
Defining bone on bone pain (severe OA) and detailing management strategies to reduce friction and improve mobility. Bone on bone arthritis, also known as end-stage osteoarthritis, is a condition where cartilage wears away. This leaves bones rubbing against each other.
Osteoarthritis of the knee is a common issue that affects the knee joint. It causes cartilage to break down over time. While it’s a lifelong condition, there are treatments to help manage symptoms.
At Liv Hospital, they use new treatment strategies to manage bone on bone arthritis effectively. Their approach combines different types of care to improve patients’ lives.
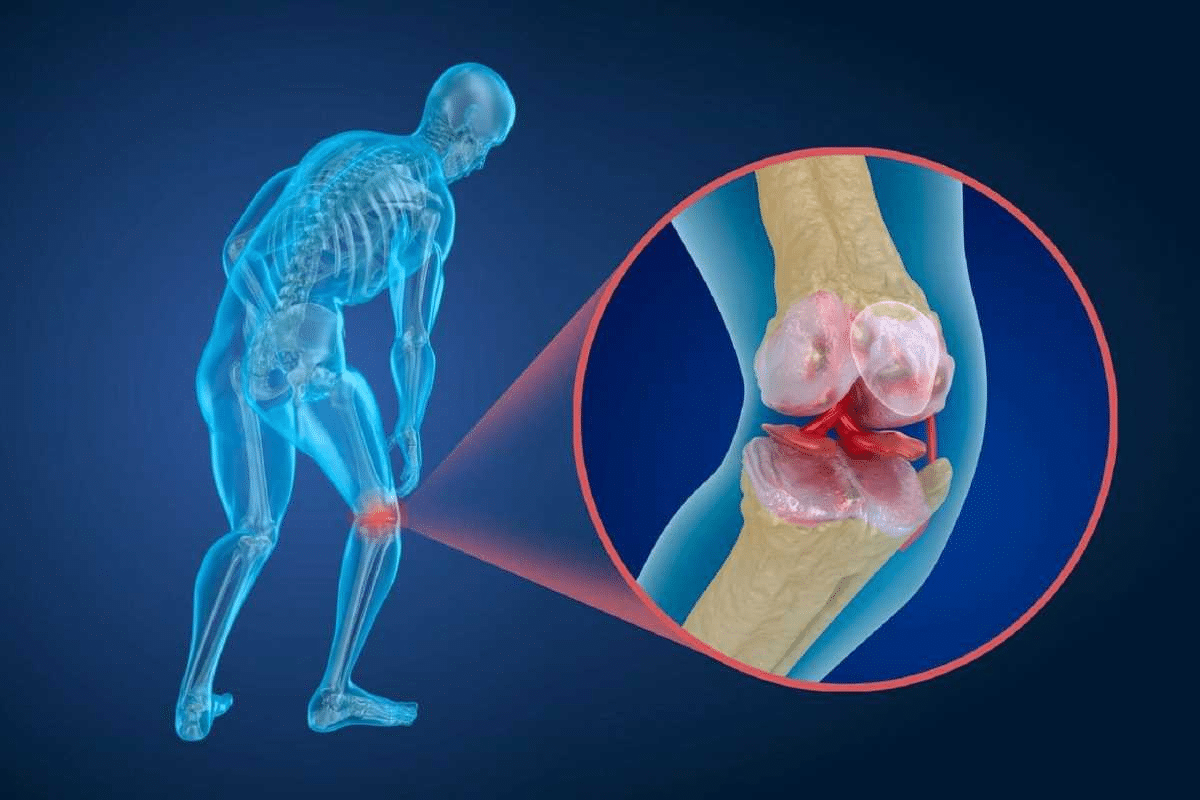
It’s important to know about bone on bone arthritis to manage its symptoms well. This severe form of osteoarthritis happens when the cartilage in a joint wears away. This leaves the bones touching each other.
Bone on bone arthritis means there’s no cartilage left in a joint. The bones then rub against each other. This is a late stage of osteoarthritis, a disease that damages cartilage and bone.
