex disease that affects women worldwide. It has various subtypes that need different approaches to diagnosis and treatment. We aim to help you understand the different types of this disease.
A staggering fact is that epithelial ovarian cancer accounts for approximately 90% of ovarian cancer cases. This makes it the most common type. The rest are mostly non-epithelial, including germ cell and sex cord-stromal tumors.
Understanding these different types is essential for effective treatment and patient support. We will dive into the characteristics and implications of each type in this article.
Key Takeaways
- Ovarian cancer is a heterogeneous disease with multiple subtypes.
- Epithelial ovarian cancer is the most common type, accounting for about 90% of cases.
- Non-epithelial ovarian cancer includes germ cell and sex cord-stromal tumors.
- Understanding the different types is vital for accurate diagnosis and treatment.
- Each type of ovarian cancer has unique characteristics and implications for treatment.
Understanding Ovarian Cancer
Ovarian cancer is a major cause of death among women. It’s important to understand this disease well. This will help us see how serious it is.
Definition and Basic Anatomy
Ovarian cancer starts in the ovaries, which are key parts of the female body. The ovaries make eggs and hormones. These hormones help control the menstrual cycle and if a woman can get pregnant.
“The ovaries are a vital part of the female reproductive system, and their health is critical for overall well-being,” say doctors. Knowing how the ovaries work is key to understanding ovarian cancer.
Prevalence and Impact in the United States
Ovarian cancer is the fifth leading cause of death from cancer in women in the U.S., says the American Cancer Society. It’s a big health issue that affects many women every year.
We don’t know what causes ovarian cancer, but some things can make it more likely. These include family history and certain genetic changes.
Ovarian cancer has a big impact, not just on the women who get it. It also affects their families and the healthcare system. We need to understand its impact to make sure we have enough resources for research, diagnosis, and treatment.

Types of Ovarian Cancer: The Main Classification
Knowing the different types of ovarian cancer is key for good treatment. Ovarian cancer is split into groups based on where it starts and what it looks like. This helps doctors choose the right treatment for each patient.
Primary vs. Metastatic Ovarian Cancer
Ovarian cancer can start in the ovaries or come from other places. Primary ovarian cancer is the most common and has many subtypes. Metastatic ovarian cancer is rarer and often comes from cancers like breast or colon.
Telling primary from metastatic ovarian cancer is important for treatment. We use tests like imaging and biopsies to figure out where the cancer started.
The Two Major Categories: Epithelial and Non-Epithelial
Primary ovarian cancer is mainly divided into epithelial and non-epithelial types. Epithelial ovarian cancer, from the outer ovary layer, makes up most cases. Non-epithelial ovarian cancer, like germ cell and sex cord-stromal tumors, is rarer but important.
Epithelial ovarian cancer has subtypes like serous, clear cell, and endometrioid. Non-epithelial ovarian cancer includes germ cell tumors in younger women and sex cord-stromal tumors that make hormones.
Knowing these categories helps doctors create treatment plans that fit each type of ovarian cancer.
Epithelial Ovarian Cancer: The Most Common Type
Epithelial ovarian cancer is the most common type of ovarian cancer, making up about 90% of cases. It starts in the outer layer of the ovary. Knowing about epithelial ovarian cancer helps with early detection and treatment.
Origin and Development
Epithelial ovarian cancer comes from the cells on the surface of the ovaries. The exact cause is complex, involving genetics and environment. It happens when normal cells turn into cancer cells through genetic changes.
Many factors can influence its development. These include genetics, hormones, and reproductive history. For example, a family history of ovarian or breast cancer increases the risk.

Risk Factors Specific to Epithelial Ovarian Cancer
Several risk factors have been found for epithelial ovarian cancer. Genetic mutations like BRCA1 and BRCA2 greatly increase the risk. Reproductive history also matters; never being pregnant or having trouble getting pregnant raises the risk.
Other factors include endometriosis and hormone replacement therapy. Knowing these risk factors helps assess individual risk. It also helps in reducing risk through preventive measures or early detection.
By understanding the risk factors and how epithelial ovarian cancer develops, we can improve prevention and management. This is key for tackling this common form of ovarian cancer.
Subtypes of Epithelial Ovarian Cancer
Recent studies have shown that epithelial ovarian cancer is more diverse than we thought. This diversity is key to understanding the disease. Each subtype has its own molecular and clinical features that affect treatment and survival.
