
We aim to give you a full understanding of CPPD Arthritis. This condition affects millions of older adults globally. CPPD, or Calcium Pyrophosphate Deposition Disease, is a form of arthritis. It happens when calcium pyrophosphate dihydrate crystals build up in the joints calcium crystal disease.
CPPD disease is often missed because it can look like other arthritis types, like rheumatoid arthritis or gout. Even though it affects 4-7% of people over 60, it’s not well-known as a cause of joint pain.
We will look deeper into its symptoms, how to diagnose it, and treatment options. This will help you understand and manage CPPD Arthritis better.
Calcium Pyrophosphate Deposition Disease, or CPPD, is a form of arthritis. It happens when calcium pyrophosphate dihydrate crystals build up in joints. This can cause pain and swelling in the joints, often seen in older people. We’ll look into what CPPD is, its history, and how it’s different from other diseases.
The term CPPD means Calcium Pyrophosphate Deposition disease. It’s when crystals of calcium pyrophosphate dihydrate form in joint cartilage, causing arthritis. Knowing what CPPD is helps doctors diagnose and treat it better.
CPPD disease was first found in the 1960s. This was a big step in understanding arthritis. Ever after, scientists have been studying CPPD to learn more about it. They’ve found out about its causes, symptoms, and how to treat it.
CPPD disease is different from other arthritis types like osteoarthritis or rheumatoid arthritis. The main difference is the presence of calcium pyrophosphate dihydrate crystals in the joints. This is what makes CPPD unique. Here’s how it differs:

Understanding calcium crystal disease is key to finding effective treatments. We’ll look at how calcium pyrophosphate crystals form and why they cause joint inflammation.
Calcium pyrophosphate crystals form in joints due to age, metabolic disorders, and genetics. They deposit abnormally in cartilage and synovial fluid. This abnormal formation is a major cause of CPPD disease.
The exact reasons for crystal formation are complex. Aging, joint trauma, and metabolic conditions like hyperparathyroidism play a role. Knowing these factors helps us find at-risk individuals and prevent the disease.
Calcium pyrophosphate crystals in joints trigger inflammation, leading to CPPD symptoms. When these crystals enter the synovial fluid, the immune system sees them as foreign. This triggers inflammation. This inflammation causes joint pain, swelling, and stiffness, typical of CPPD disease.
The inflammation is caused by cytokines and chemokines that draw immune cells to the joint. This inflammation can be very painful and limit joint function. Understanding this inflammatory response is vital for creating targeted treatments for CPPD disease.
Studying CPPD shows us who gets it and why. It helps us understand who is most likely to be affected. It also tells us what factors contribute to its development.
CPPD is more common in older adults. Its prevalence increases with age. It’s rare in those under 60 but affects up to 50% of those over 80.
This shows CPPD might be linked to aging and joint degeneration.
Research finds differences in CPPD prevalence among different groups. Some studies suggest a gender difference, with higher prevalence in women or men. Ethnic differences also exist, with some groups more prone to CPPD.
Several risk factors for CPPD have been found. These include metabolic disorders like hyperparathyroidism and hemochromatosis. Genetic factors also increase the risk, with some families more affected.
Joint trauma and certain surgeries also raise the risk of CPPD.
Knowing these risk factors is key to early CPPD detection and management. Healthcare providers can then offer preventive measures and timely interventions.
It’s important to know the different ways CPPD arthropathy shows up. This helps in managing the disease better. CPPD can appear in many forms, so it’s key to recognize them all for proper care.
Asymptomatic chondrocalcinosis is a common form of CPPD disease. It’s when calcium pyrophosphate crystals build up in cartilage but don’t cause symptoms. This is often found by chance during tests for other reasons.
More people get this as they get older. Even though it doesn’t hurt, it’s important to watch these cases. Some might start showing symptoms later.
Acute pseudogout attacks are a sudden and severe form of CPPD disease. They cause intense pain, swelling, and inflammation in the joints. These can be triggered by injury, surgery, or some medicines.
During an attack, the joint looks warm, red, and sore. It can feel like other types of arthritis, like gout. Quick diagnosis and treatment are key to ease the pain and prevent damage.
Some people with CPPD disease get a chronic form. This causes joints to slowly wear down and become deformed. It looks like osteoarthritis but has more inflammation and can affect more joints.
Dealing with chronic CPPD needs a full plan. This includes medicines for inflammation, physical therapy, and sometimes surgery for serious damage.
CPPD disease can also look like rheumatoid arthritis. It has symptoms like morning stiffness and affects joints on both sides of the body. This makes it hard to tell it apart from true rheumatoid arthritis.
Getting the right diagnosis is very important. The treatments for CPPD and rheumatoid arthritis are different. Knowing the exact condition helps doctors give the best care.