Healthy joints have cartilage that acts as a shock absorber. This allows for smooth movement and less friction between bones. The synovial fluid also helps with movement. A healthy joint has:
Cartilage degeneration happens over time due to age, injury, or too much stress on the joint. As cartilage wears away, the joint gets inflamed. This leads to pain and stiffness.
The degeneration process has several stages:
Bone on bone arthritis often affects joints like the knees, hips, and spine. It also affects the hands and neck. Knowing how it progresses helps in managing the condition and improving life quality.

The term ‘bone on bone’ describes the advanced stage of osteoarthritis. In this stage, the cartilage between bones is completely gone. This leaves the bones touching each other directly.
Osteoarthritis is a disease that wears down joints over time. It starts with cartilage loss, causing pain and stiffness. As it gets worse, the cartilage disappears, leaving bones to rub against each other.
Studies show that osteoarthritis affects millions globally. It gets worse with age, injuries, genetics, and being overweight.
|
Stage |
Characteristics |
Symptoms |
|---|---|---|
|
Early Stage |
Cartilage begins to wear away |
Mild pain, stiffness |
|
Moderate Stage |
Cartilage loss increases |
Moderate pain, swelling |
|
End Stage |
Complete cartilage loss, bone on bone |
Severe pain, reduced mobility |
Bone on bone occurs when cartilage is lost, causing bones to rub. This leads to a lot of pain, swelling, and less mobility. Experts say managing this is tough and needs a detailed plan.
“The loss of cartilage in osteoarthritis leads to bone-on-bone contact, resulting in pain and limited mobility.” – Arthritis Foundation
Osteoarthritis is different from other arthritis types like rheumatoid and psoriatic. Osteoarthritis is about wear and tear, while rheumatoid is an autoimmune disease. Knowing the differences helps in treating each condition right.
Bone on bone pain is a sign of severe degeneration. It causes bones to touch, leading to pain, swelling, stiffness, and less mobility. Treating it needs a mix of lifestyle changes, non-surgical methods, and sometimes surgery.
It’s important to know what causes bone on bone conditions. This is because understanding the causes helps manage the pain and discomfort. Bone on bone arthritis often comes from normal wear and tear or joint injury over time.
As we get older, the cartilage in our joints wears down. This leads to bone rubbing against bone. This is a big reason for osteoarthritis, where cartilage breaks down.
Table: Factors Contributing to Age-Related Wear and Tear
|
Factor |
Description |
Impact on Joints |
|---|---|---|
|
Age |
Cartilage degradation over time |
Increased risk of bone on bone contact |
|
Repetitive Stress |
Continuous strain on joints |
Accelerated wear and tear |
|
Genetic Factors |
Inherited traits affecting cartilage health |
Predisposition to osteoarthritis |
Joint injuries, like fractures or severe sprains, can raise the risk of bone on bone arthritis. These injuries can damage cartilage right away. Over time, this damage can get worse.
“Joint injuries can lead to post-traumatic arthritis, a condition where the cartilage deteriorates following trauma.”
Genetics also play a big part in osteoarthritis. If your family has a history of the condition, you’re more likely to get it too.
Being overweight puts extra stress on joints like the knees and hips. This stress can wear down cartilage faster. This can lead to bone on bone conditions.
Smoking also harms connective tissues. This can make arthritis pain worse and make managing bone on bone conditions harder.
Knowing which joints are often hit by bone on bone arthritis is key. This condition can affect many joints, but some are more likely to get it. This is because of their role and where they are in the body.
The knee is a top spot for bone on bone arthritis. Knee osteoarthritis can be mild, moderate, or severe. Severe cases have very little cartilage, causing bones to rub against each other.
The hip is another joint that often gets bone on bone arthritis. This condition wears down the cartilage in the hip. It leads to bone-on-bone contact and pain. Hip osteoarthritis can really hurt your ability to move and enjoy life.
Bone on bone arthritis can also hit the spine, mainly in the neck and lower back. When cartilage between vertebrae breaks down, it causes bone spurs and less space. This results in neck and back pain and stiffness.
Bone on bone arthritis is less common in the hands and fingers. But, it can cause pain, stiffness, and finger deformity. It affects the joints at the tips and middle of the fingers, leading to noticeable changes.