High-Grade Serous Ovarian Cancer
High-grade serous ovarian cancer (HGSOC) is the most aggressive type, causing about 70-80% of ovarian cancer deaths. It grows fast and is often diagnosed late. This makes treatment a big challenge.
HGSOC is linked to TP53 gene mutations and is usually diagnosed late. Advanced genomic profiling has helped us understand this subtype better.
Low-Grade Serous Ovarian Cancer
Low-grade serous ovarian cancer (LGSOC) is less common and has a better outlook than HGSOC. It affects younger women and is linked to KRAS or BRAF gene mutations. LGSOC is hard to treat with standard chemotherapy, so surgery is often the first choice.
LGSOC’s slow growth rate allows for a more detailed treatment plan. This often includes surgery and targeted therapies.
Clear Cell Ovarian Cancer
Clear cell ovarian cancer is hard to treat with standard chemotherapy. It’s often linked to endometriosis. Despite being diagnosed early, it’s tough to treat because of its resistance to common therapies.
“Clear cell ovarian cancer’s unique behavior calls for personalized treatment,” as guidelines suggest.
Endometrioid Ovarian Cancer
Endometrioid ovarian cancer looks like endometrial cancer and is linked to endometriosis. It has a better prognosis than some subtypes, mainly when caught early.
Managing endometrioid ovarian cancer often involves surgery and targeted therapy. This reflects its unique nature.
In summary, knowing the different types of epithelial ovarian cancer is vital for effective treatment. By understanding each subtype’s unique traits, we can improve patient care and move ovarian cancer research forward.
More Epithelial Subtypes and Rare Variants
Epithelial ovarian cancer includes many rare types, each with its own challenges. These include mucinous ovarian cancer, Brenner tumors, and mixed epithelial tumors. Knowing about these is key to managing them well.
Mucinous Ovarian Cancer
Mucinous ovarian cancer is a rare form, making up about 3% of cases. It’s known for cells that produce mucin, which can make diagnosis tricky. This is because it looks similar to other tumors from different places.
Key Features of Mucinous Ovarian Cancer:
- Often presents at an early stage, but can be bulky
- May be associated with benign or borderline mucinous tumors
- Histological diagnosis can be challenging due to the need to distinguish from metastatic mucinous tumors
Brenner Tumors
Brenner tumors are rare ovarian neoplasms that are mostly benign but can be malignant. They have nests of transitional-type epithelium in a fibromatous stroma.
Diagnostic Considerations for Brenner Tumors:
- Most are discovered incidentally during imaging or surgery for other indications
- Histological examination is key for diagnosis, showing the characteristic epithelial nests
- Malignant Brenner tumors are extremely rare and need careful histological evaluation
Mixed Epithelial Tumors
Mixed epithelial tumors have different epithelial types, like serous, mucinous, or endometrioid. This mix makes diagnosis and classification harder.
| Type | Characteristics | Diagnostic Challenges |
| Mucinous Ovarian Cancer | Mucin-producing cells, often bulky | Distinguishing from metastatic mucinous tumors |
| Brenner Tumors | Transitional-type epithelium in fibromatous stroma | Identifying malignant in typically benign tumors |
| Mixed Epithelial Tumors | Combination of different epithelial types | Classifying tumors with multiple cell types |
It’s vital to understand these rare types of epithelial ovarian cancer. This knowledge helps in making accurate diagnoses and treatment plans. We keep learning about these complex tumors to better help patients.
Common Symptoms Across Ovarian Cancer Types
It’s important to know the common symptoms of ovarian cancer to get medical help early. Ovarian cancer can show different symptoms, some of which are not specific. This makes it hard to find it early.
Early Warning Signs
While symptoms of ovarian cancer can be vague, there are some early signs to watch for. These include:
- Abdominal bloating or swelling, which can be persistent.
- Pelvic pain or discomfort that doesn’t go away.
- Difficulty eating or feeling full quickly.
- Urinary symptoms such as urgency or frequency.
These signs can mean ovarian cancer, if they last for a while. It’s key for women to talk to their doctor if they notice these symptoms.
Advanced Disease Symptoms
As ovarian cancer gets worse, symptoms can get more serious. These can include:
- Pain in the back or pelvis.
- Fatigue or feeling extremely tired.
- Changes in bowel habits, such as constipation.
- Weight loss or gain, mainly in the belly area.
In later stages, ovarian cancer can cause serious problems like bowel blockage. This can lead to severe pain and vomiting.
