Bisphosphonates have been key in treating osteoporosis for over 20 years. They help keep bones strong and lower fracture risks. But, they can also cause side effects that patients need to know about.Listing seven common bisphosphonates side effects and important safety information regarding their long-term use.
It’s important to understand the possible issues with bisphosphonates. This knowledge helps patients make better health choices. Knowing what might happen can also help patients and doctors work together to protect their bones.
Key Takeaways
- Bisphosphonates are used to treat osteoporosis and maintain bone density.
- Awareness of possible side effects is key for making good health choices.
- Common side effects include stomach problems.
- Though rare, serious issues can happen.
- Patients should closely work with their doctors to care for their bones.
- Liv Hospital focuses on a patient-centered approach to treating osteoporosis.
Understanding Bisphosphonates and Their Role in Osteoporosis Treatment
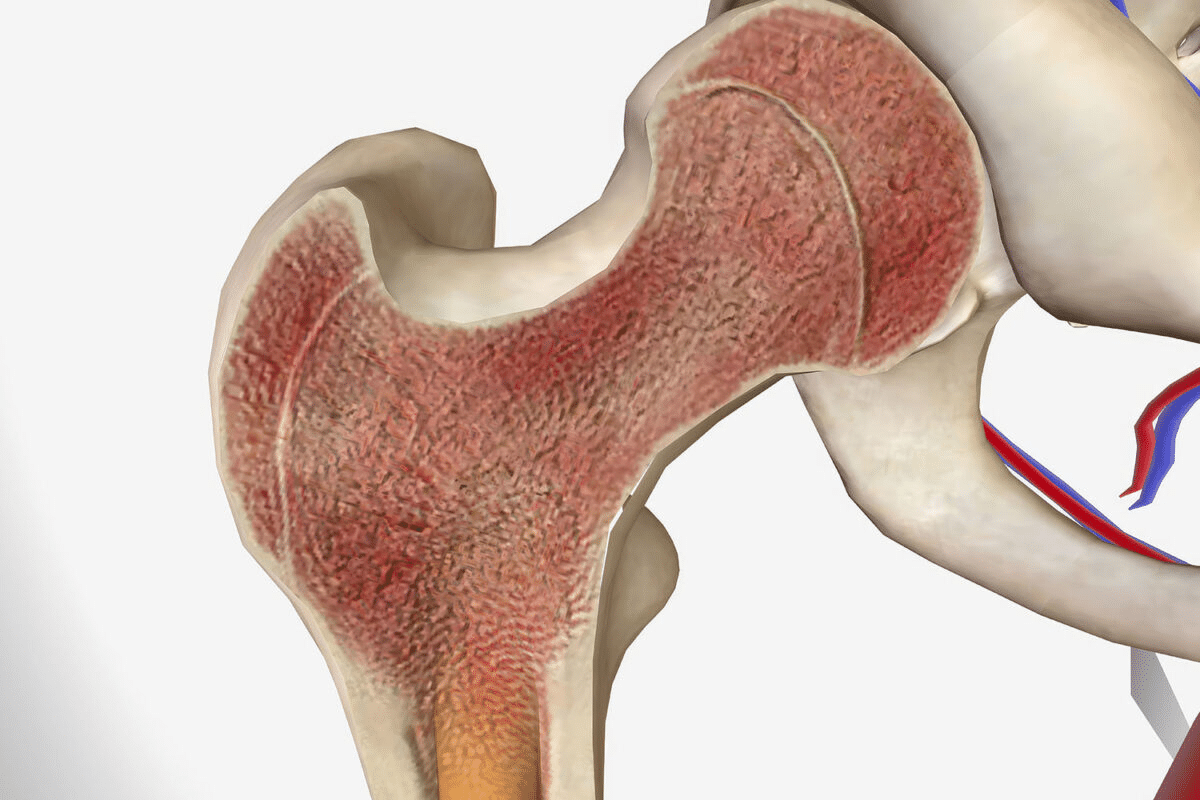
Bisphosphonates are key in fighting osteoporosis, a condition that weakens bones. They are part of a bigger plan to treat osteoporosis. Bisphosphonates are very important in this plan.
What Are Bisphosphonates?
Bisphosphonates are medicines used to treat osteoporosis. They help keep or increase bone density. This is important because it lowers the risk of fractures.