In summary, bone on bone arthritis often targets weight-bearing joints like the knees and hips. It also affects the spine and hands. Knowing which joints are at risk is vital for finding the right treatment and managing symptoms.
It’s important to know the symptoms of bone on bone arthritis to manage it well. This condition happens when the cartilage between joints wears away. This leads to bone rubbing against bone.
The pain from bone on bone arthritis can be constant and vary in how bad it is. People often feel a dull ache all the time and sharp pain during activities. Understanding these pain patterns is key to treating the condition.
Inflammation and swelling are common signs of bone on bone arthritis. As the joint gets worse, the tissues around it get inflamed. This causes swelling and more pain. Reducing inflammation is important to manage symptoms and slow the disease.
As bone on bone arthritis gets worse, joints can become stiff and move less. This stiffness is often worse after resting or being inactive. Regular exercise and physical therapy can help keep joints moving and reduce stiffness.
Bone on bone arthritis can make everyday tasks hard. Walking, climbing stairs, or even simple actions can be tough. It’s important to see how these symptoms affect daily life. This helps create a treatment plan that improves quality of life.
By knowing and recognizing bone on bone arthritis symptoms, patients and doctors can work together. This helps manage the condition and improve overall well-being.
To diagnose bone on bone arthritis, doctors use a mix of clinical findings, imaging studies, and sometimes joint fluid analysis. This method helps them see how much cartilage is lost and how damaged the joint is.
The first step is a detailed physical exam. Doctors check the joint’s movement, stability, and pain when moved. Pain patterns and how well the joint works are key signs of how severe the arthritis is.
Experts say, “The way your knee feels and functions is more important than what X-rays show.” This shows how vital a physical exam is in making a diagnosis.
Imaging is key in confirming bone on bone arthritis. The main tools used are:
|
Imaging Modality |
Primary Use in Diagnosing Bone on Bone Arthritis |
|---|---|
|
X-rays |
Assessing joint space narrowing and bone spurs |
|
MRI |
Evaluating soft tissue damage and cartilage loss |
|
CT scans |
Providing detailed images of bone structures |
Joint fluid analysis (arthrocentesis) might be done to check for other causes of pain, like infection or gout. It involves taking fluid from the joint for lab tests.
“Movement helps more than rest” is a principle that guides not only the treatment but also the diagnosis, as patient-reported outcomes are vital in understanding the impact of bone on bone arthritis.
Getting a bone on bone arthritis diagnosis doesn’t mean surgery right away. Treatment plans are made based on the person’s symptoms, health, and lifestyle.
The first step in treating bone on bone arthritis is often non-surgical treatments. These aim to lessen pain and boost joint function. They can greatly improve life quality for those affected.
Medicine is key in managing bone on bone arthritis symptoms. Doctors often prescribe pain relievers like acetaminophen and NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) like ibuprofen. These drugs help reduce pain and swelling, making daily tasks easier.
In some cases, stronger pain meds might be given for a short time. Always follow your doctor’s advice to avoid side effects.
Physical therapy (PT) is vital in treating bone on bone arthritis. It aims to improve joint movement, strengthen muscles, and enhance function. Many with advanced knee osteoarthritis fear exercising, thinking it will worsen their condition. But, physical therapy is more than just exercising. It’s a customized plan to manage pain and boost mobility.
Studies show physical therapy is a top choice for joint and muscle pain. It offers a non-invasive way to manage bone on bone arthritis.
Assistive devices can lessen joint stress. Tools like canes, walkers, and orthotics help distribute weight and ease pain. For example, using a cane on the opposite side of the affected hip or knee can reduce joint load.
For some, injections are suggested to manage joint pain. Corticosteroid injections can temporarily reduce inflammation. Hyaluronic acid injections can also help by lubricating the joint and improving function.
These non-surgical treatments provide various options for managing bone on bone arthritis. They allow individuals to work with healthcare providers to create a personalized treatment plan.
Making lifestyle changes is key to easing bone on bone arthritis symptoms. A few simple changes can greatly improve your life and help manage your condition.
Keeping a healthy weight is vital for managing bone on bone arthritis. Extra weight adds stress to joints like knees, hips, and spine, making symptoms worse. Eating right and exercising can help reduce this stress.