Knowing the symptoms of ovarian cancer, both early and late, is key to better treatment. We urge women to watch their health closely. If they notice any unusual or lasting symptoms, they should see a doctor.
| Symptom | Early Stage | Advanced Stage |
| Abdominal Bloating | Common | More pronounced |
| Pelvic Pain | Present | Often severe |
| Difficulty Eating | Occasional | Frequent |
| Weight Changes | Less common | Common, significant |
Non-Epithelial Ovarian Cancer: Germ Cell Tumors
We’re diving into germ cell tumors, a rare form of ovarian cancer. These tumors come from the germ cells in the ovary. These cells make eggs, and when they turn cancerous, they can form different types of germ cell tumors.
Origin and Development
Germ cell tumors start from the primordial germ cells in the ovary. These cells are egg precursors. The exact cause of these tumors is not known, but genetic mutations are thought to play a big role.
These tumors can happen at any age but are most common in young women. This is unlike epithelial ovarian cancer, which is more common in older women.
Types of Germ Cell Tumors
There are several types of germ cell tumors, each with its own traits. The most common types include:
- Dysgerminoma: This is the most common type, making up about 40% of all ovarian germ cell tumors. Dysgerminomas are often malignant and can spread to other parts of the body.
- Yolk Sac Tumor: Also known as endodermal sinus tumors, yolk sac tumors are highly malignant and typically occur in young women. They are known for producing alpha-fetoprotein (AFP), a tumor marker that can be detected in the blood.
- Teratoma: Teratomas are a type of germ cell tumor that can contain several different types of tissues, such as hair, muscle, and bone. While most teratomas are benign, some can become malignant.
Risk Factors and Demographics
Germ cell tumors are rare, making up about 5% of all ovarian cancers. They are more common in women under 30. The risk factors for these tumors are not as well understood as those for epithelial ovarian cancer. But, certain genetic conditions, like Turner syndrome, have been linked to a higher risk.
Knowing the risk factors and demographics of germ cell tumors is key for early detection and treatment. We will keep exploring ovarian cancer, providing detailed information to support those affected by it.
Non-Epithelial Ovarian Cancer: Sex Cord-Stromal Tumors
Sex cord-stromal tumors start from the stromal cells in the ovary. They are less common than epithelial ovarian cancers. But, they can make hormones, causing different symptoms.
Origin and Characteristics
These tumors come from the stromal part of the ovary. This part supports the ovarian follicles. They are different from epithelial ovarian cancers, which start from the surface of the ovary.
The stromal cells can turn into different types of cells. This leads to various subtypes of sex cord-stromal tumors. Knowing where these tumors come from is key for diagnosis and treatment.
Types of Stromal Tumors
Sex cord-stromal tumors can be divided into several types. These types are based on the cells they are made of and how they look under a microscope. The main types include:
- Granulosa cell tumors
- Sertoli-Leydig cell tumors
- Theca cell tumors
- Fibromas
Each type has its own special features and how it behaves. For example, granulosa cell tumors can make estrogen. This can cause endometrial hyperplasia or cancer.
| Tumor Type | Cell of Origin | Hormone Production |
| Granulosa Cell Tumor | Granulosa cells | Estrogen |
| Sertoli-Leydig Cell Tumor | Sertoli and Leydig cells | Androgens/Estrogens |
| Theca Cell Tumor | Theca cells | Estrogen |
Hormone Production and Effects
Sex cord-stromal tumors are known for making hormones. The hormone they make can affect how symptoms show up. This can range from virilization to endometrial hyperplasia or cancer.
“The hormonal activity of sex cord-stromal tumors can lead to a range of symptoms, from virilization in cases of androgen excess to endometrial hyperplasia or cancer due to estrogen excess.”
It’s important to know about these hormonal effects. They can help doctors diagnose and treat these tumors better.
In summary, sex cord-stromal tumors are a special kind of ovarian cancer. Understanding their origin, types, and hormone production is vital for the best care for patients.
Borderline Ovarian Tumors: Between Benign and Malignant
Borderline ovarian tumors are a special group of ovarian tumors. They are not fully benign or malignant. We will look into what they are, how they are managed, and their outlook.
Definition and Characteristics
These tumors have features that are in between benign and malignant. They don’t have the invasion seen in cancer. They can be serous, mucinous, or other types based on their look.
Key Features of Borderline Ovarian Tumors:
- Intermediate histological features
- Lack of stromal invasion
- Potential for malignant transformation
- Varied histological subtypes
Management and Prognosis
The main treatment for these tumors is surgery. The outlook is usually good, if caught early.