How Bisphosphonates Work to Strengthen Bones
Bisphosphonates slow down bone turnover, which lowers fracture risk. They do this by stopping bone resorption. This lets bone formation win over bone loss, making bones stronger.
Key benefits of bisphosphonates include:
- Reduced risk of vertebral and non-vertebral fractures
- Increased bone mineral density
- Slowed bone loss
Common Types of Bisphosphonate Medications
There are many bisphosphonate medicines, each with its own use and how to take it. Some well-known ones are:
|
Medication Name |
Administration Frequency |
|---|---|
|
Alendronate (Fosamax) |
Weekly or daily |
|
Risedronate (Actonel) |
Weekly or monthly |
|
Ibandronate (Boniva) |
Monthly or quarterly (intravenous) |
The right bisphosphonate and how often to take it depends on the patient’s needs and health history.
Overview of Bisphosphonates Side Effects: What Patients Should Expect
Bisphosphonates are good for treating osteoporosis but can have side effects. It’s important for patients to know about these effects. This knowledge helps manage side effects and use the medication safely.
Frequency and Severity of Side Effects
Side effects from bisphosphonates can differ for each patient. Common issues include heartburn, nausea, and trouble swallowing. Many patients, mainly those taking oral bisphosphonates, experience these problems.
“The most common adverse effects associated with oral bisphosphonates are gastrointestinal in nature,” notes a study on the safety profile of these medications.
“Gastrointestinal irritation, including esophageal irritation and gastritis, has been reported in patients taking oral bisphosphonates.”
Risk Factors That Increase Side Effect Likelihood
Some factors can make side effects from bisphosphonates more likely. These include having past gastrointestinal issues, other health conditions, and taking medications that interact with bisphosphonates. For example, those with esophageal problems are more likely to get esophageal irritation from oral bisphosphonates.
- Pre-existing gastrointestinal conditions
- Concurrent use of NSAIDs or other medications that may irritate the stomach
- Poor posture or difficulty remaining upright after taking oral bisphosphonates
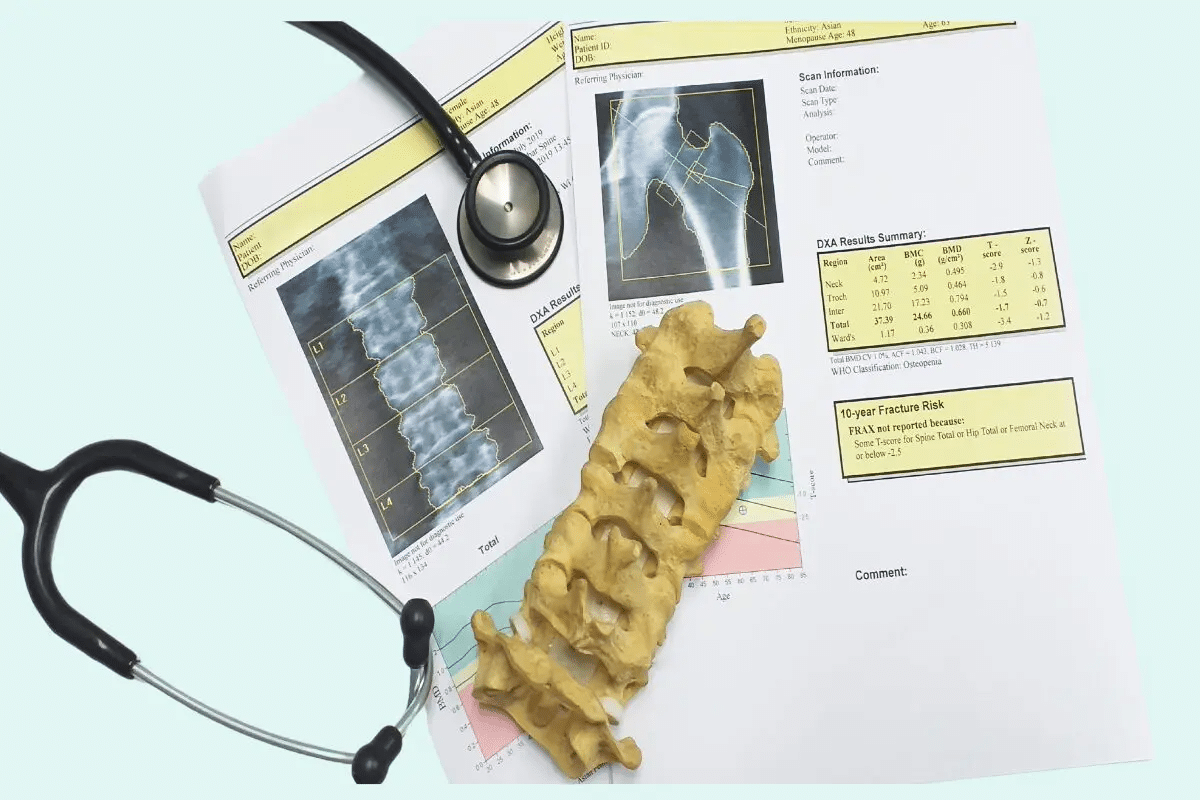
Monitoring Recommendations for Patients
Regular checks with healthcare providers are key for patients on bisphosphonates. These visits help track bone density and watch for side effects. It’s also important for patients to report any unusual symptoms right away.
