What bacteria causes UTI? Learn about the main culprits and how they guide urinary tract infection treatments. Crucial, powerful facts on E. coli and more.
Urinary tract infections (UTIs) are a big problem worldwide. Over 4 billion cases happen every year. The main cause is Escherichia coli (E. coli) bacteria, which is behind 60-80% of uncomplicated UTI cases. We will look into the latest facts and how healthcare leaders are tackling this issue.
E. coli bacteria cause most UTIs and are treated with antibiotics. But some strains resist common antibiotics, making treatment key. At LIV Hospital, we aim to offer top-notch healthcare and support for UTI patients.
Key Takeaways
- E. coli is the primary bacterium responsible for UTIs.
- UTIs are a significant global health concern.
- Antibiotic resistance is a growing concern in UTI treatment.
- Effective treatment is key to managing UTIs.
- LIV Hospital provides complete support for UTI patients.
Understanding Urinary Tract Infections and Their Bacterial Origins
UTIs are a big health problem. They happen because of harmful bacteria. We will look at what UTIs are, how common they are, and how bacteria cause them.
What Is a UTI and Global Prevalence Statistics
A Urinary Tract Infection (UTI) happens when bacteria get into the urinary tract. This can cause infection in the urine, bladder, or kidneys. Women are 30 times more likely to get a UTI because of their anatomy.
UTIs are a big deal worldwide. They affect millions of people. Studies show that UTIs are very common, mostly in women.
How Bacteria Enter and Colonize the Urinary Tract
Bacteria get into the urinary tract through the urethra. They can then infect different parts. The most common way is when bacteria from the gut move up to the urinary tract.
Escherichia coli (E. coli), a common gut bacterium, is often found in UTIs. This shows how important gut health is for the urinary tract.
Demographic Differences in UTI Bacterial Causes
The bacteria causing UTIs can differ based on who you are. For example, E. coli is found in up to 76.7% of UTIs in some groups. Other bacteria, like Klebsiella pneumoniae and Enterococcus faecalis, are also common in certain people or groups.
Knowing these differences helps doctors treat UTIs better.
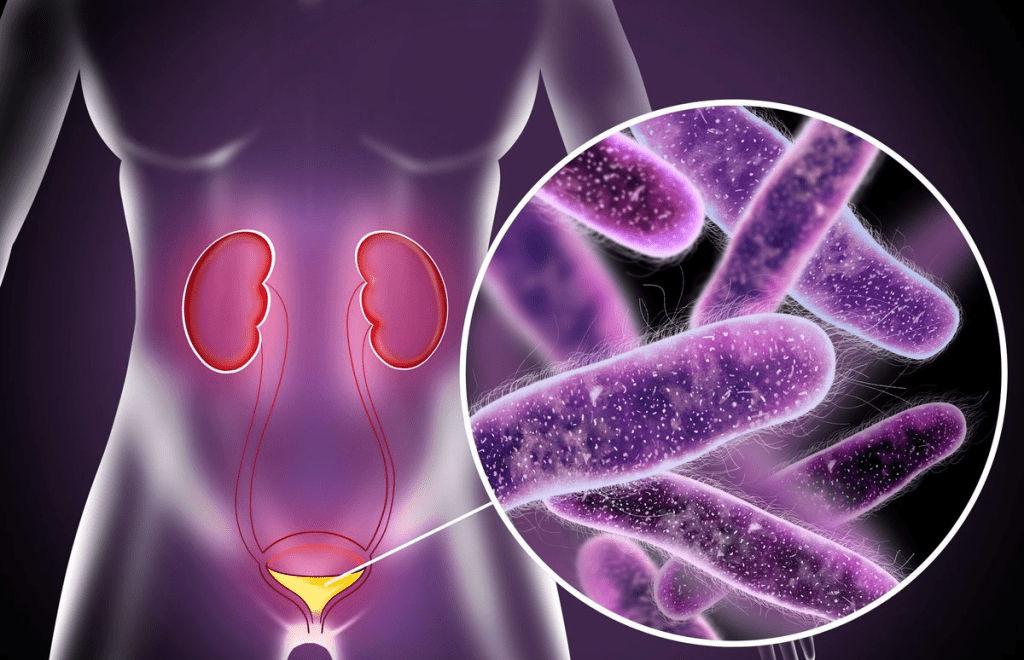
Escherichia coli (E. coli): The Leading Cause of UTIs
UTIs are most commonly caused by Escherichia coli (E. coli). This bacterium is usually harmless in the gut but can cause infections when it enters the urinary tract. We will look at why E. coli is the main cause of UTIs, its virulence factors, and how it affects patients.