Factors Influencing Prognosis:
- Stage at diagnosis
- Histological subtype
- Presence of invasive implants
| Histological Subtype | Prognosis | Management Approach |
| Serous Borderline Tumors | Generally good, with a high survival rate | Surgical staging and removal |
| Mucinous Borderline Tumors | Variable, depending on stage and subtype | Surgery, potentially followed by surveillance |
It’s important to have a detailed follow-up plan for these patients. This helps watch for any signs of the tumor coming back or growing.
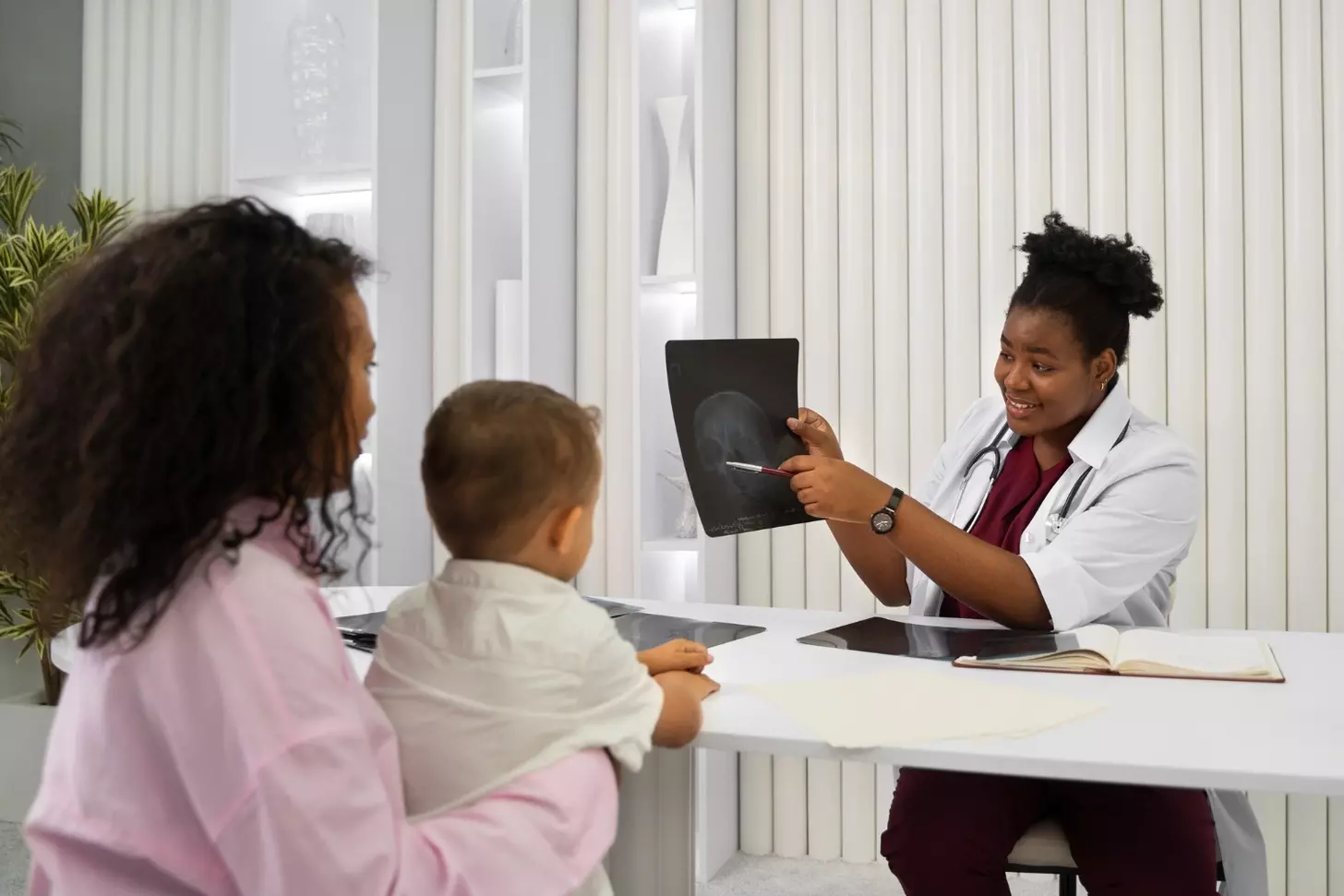
Diagnosing Ovarian Cancer Types
Getting an accurate diagnosis is key to managing ovarian cancer. Diagnosing ovarian cancer requires several tests. These tests help find out if the disease is there, what type it is, and how far it has spread.