Regular monitoring can help in early detection and management of side effects, improving the overall safety and efficacy of bisphosphonate treatment.
|
Monitoring Aspect |
Recommendation |
|---|---|
|
Bone Density |
Regular DEXA scans |
|
Gastrointestinal Health |
Patient reporting of symptoms; possible endoscopy for high-risk patients |
|
Renal Function |
Periodic serum creatinine checks |
Side Effect #1: Gastrointestinal Irritation and Digestive Issues
Bisphosphonates can cause stomach problems. These issues can be mild or severe. People taking these drugs for osteoporosis often face stomach troubles.
Heartburn and Esophageal Irritation
Heartburn and esophageal irritation are common in bisphosphonate users. The drug can irritate the esophagus, causing pain and discomfort. Proper administration is key to minimizing this risk.
Here’s some data on stomach side effects:
|
Symptom |
Frequency |
|---|---|
|
Heartburn |
20% |
|
Nausea |
15% |
|
Difficulty Swallowing |
10% |
Difficulty Swallowing (Dysphagia)
Dysphagia, or trouble swallowing, is another side effect. It can be uncomfortable and may lead to serious issues if not treated.
“Patients should be advised to remain upright and not lie down for at least 30 minutes after taking bisphosphonates to reduce the risk of esophageal irritation.”
Nausea and Stomach Discomfort
Nausea and stomach discomfort are common too. These symptoms can be managed with proper administration and sometimes extra medication.
Proper Administration to Minimize GI Side Effects
To lessen stomach side effects, follow these guidelines:
- Take the medication with a full glass of water.
- Remain upright for at least 30 minutes after taking the medication.
- Avoid lying down or bending over after taking the medication.
Side Effect #2: Acute Phase Reactions Following Intravenous Infusions
Intravenous infusions of bisphosphonates can trigger acute phase reactions in some patients. These reactions are a common side effect associated with the administration of bisphosphonates for osteoporosis treatment.
Flu-like Symptoms and Fever
One of the primary characteristics of acute phase reactions is the onset of flu-like symptoms, including fever. Patients may feel as though they have contracted the flu, with symptoms such as chills, fatigue, and a general feeling of being unwell.
Muscle Pain and Headaches
In addition to flu-like symptoms, patients may experience muscle pain and headaches. These symptoms can range from mild to severe and are usually temporary.
Duration and Management of Acute Reactions
The duration of acute phase reactions can vary, but they typically resolve on their own within a few days. Management strategies include the use of over-the-counter pain relievers to alleviate symptoms.
What to Expect with First vs. Subsequent Infusions
The severity and frequency of acute phase reactions tend to decrease with subsequent infusions. Approximately 1 in 3 patients experience these reactions with the first infusion, characterized by flu-like symptoms, fever, muscle pain, and headaches. Patients should be aware of this and discuss any concerns with their healthcare provider.
Side Effect #3: Bone, Joint, and Muscle Pain
Bisphosphonates help treat osteoporosis but can cause pain in bones, joints, and muscles. This side effect can really affect how well a person lives and sticks to their treatment plan.