Knowing the symptoms of CPPD is key for the right diagnosis and treatment. We will look at the common signs of CPPD. This will help both patients and doctors understand and manage this complex disease.
Joint pain is a main symptom of CPPD, often with swelling. This pain can be mild or very severe. It usually happens in the joint that’s affected.
Swelling happens because of inflammation from calcium pyrophosphate crystals.
Key characteristics of joint pain in CPPD include:
Stiffness, mainly after rest, is another symptom of CPPD. This stiffness can make it hard to move around. We will talk about ways to manage stiffness and improve joint function.
Factors contributing to stiffness include:
CPPD symptoms can look like other arthritis types, like osteoarthritis or rheumatoid arthritis. Getting a correct diagnosis needs a full check-up. This includes looking at your medical history, imaging, and joint fluid analysis.
|
Condition |
Common Symptoms |
Distinguishing Features |
|---|---|---|
|
CPPD |
Joint pain, swelling, stiffness |
Presence of calcium pyrophosphate crystals in joint fluid |
|
Osteoarthritis |
Joint pain, stiffness, limited mobility |
Degenerative changes on X-ray, absence of crystals |
|
Rheumatoid Arthritis |
Symmetrical joint pain, swelling, morning stiffness |
Presence of rheumatoid factor, specific inflammatory markers |
Knowing which joints are affected by CPPD is key for correct diagnosis and treatment. CPPD can show up in many joints across the body. The amount and where the crystals settle can vary a lot from person to person.
The knee is often hit by CPPD. Crystal deposition in the knee can cause a lot of pain and swelling. This can make it seem like other types of arthritis.
Chondrocalcinosis in the knee is when calcium pyrophosphate crystals build up in the cartilage. This can be very painful.
CPPD can also affect the wrist and hand. This can make it hard to grip things and do daily tasks. Radiocarpal joint involvement is common, and crystals can also show up in the triangular fibrocartilage.
The shoulder and hip are also places where CPPD can show up. In the shoulder, it can cause pain and make it hard to move. In the hip, it can lead to a lot of pain and make walking hard.
We should think about CPPD when someone has pain in their shoulder or hip.
Spinal CPPD is rare but serious. Spinal CPPD can cause the cervical spine to become unstable. This can lead to severe neurological symptoms.
We need to watch for this to treat it quickly and properly.
To sum up, here’s a table showing where CPPD can occur and what it can do:
|
Joint |
Common Features |
Clinical Impact |
|---|---|---|
|
Knee |
Chondrocalcinosis, crystal deposition |
Pain, swelling, limited mobility |
|
Wrist and Hand |
Radiocarpal joint involvement, reduced grip strength |
Impaired dexterity, daily activity limitation |
|
Shoulder and Hip |
Pain, limited mobility |
Reduced function, impact on mobility |
|
Spine |
Cervical spine instability, neurological symptoms |
Potential for serious neurological complications |
By knowing how CPPD can affect different joints, we can better diagnose and treat it.
To accurately diagnose CPPD, healthcare providers use a detailed strategy. This strategy looks at all parts of the disease. It leads to a precise diagnosis and a good treatment plan.
A thorough physical exam is key in diagnosing CPPD. Healthcare providers check for signs of joint inflammation. They look for swelling, redness, and warmth in the knees, wrists, and other affected joints.
They also check for joint tenderness and reduced range of motion. During the exam, they may perform specific maneuvers. These help assess joint stability and look for any deformities.