Prevalence of E. coli in UTIs
E. coli is responsible for about 80% of all UTI cases. This is because it’s common in the human gut and can easily contaminate the urinary tract. The bacterium can cause infections if it enters the urinary tract, usually from stool that migrates into the urethra.
Several reasons explain why E. coli is so dominant in UTIs:
- E. coli’s presence in the gastrointestinal tract makes it a common contaminant of the urinary tract.
- The bacterium’s ability to adhere to and colonize the urothelial cells lining the urinary tract.
- The virulence factors that E. coli possesses enable it to cause disease.
Virulence Factors of E. coli in UTIs
E. coli’s success in causing UTIs is due to its various virulence factors. These include:
- Adhesins: Proteins on the surface of E. coli that facilitate its attachment to the urothelial cells.
- Pili or Fimbriae: Hair-like structures that help in adhesion and colonization.
- Toxins, Such as hemolysin, can damage host cells.
These virulence factors help E. coli establish infection, evade the host’s immune response, and cause disease.
E. coli UTI Presentation and Symptoms
The presentation and symptoms of E. coli UTIs can vary. They depend on the site of infection within the urinary tract. Common symptoms include:
- Dysuria (painful urination)
- Frequent urination
- Urgent need to urinate
- Cloudy or strong-smelling urine
In more severe cases, such as pyelonephritis (kidney infection), symptoms can include flank pain, fever, and nausea. Understanding these symptoms is key for timely diagnosis and treatment.
Other Common Bacteria Responsible for UTIs
Besides E. coli, other bacteria cause many UTIs. Each has its own traits. Knowing about these is key to the right diagnosis and treatment.
Klebsiella pneumoniae: Characteristics and Prevalence
Klebsiella pneumoniae is a big UTI cause, mainly in those with weak immune systems or with catheters. It’s tough to treat because it often resists antibiotics.
Studies show Klebsiella pneumoniae is a big part of UTIs in hospitals. This calls for strict infection control.
Enterococcus faecalis: Hospital-Acquired UTI Specialist
Enterococcus faecalis often causes UTIs, mostly in hospitals. It’s hard to kill because it can live on many surfaces and resist disinfectants.
Those with catheters or who have had invasive procedures are at risk. They need careful management and prevention.
Proteus mirabilis: The Stone-Forming Bacteria
Proteus mirabilis makes urine pH go up, leading to stones. It’s linked to complicated UTIs and can cause serious problems if not treated properly.
“The ability of Proteus mirabilis to form stones complicates UTI treatment, as these stones can harbor bacteria, making them resistant to antibiotic therapy.”
Staphylococcus saprophyticus: Common in Sexually Active Women
Staphylococcus saprophyticus is a big UTI cause in young, sexually active women. It usually responds well to common antibiotics, making treatment effective.
Knowing about Staphylococcus saprophyticus helps tailor treatments for each person’s needs.
Urinary Tract Infection Treatments: Targeting Specific Bacteria
To treat urinary tract infections (UTIs) well, we must find out which bacteria are causing them. Escherichia coli is the main culprit behind most UTIs. It’s also linked to a lot of deaths from resistant infections.
Diagnostic Methods for Identifying UTI-Causing Bacteria
Getting a correct diagnosis is key to treating UTIs. We use urinalysis and urine culture to find out which bacteria are causing the problem. Urinalysis checks for bacteria, blood, or other issues in the urine. Urine culture tells us which bacteria are present and how they react to antibiotics.
These tests help doctors choose the right treatment. This approach improves treatment results and fights against antibiotic resistance.
First-Line Antibiotic Treatments Based on Bacterial Type
The choice of antibiotic depends on the bacteria causing the UTI. For example, trimethoprim-sulfamethoxazole and nitrofurantoin are often used for E. coli infections. But, antibiotic resistance can change by location, so local rates guide treatment.
For more complex UTIs or those caused by resistant bacteria, stronger antibiotics or other treatments might be needed.
Alternative and Emerging Treatment Approaches
As antibiotic resistance grows, we’re looking into new treatments. These include non-antibiotic ways to prevent UTIs, like changing habits and using cranberry products. But more research is needed to confirm their effectiveness.
New treatments like bacteriophage therapy and novel antibiotics are showing promise. We’re committed to keeping up with these advancements to give our patients the best care.
The Growing Challenge of Antimicrobial Resistance in UTI Bacteria
Antimicrobial resistance in urinary tract infection (UTI) bacteria is a big threat to health worldwide. In 2021, UTI cases hit 4.49 billion, with Escherichia coli (E. coli) being the most common and resistant. As bacteria resist antibiotics, finding new treatments is key.