Distinguishing Medication-Related Pain from Osteoporosis Symptoms
It’s hard to tell if pain from bisphosphonates or osteoporosis is the cause. Doctors suggest a detailed check-up to figure out the pain’s source.
The National Osteoporosis Foundation says it’s key to know why someone is in pain. This is because osteoporosis can cause pain from fractures or other bone problems.
Onset and Duration of Pain Symptoms
When pain starts from bisphosphonates can differ for each person. Some might feel pain right after starting treatment. Others might not feel it until later.
A study in the Journal of Bone and Mineral Research found pain usually starts about 3 years after starting bisphosphonates.
Management Strategies for Bisphosphonate-Related Pain
Dealing with pain from bisphosphonates needs a few steps. Changing the treatment plan, like the dose or type of bisphosphonate, might help.
- Over-the-counter pain relievers
- Physical therapy to improve mobility and strength
- Alternative therapies like acupuncture
When Pain May Indicate Discontinuation
Severe pain might mean stopping bisphosphonates. Doctors look at the good and bad of keeping up treatment for each patient.
“For patients with severe musculoskeletal pain, deciding to keep or stop bisphosphonates depends on their health and risk of fractures.”— American Society for Bone and Mineral Research
Side Effect #4: Osteonecrosis of the Jaw (ONJ)
Osteonecrosis of the jaw (ONJ) is a serious issue for those taking bisphosphonates for osteoporosis. It causes jawbone tissue death, leading to exposed bone in the mouth. This can be very painful and hard to treat.
Understanding the Mechanism of ONJ Development
The exact cause of ONJ is not known, but bisphosphonates are thought to disrupt bone remodeling. This leads to micro-fractures and bone death. Poor oral health and certain dental procedures can trigger ONJ in susceptible individuals.
Risk Factors That Increase ONJ Likelihood
Several factors raise the risk of ONJ. These include how long you’ve been on bisphosphonates, the type of bisphosphonate, and dental problems or recent surgery. Patients with a history of dental extractions or oral surgery are at higher risk.
|
Risk Factor |
Description |
|---|---|
|
Duration of Therapy |
Longer treatment duration increases ONJ risk |
|
Dental Problems |
Presence of dental issues or recent surgery |
|
Potency of Bisphosphonate |
Higher potency bisphosphonates have a higher risk |
Preventive Dental Care for Bisphosphonate Users
Preventive dental care is key for bisphosphonate users. Regular dental visits, good oral hygiene, and avoiding unnecessary dental work can lower ONJ risk. Patients should inform their dentist about their bisphosphonate treatment.
Treatment Options When ONJ Occurs
When ONJ happens, treatment aims to manage symptoms and pain. This may include antibiotics, pain meds, and sometimes surgery to remove dead bone tissue.
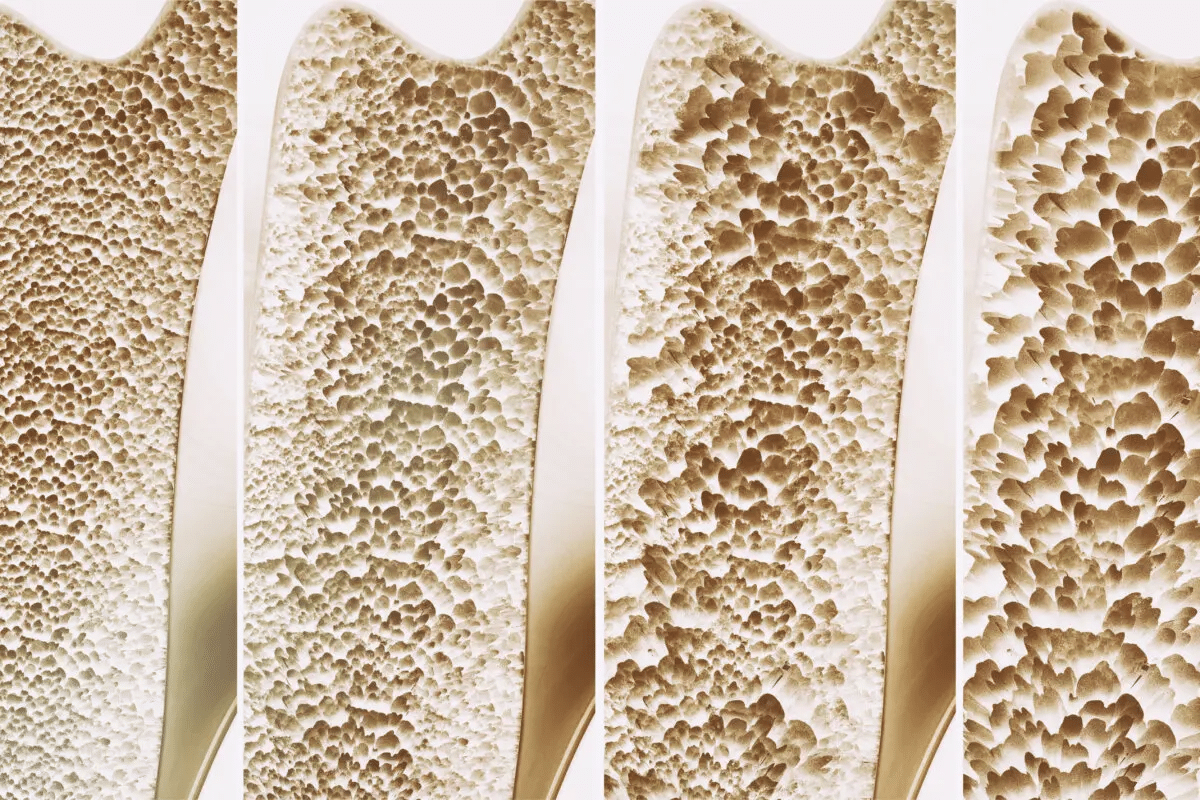
Side Effect #5: Atypical Femoral Fractures