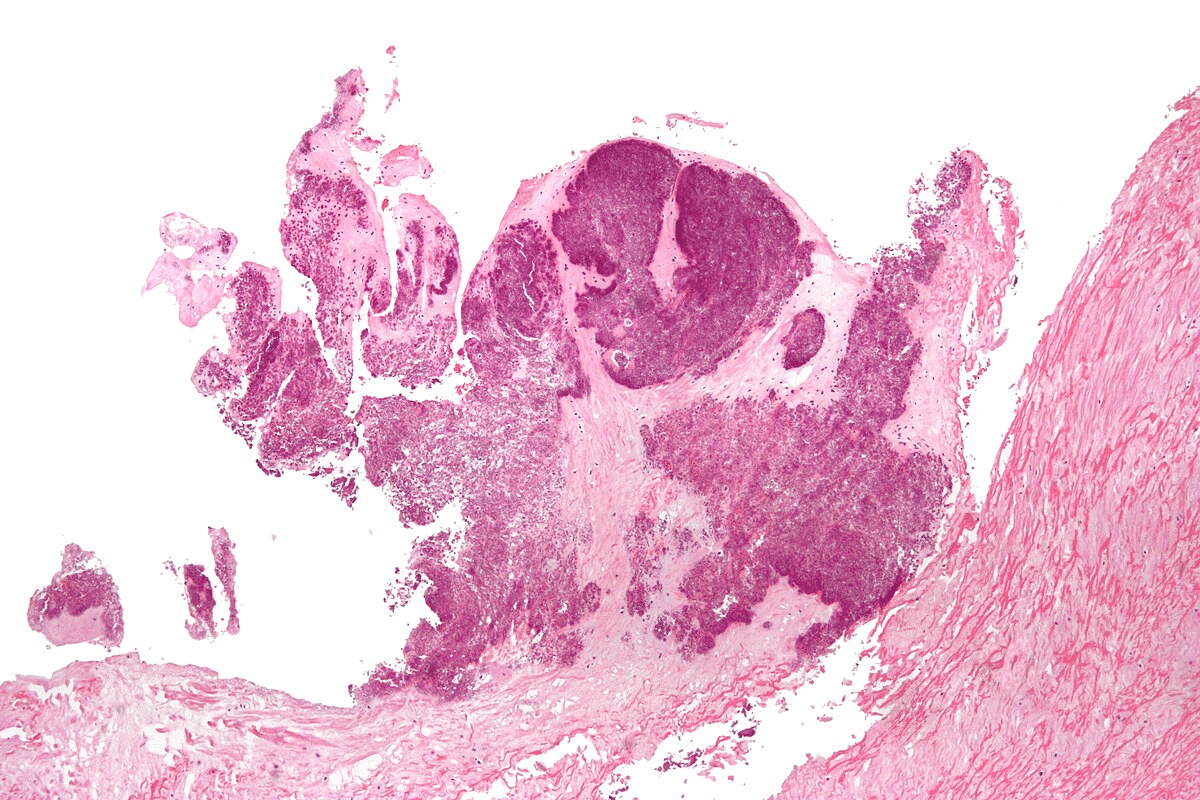
Imaging studies are vital in diagnosing CPPD. X-rays help identify calcification in the cartilage, known as chondrocalcinosis. This is a key sign of CPPD.
Other imaging like ultrasound and MRI are used too. They help assess joint damage and find calcium pyrophosphate crystals.
The definitive diagnosis of CPPD comes from finding calcium pyrophosphate crystals in the joint fluid. This is done through a joint aspiration, or arthrocentesis. Fluid is taken from the affected joint and examined under a microscope.
Seeing positively birefringent rhomboid or needle-shaped crystals under polarized light microscopy confirms CPPD. This test is important for telling CPPD apart from other types of arthritis, like gout or septic arthritis.
It’s important to know the medical conditions linked to CPPD for better treatment. Studies show CPPD often comes with other health problems.
Metabolic disorders are key in CPPD development. Hyperparathyroidism, hemochromatosis, and hypomagnesemia raise CPPD risk.
|
Metabolic Disorder |
Association with CPPD |
|---|---|
|
Hyperparathyroidism |
Increased calcium levels contribute to CPPD |
|
Hemochromatosis |
Iron overload can lead to joint damage and CPPD |
|
Hypomagnesemia |
Low magnesium levels can contribute to CPPD development |
Endocrine diseases, like those affecting calcium and phosphate, are linked to CPPD. Hypothyroidism increases CPPD risk.
We’ll explore the connection between endocrine diseases and CPPD. The relationship between these conditions highlights the complexity of CPPD disease.
Genetics also influence CPPD. Certain genetic mutations increase CPPD risk, mainly in those with a family history.
Aging is a big risk factor for CPPD. Older adults are more likely to get it. Joint degeneration also contributes to calcium pyrophosphate crystal deposition.
Knowing these conditions helps doctors create better treatment plans for CPPD patients.
Managing CPPD disease needs a mix of treatments. We focus on handling acute attacks, long-term plans, and using medicines to ease symptoms and stop future episodes.
Acute CPPD attacks, or pseudogout, need quick treatment to lessen inflammation and pain. Here are some steps we take:
For those with recurring or chronic CPPD, long-term plans are key. We consider the following:
Many medicines are used to manage CPPD, including:
Treatment plans must be tailored to each patient. We consider their specific needs, medical history, and CPPD severity. We work closely with patients to create a treatment plan that fits their unique situation.
Living with Calcium Pyrophosphate Deposition Disease (CPPD) means making lifestyle changes and practicing self-care. Medical treatments are key, but lifestyle changes can also help. They can make symptoms better and improve life quality for CPPD patients.
Keeping joints safe is important for CPPD management. Avoid activities that strain joints too much. Use the right body mechanics and spread out forces when lifting or carrying things.
Gentle exercises and physical therapy keep joints moving and muscles strong. This reduces injury risk.