Imaging Techniques
Imaging tests are vital in diagnosing ovarian cancer. We mainly use ultrasound to see the ovaries and spot any issues. Computed Tomography (CT) scans help us see how far the disease has spread.
In some cases, we might use Magnetic Resonance Imaging (MRI) for more detailed images. These tests are important for finding out the size and location of tumors. This information is key for planning treatment.
Biopsy and Pathology
A biopsy is a key step in diagnosing ovarian cancer. It involves taking a tissue sample from the ovary or tumor. A pathologist then examines this sample under a microscope.
The biopsy results tell us the type of ovarian cancer and how aggressive it is. Knowing this helps us create a treatment plan that fits the individual’s needs.
Genetic Testing
Genetic testing is also important in diagnosing ovarian cancer. It helps find genetic mutations like BRCA1 and BRCA2. These mutations can raise the risk of ovarian cancer and change treatment plans.
We suggest genetic testing for those with a family history of ovarian or breast cancer. The test results help us understand the risk. This information guides us in setting up screening and prevention plans.
Staging and Grading of Ovarian Cancer
Staging and grading ovarian cancer are key in planning treatment and predicting outcomes. Getting a diagnosis can be tough, but knowing the stage and grade helps tailor treatment. This makes it more effective for each person.
The FIGO Staging System
The International Federation of Gynecology and Obstetrics (FIGO) staging system is widely used. It helps us see how far the cancer has spread. This is vital for planning treatment and predicting outcomes.
The FIGO staging system divides ovarian cancer into four main stages:
- Stage I: Cancer is limited to the ovaries.
- Stage II: Cancer has spread to the pelvis.
- Stage III: Cancer has spread to the abdomen.
- Stage IV: Cancer has spread to distant sites.
Tumor Grading and Its Significance
Tumor grading is another important part of diagnosing ovarian cancer. It looks at how aggressive the tumor is by examining cancer cells under a microscope.
The grading system usually puts tumors into three categories:
- Grade 1 (Well-differentiated): Cells are closer to normal cells.
- Grade 2 (Moderately differentiated): Cells are somewhat abnormal.
- Grade 3 (Poorly differentiated): Cells are very abnormal and aggressive.
Knowing the stage and grade of ovarian cancer helps us create a detailed treatment plan. This plan is designed to match the cancer’s specific characteristics. It aims to improve treatment success rates.
Treatment Approaches for Different Ovarian Cancer Types
Ovarian cancer treatment changes based on the cancer’s type, stage, and grade. It needs a personalized plan. Each patient’s situation is different, so treatments are tailored to meet their needs.
Surgery Options
Surgery is often the first step in treating ovarian cancer, mainly for early-stage cases. The goal is to remove as much of the tumor as possible. We look at several surgical options, including:
- Total hysterectomy with bilateral salpingo-oophorectomy
- Debulking surgery to remove as much tumor as possible
- Fertility-sparing surgery for younger patients
Surgical outcomes greatly affect the patient’s prognosis and quality of life. We work closely with our surgical team to achieve the best results.
Chemotherapy Regimens
Chemotherapy is key for treating ovarian cancer, mainly for advanced cases. We use different chemotherapy regimens, including:
| Chemotherapy Regimen | Common Usage |
| Carboplatin and Paclitaxel | First-line treatment for most ovarian cancer types |
| Doxorubicin | Used in combination with other drugs for recurrent disease |
| Topotecan | Used for recurrent ovarian cancer |
A leading oncologist notes, “Chemotherapy is a key part of ovarian cancer treatment. It offers hope for better survival and quality of life.”
Targeted Therapies
Targeted therapies are a promising way to treat ovarian cancer. They focus on specific molecular targets. We look at therapies like:
- Bevacizumab, which targets angiogenesis
- PARP inhibitors, which target DNA repair mechanisms
These therapies can be used alone or with chemotherapy to improve treatment results. We keep up with the latest research in targeted therapies to offer our patients the best options.
Prevention and Risk Reduction Strategies
To lower ovarian cancer risk, we need to know our genes, change our lifestyle, and get medical help. While we can’t stop ovarian cancer completely, we can reduce the risk with smart choices.