Effective Weight Management Tips:
Low-impact exercises are great for those with bone on bone arthritis. They keep joints moving and muscles strong without harming the joints.
Recommended Low-Impact Exercises:
It’s important to protect joints from further damage in bone on bone arthritis. Using techniques that lessen stress and strain on joints is key.
Joint Protection Strategies:
Eating a balanced diet is important for managing bone on bone arthritis. Some foods have anti-inflammatory properties that can help ease symptoms.
|
Food Category |
Beneficial Foods |
|---|---|
|
Fruits |
Berries, citrus fruits |
|
Vegetables |
Leafy greens, broccoli |
|
Proteins |
Fatty fish, nuts |
|
Grains |
Whole grains |
By making these lifestyle changes, people with bone on bone arthritis can better manage their symptoms and improve their quality of life.
For those with severe bone on bone arthritis, surgery might be a way to improve joint function and ease pain. A diagnosis of bone on bone arthritis doesn’t always mean surgery right away. But, sometimes surgery is the best option.
Surgery is considered when other treatments don’t work and the condition affects daily life. Knee replacement surgery is often suggested for severe bone on bone knee arthritis. The decision to have surgery depends on the patient’s health, how severe their condition is, and their personal wishes.
The American Academy of Orthopaedic Surgeons says surgery is considered when other treatments fail and the condition impacts quality of life.
This approach ensures that surgery is reserved for those who can benefit most from it.
Joint replacement surgery replaces the damaged joint with an artificial one. This is often done for hips and knees. Below is a table with key points about joint replacement surgery.
|
Joint |
Surgery Type |
Recovery Time |
|---|---|---|
|
Knee |
Total Knee Replacement |
6-12 weeks |
|
Hip |
Total Hip Replacement |
6-12 weeks |
Arthroscopy is a less invasive surgery that uses a small camera and tools to fix or remove damaged tissue. It’s often used in early arthritis but can help some with bone on bone arthritis too.
Recovery from surgery needs a structured rehab program to improve strength, flexibility, and function. Physical therapy is key in this process, helping patients move better and be more independent.
A successful recovery depends on following the rehab plan and making lifestyle changes to support joint health long-term.
Managing bone on bone arthritis well needs a full plan. Knowing the condition helps people take steps to feel better. This improves their life quality.
Many with osteoarthritis manage their pain and live better with the right care and lifestyle changes. Keeping a healthy weight, doing low-impact exercises, and using aids help.
Good management of bone on bone arthritis mixes medical care and lifestyle changes. Working with doctors and making smart choices helps reduce pain. It also keeps people independent.
With the right strategy, living well with bone on bone arthritis is possible. Taking charge of the condition boosts overall health. This lets people stay active and enjoy life fully.
Bone on bone arthritis happens when the cartilage between bones wears away. This causes the bones to rub against each other, leading to pain and stiffness.
Yes, bone on bone arthritis is a stage of osteoarthritis. In this stage, the cartilage is gone, and the bones touch each other directly.
Bone on bone arthritis means the cartilage between bones has broken down. This causes the bones to touch each other, leading to pain and discomfort.
Common causes include age, joint injuries, genetics, and obesity.
Joints like the knees, hips, spine, and hands are often affected.
Symptoms include pain, inflammation, stiffness, and reduced movement. These can make daily activities hard.
Doctors use physical exams, imaging, and joint fluid analysis to diagnose it.
Options include medication, physical therapy, assistive devices, and joint pain injections.
Yes, managing weight, exercising, protecting joints, and diet changes can help.
Surgery is needed when treatments fail and the condition affects daily life a lot.
Options include joint replacement, arthroscopic procedures, and other surgeries.
Manage knee pain with non-surgical treatments, lifestyle changes, and possibly surgery, based on the condition’s severity.
Untreated, it can lead to deformity. But it’s mainly about cartilage loss and bone contact.
Alternative therapies can help, but use them with conventional treatments and under a healthcare professional’s guidance.
National Center for Biotechnology Information. Bone-on-Bone Arthritis: Management of End-Stage Osteoarthritis. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6726422/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!