Bisphosphonates are good for treating osteoporosis but can cause atypical femoral fractures. This is a rare but serious side effect for those on long-term therapy.
How Bisphosphonates Can Occasionally Lead to Fractures
Bisphosphonates slow down bone loss, which can cause micro-cracks in bones. This increases the risk of atypical femoral fractures, mainly in those treated for over 5 years. It’s important for patients and doctors to know about this risk.
Warning Signs and Symptoms to Monitor
Those on long-term bisphosphonate therapy should watch for new thigh, hip, or groin pain. These signs could mean an atypical femoral fracture is coming. Spotting it early is vital to avoid a full fracture.
- New or unusual pain in the thigh, hip, or groin area
- Pain that gets worse with activity
- Difficulty walking or bearing weight on the affected leg
Diagnostic Approaches for Suspected Atypical Fractures
When atypical femoral fractures are suspected, X-rays or MRI scans are used to confirm. Quick evaluation is key to start the right treatment.
Long-term Management Considerations
For those at risk, doctors might look at other treatments or change the bisphosphonate plan. This could mean a break from the drug or switching to something else.
“The decision to continue or modify bisphosphonate therapy should be based on an individual patient’s risk-benefit profile.”
Knowing the risks and benefits of bisphosphonates helps patients and doctors make better choices for osteoporosis treatment.
Side Effect #6: Hypocalcemia and Electrolyte Imbalances
Bisphosphonates can cause hypocalcemia, which is low calcium in the blood. This is more common in people who already have low calcium or vitamin D. It’s important to manage this condition to avoid serious problems.
Mechanism of Calcium Depletion
Bisphosphonates stop bones from releasing calcium into the blood. This can worsen hypocalcemia in those with low calcium or vitamin D. It’s key for patients to have enough calcium and vitamin D before starting treatment.
Symptoms of Low Calcium Levels
Hypocalcemia can cause several symptoms, including:
- Muscle cramps and spasms
- Numbness or tingling in the fingers and toes
- Fatigue and weakness
- Seizures in severe cases
It’s important to notice these symptoms early to get help quickly.
Importance of Calcium and Vitamin D Supplementation
Supplementing with calcium and vitamin D is vital for patients on bisphosphonates. Getting enough of these nutrients can help avoid electrolyte imbalances. Patients should talk to their doctor about the right amount to take.
Monitoring and Managing Electrolyte Levels
It’s important to regularly check electrolyte levels, like calcium, for patients on bisphosphonates. Doctors might suggest blood tests to catch any imbalances. Spotting problems early helps prevent bigger issues.
Doctors might adjust the bisphosphonate dose, add calcium and vitamin D supplements, or fix any underlying issues. They can create a plan that fits each patient’s needs.