Genetic Counseling and Testing
Genetic tests and counseling are key for spotting high-risk ovarian cancer. BRCA1 and BRCA2 gene mutations raise the risk a lot. Testing can show if you or your family have these genes.
- Genetic testing finds mutations that up the risk of ovarian cancer.
- Counseling helps people grasp their risk and make smart choices.
- Family history is key in deciding if you need genetic testing.
Lifestyle Modifications
Changing our lifestyle can also help lower ovarian cancer risk. Keeping a healthy weight and eating a balanced diet are good steps.
- Eat lots of fruits, veggies, and whole grains.
- Don’t gain too much weight.
- Stay active with regular exercise.
Prophylactic Surgery
For those at high risk, prophylactic surgery might be an option. This could mean removing the ovaries and fallopian tubes with a salpingo-oophorectomy.
- Prophylactic surgery can greatly cut down ovarian cancer risk.
- It’s usually for those with BRCA1 or BRCA2 mutations.
- It’s a big decision that should be talked over with doctors.
By using these strategies, we can lower our chance of getting ovarian cancer. It’s important to talk to doctors to figure out the best plan for you.
Prognosis and Survival Rates by Cancer Type
Ovarian cancer’s outlook changes a lot based on its type and stage. Knowing what affects prognosis helps in creating better treatment plans. This improves how well patients do.
Epithelial Ovarian Cancer Outcomes
Epithelial ovarian cancer is the most common type. It usually has a worse outlook than germ cell and stromal tumors. The five-year survival rate for epithelial ovarian cancer is about 47%.
This rate can change a lot based on when the cancer is found. For example, if caught early, survival chances are much better.
Early detection is key: Finding epithelial ovarian cancer early can raise the five-year survival rate to 90%. But, most cases are found too late. This makes treatment harder and lowers survival chances.
Germ Cell and Stromal Tumor Outcomes
Germ cell and sex cord-stromal tumors have different outlooks than epithelial ovarian cancer. These tumors are more common in younger women. They usually have a better outlook, if found early.
Germ cell tumors: The survival rate for germ cell tumors is higher. Early-stage disease has a five-year survival rate of 80% to 90%. Stromal tumors also have a good outlook, with a five-year survival rate of 70% to 90%. This depends on the stage and grade.
Factors Affecting Prognosis
Many things can change how likely someone is to survive ovarian cancer. These include the cancer’s stage, grade, and the patient’s health. How well the cancer responds to treatment also matters a lot.
It’s important for patients and doctors to understand these factors. This helps in making the best treatment choices. By focusing on the cancer type and individual patient needs, we can improve survival chances.
Conclusion
It’s key to know about the different types of ovarian cancer and how to treat them. Ovarian cancer is complex and needs a deep understanding of its types and treatments.
Healthcare providers can make better treatment plans by knowing the unique traits of each tumor type. This summary shows how important it is to care for each patient in a special way.
As we learn more about ovarian cancer, we can get better at diagnosing and treating it. Our aim is to offer top-notch support and care to those fighting this disease.
FAQ
What are the main types of ovarian cancer?
Ovarian cancer is mainly divided into two types: epithelial and non-epithelial. Epithelial ovarian cancer makes up about 90% of cases.
What is epithelial ovarian cancer?
Epithelial ovarian cancer starts in the outer layer of the ovary. It can be further classified into serous, mucinous, clear cell, and endometrioid types.
What are the subtypes of epithelial ovarian cancer?
Epithelial ovarian cancer includes subtypes like high-grade serous, low-grade serous, clear cell, and endometrioid ovarian cancer.
What are germ cell tumors?
Germ cell tumors are rare in ovarian cancer. They mostly affect younger women and come from the germ cells of the ovary.
What are borderline ovarian tumors?
Borderline ovarian tumors are rare. They show traits of both benign and malignant tumors. Their treatment and outlook depend on several factors.
How is ovarian cancer diagnosed?
Diagnosing ovarian cancer involves tests like imaging, biopsy, and genetic testing. These help find the type and extent of the disease.
What is the FIGO staging system?
The FIGO staging system is used for ovarian cancer. Tumor grading shows how aggressive the tumor is. Knowing the stage and grade helps in planning treatment.
What are the treatment options for ovarian cancer?
Treatment for ovarian cancer includes surgery, chemotherapy, and targeted therapies. The choice depends on the disease’s type, stage, and grade.
Can ovarian cancer be prevented?
Preventing ovarian cancer is not guaranteed. But, risk reduction strategies like genetic testing, lifestyle changes, and prophylactic surgery can help.