Current Statistics on Resistant UTI Pathogens
Research shows E. coli, the top UTI cause, is getting more resistant to antibiotics. “The rise in E. coli resistance to antibiotics is alarming,” experts say. This calls for new ways to treat UTIs.
Bacteria become resistant by changing to avoid antibiotics. They can do this through genetic changes or by getting genes from other bacteria. This makes treating UTIs harder with usual antibiotics.
Mechanisms of Resistance Development in Common UTI Bacteria
UTI bacteria resist antibiotics in several ways:
- They make enzymes that neutralize antibiotics
- They change their cell walls to block antibiotics
- They use pumps to throw out antibiotics
- They mutate to dodge the antibiotic’s target
Knowing how bacteria resist is vital for new treatments. We must keep up with these changes to fight resistant infections.
Multidisciplinary Care Pathways for Resistant Infections
Beating antimicrobial resistance in UTI bacteria needs teamwork. This includes:
- Better tests to quickly find the bacteria and their resistance
- Targeted antibiotics based on resistance
- New antibiotics and treatments
- Better ways to stop resistant bacteria from spreading
By using these methods, we can handle resistant UTIs better. It’s important to keep watching resistance trends and adjust our treatments.
“The key to addressing antimicrobial resistance lies in a collaborative effort between healthcare providers, researchers, and policymakers to develop and implement effective countermeasures.”
Conclusion: Preventing and Managing Bacterial UTIs Effectively
Urinary tract infections are a big health issue. Research shows that about 40% of women in the U.S. will get a UTI at some point. Most UTIs are caused by Escherichia coli, followed by Klebsiella and other bacteria. It’s important to know the causes and how to prevent them.
To prevent UTIs, we can follow simple steps. Wipe from front to back, drink plenty of water, and pee after sex. If you do get a UTI, getting it treated quickly is key. This helps manage the infection and improves health outcomes.
Healthcare systems worldwide need to keep their UTI treatment plans up to date. They should also work together to give patients the best care. Healthcare providers must stay current with UTI causes and treatments to provide top-notch care.
FAQ
What is a Urinary Tract Infection (UTI) and what causes it?
A UTI is an infection in the urinary system. It’s usually caused by bacteria, with E. coli being the main culprit. This bacterium is responsible for 60-80% of UTI cases.
What are the symptoms of a UTI caused by E. coli?
Symptoms of a UTI caused by E. coli include a burning feeling while urinating. You might also urinate more often, have cloudy or smelly urine, and pelvic pain in women. Severe cases can cause fever, chills, and flank pain.
Are UTIs more common in certain demographics, and if so, why?
Yes, UTIs are more common in certain groups. Women are more likely to get UTIs because their urethra is shorter. This makes it easier for bacteria to reach the bladder. Older adults and people with certain medical conditions are also at higher risk.
What other bacteria can cause UTIs besides E. coli?
Besides E. coli, other bacteria like Klebsiella pneumoniae and Enterococcus faecalis can cause UTIs. Proteus mirabilis and Staphylococcus saprophyticus are also culprits. Each has its own characteristics and affects different people.
How are UTIs diagnosed, and what role does identifying the causative bacteria play?
UTIs are diagnosed through a combination of clinical evaluation and lab tests, including urine cultures. Knowing the bacteria causing the infection is key to choosing the right antibiotic.
What are the treatment options for UTIs, and how do they target specific bacteria?
Treatment for UTIs usually involves antibiotics. The antibiotic choice depends on the bacteria causing the infection and local resistance patterns. First-line treatments are often used, but new approaches are being explored to fight antimicrobial resistance.
What is antimicrobial resistance, and how does it affect UTI treatment?
Antimicrobial resistance happens when bacteria become resistant to antibiotics. This makes treating UTIs harder, as standard treatments may not work. Alternative antibiotics or treatment strategies are needed.
How can UTIs be prevented, and what practices can reduce the risk of developing a UTI?
To prevent UTIs, drink plenty of water and urinate when needed. Good hygiene and, for some women, urinating after sex can help. Knowing the causes and taking preventive steps can lower your risk of getting a UTI.
References
- Flores-Mireles, A. L., Walker, J. N., Caparon, M., & Hultgren, S. J. (2015). Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nature Reviews Microbiology, 13(5), 269“284.https://www.nature.com/articles/nrmicro3432
- Ghasemian, R., & Naderi, H. R. (2021). Escherichia coli and other bacteria causing urinary tract infections in outpatients and inpatients. Journal of Clinical Medicine, 10(5), 1081.https://www.mdpi.com/2077-0383/10/5/1081


