Side Effect #7: Ocular Complications and Vision Changes
Ocular complications and vision changes are possible side effects of bisphosphonate therapy. Patients need to know about these risks. Bisphosphonates can cause eye-related issues.
Types of Eye Problems Associated with Bisphosphonates
Bisphosphonates are linked to eye problems like conjunctivitis, uveitis, and scleritis. These can cause discomfort, pain, and serious vision issues if not treated quickly.
Recognizing Vision-Related Side Effects
Patients on bisphosphonates should watch for vision or eye health changes. Look out for blurred vision, eye pain, redness, and increased sensitivity to light. If these symptoms appear, see a healthcare provider right away.
Treatment Approaches for Eye Complications
Treatment for eye problems linked to bisphosphonates varies. Sometimes, stopping the bisphosphonate is needed. Other times, more medications or therapies are required.
Preventive Eye Care for Patients on Bisphosphonates
Preventive care is important to reduce eye risks. Regular eye exams and telling your eye care provider about bisphosphonate treatment are key. This proactive approach helps protect eye health during osteoporosis treatment.
Conclusion: Weighing the Benefits and Risks of Bisphosphonate Therapy
Bisphosphonates are a key part of treating osteoporosis. They help lower the chance of fractures in patients. But, they can also cause side effects that patients need to know about.
It’s important to understand both the good and bad sides of bisphosphonate therapy. These drugs make bones stronger. Yet, they might upset your stomach, cause fever, or lead to other issues.
Patients should talk to their doctors to lessen risks. They should watch for side effects, take care of their teeth to avoid jaw problems, and know the signs of unusual bone fractures.
Being informed and careful helps patients get the most from bisphosphonate therapy. This careful balance is essential for treating osteoporosis well.
FAQ
What are the common side effects of bisphosphonates?
Bisphosphonates can cause stomach upset, flu-like symptoms, and muscle pain. They may also lead to jaw problems, bone fractures, and eye issues. Hypocalcemia and other side effects are possible too.
How can gastrointestinal side effects be minimized when taking bisphosphonates?
To lessen stomach problems, take bisphosphonates with an empty stomach. Stay upright for 30 minutes after. Avoid bending or lying down.
What are the symptoms of an acute phase reaction following intravenous bisphosphonate infusion?
You might feel flu-like, have a fever, muscle pain, or headaches. These symptoms start within 24-48 hours and usually go away in a few days.
How can bone, joint, and muscle pain be managed in patients taking bisphosphonates?
For pain, try over-the-counter pain meds, rest, and physical therapy. Sometimes, stopping the bisphosphonate is needed.
What is osteonecrosis of the jaw (ONJ), and how can it be prevented in bisphosphonate users?
ONJ is jawbone damage. To prevent it, see your dentist regularly, keep your teeth clean, and avoid dental work while on bisphosphonates.
What are the warning signs and symptoms of atypical femoral fractures associated with bisphosphonate use?
Look out for thigh or groin pain. This could mean an atypical femoral fracture is coming. Tell your doctor if you have these symptoms.
Why is calcium and vitamin D supplementation important when taking bisphosphonates?
Taking calcium and vitamin D helps keep bones strong. It also prevents low calcium levels, a side effect of bisphosphonates.
What types of eye problems have been associated with bisphosphonate use?
Bisphosphonates can cause eye issues like conjunctivitis, uveitis, and scleritis. If you have vision problems, tell your doctor.
How can patients minimize the risks associated with bisphosphonate therapy?
Follow your doctor’s advice, report any side effects, and keep up with regular check-ups. This helps manage risks and adjust treatment as needed.
What are the benefits of bisphosphonate therapy in treating osteoporosis?
Bisphosphonates help prevent fractures, slow bone loss, and increase density. They are a key treatment for osteoporosis.
What are the potentially long-term side effects of bisphosphonate therapy?
Long-term use can raise the risk of fractures, jaw problems, and other issues. It’s important to monitor and assess risks over time.
References
Government Health Resource. Evidence-Based Medical Guidance. Retrieved from https://www.nejm.org/doi/full/10.1056/NEJMcp1513724



