It’s best to talk to a healthcare professional about an exercise plan that’s right for you.
“Regular exercise is essential for maintaining joint health and overall well-being in patients with CPPD.”
Medical Expert, Rheumatologist
Eating a balanced diet with anti-inflammatory foods helps manage CPPD symptoms. Foods rich in omega-3 fatty acids, antioxidants, and fiber are good choices.
|
Food Group |
Examples |
Benefits |
|---|---|---|
|
Fatty Fish |
Salmon, Sardines |
High in omega-3 fatty acids, reducing inflammation |
|
Fruits and Vegetables |
Berries, Leafy Greens |
Rich in antioxidants, combating oxidative stress |
|
Whole Grains |
Quinoa, Brown Rice |
High in fiber, supporting digestive health |
Using assistive devices and making home changes can help CPPD patients a lot.
Knowing how CPPD arthritis will progress is key to managing it well. The outlook for CPPD disease varies a lot. This depends on how the disease moves and how well treatments work.
CPPD arthritis moves at different speeds for different people. Some see slow changes with few symptoms. Others face quick declines in joint health. Age, metabolic disorders, and genetics play big roles in how fast it moves.
|
Disease Progression Pattern |
Characteristics |
Impact on Quality of Life |
|---|---|---|
|
Slow Progression |
Minimal symptoms, gradual joint degeneration |
Mild impact, manageable with lifestyle adjustments |
|
Rapid Progression |
Frequent acute attacks, significant joint damage |
Significant impact, may require aggressive treatment |
|
Stable Condition |
Little to no progression, occasional flare-ups |
Moderate impact, manageable with treatment and lifestyle |
CPPD can really affect a person’s life. Chronic pain, less mobility, and frequent attacks can mess with daily life and happiness. But, with the right care, many can live well despite the disease.
It’s important for patients to know when to get help. Seek medical help right away for sudden, severe joint pain, swelling, redness, or fever. Regular check-ups with doctors are also key to keeping an eye on the disease and adjusting treatments.
Research on CPPD arthritis is always going on. Scientists are trying to understand the disease better and find new treatments. New treatments might include more precise therapies and new ways to handle crystal buildup. Keeping up with research helps both patients and doctors make better choices.
Living with CPPD disease means taking a full approach. This includes medical treatment, making lifestyle changes, and ongoing care. CPPD, or Calcium Pyrophosphate Deposition Disease, is when calcium pyrophosphate crystals build up in joints. This leads to different types of arthritis.
To manage CPPD well, it’s key to know its symptoms, how it’s diagnosed, and treatment choices. Being proactive in care helps lessen symptoms, boosts quality of life, and slows disease growth.
We’ve seen how important lifestyle changes are for CPPD. This includes protecting joints, exercising, and watching what you eat. Also, keeping up with new research and treatments is vital for the best care.
In conclusion, dealing with CPPD disease needs a plan that covers physical, emotional, and social needs. Working with healthcare providers and focusing on the patient helps. This way, people with CPPD can face the disease’s challenges and live a happy life.
CPPD stands for Calcium Pyrophosphate Deposition disease. It’s a condition where calcium pyrophosphate crystals build up in joints. This leads to inflammation and arthritis.
Symptoms include joint pain, swelling, stiffness, and reduced mobility. These can be either acute or chronic. They might look like other forms of arthritis.
Doctors use a physical exam, X-rays, and joint fluid analysis to diagnose CPPD. They look for calcium pyrophosphate crystals.
Risk factors include getting older, certain metabolic disorders, and endocrine diseases. Genetic predisposition and joint degeneration also play a role.
Treatment for CPPD includes managing acute attacks with medication. Long-term strategies aim to reduce crystal formation. Lifestyle changes also help improve quality of life.
There’s no cure for CPPD. But, treatments and lifestyle changes can manage the condition. They help reduce symptoms and improve life quality.
Managing CPPD involves joint protection, regular exercise, and physical therapy. Dietary considerations and assistive devices also help improve daily functioning.
Yes, CPPD is linked to metabolic and endocrine disorders. Genetic factors also influence its development and progression.
CPPD can affect various joints, like the knee, wrist, hand, shoulder, hip, and spine. Each joint may show different symptoms and severity.
The prognosis for CPPD varies. It depends on disease progression, treatment response, and other health conditions. With proper management, many patients can lead active lives.
CPPD involves calcium pyrophosphate crystals, while osteoarthritis is a degenerative joint disease. Both can cause joint pain and degeneration, but they differ in cause.
Research is ongoing to find new treatments for CPPD. This offers hope for better outcomes and quality of life for patients.
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5107653/
Subscribe to our e-newsletter to stay informed about the latest innovations in the world of health and exclusive offers!