Chondrocalcinosis of the knee is a condition where calcium pyrophosphate dihydrate crystals build up in the cartilage. This can cause joint pain and swelling. It’s also known as calcium pyrophosphate deposition disease (CPPD). This condition affects many people, making it seem like other types of arthritis what is chondrocalcinosis.
At Liv Hospital, we understand how important it is to know about chondrocalcinosis. It can lead to ongoing joint pain and swelling. This can really affect someone’s life quality.
Key Takeaways
- Chondrocalcinosis of the knee involves the accumulation of calcium pyrophosphate dihydrate crystals in the cartilage.
- This condition is also known as calcium pyrophosphate deposition disease (CPPD).
- It can cause joint pain and inflammation, often mimicking other forms of arthritis.
- Effective management is key to reduce symptoms and improve life quality.
- Knowing about chondrocalcinosis is vital for early detection and treatment.
Understanding Chondrocalcinosis of the Knee
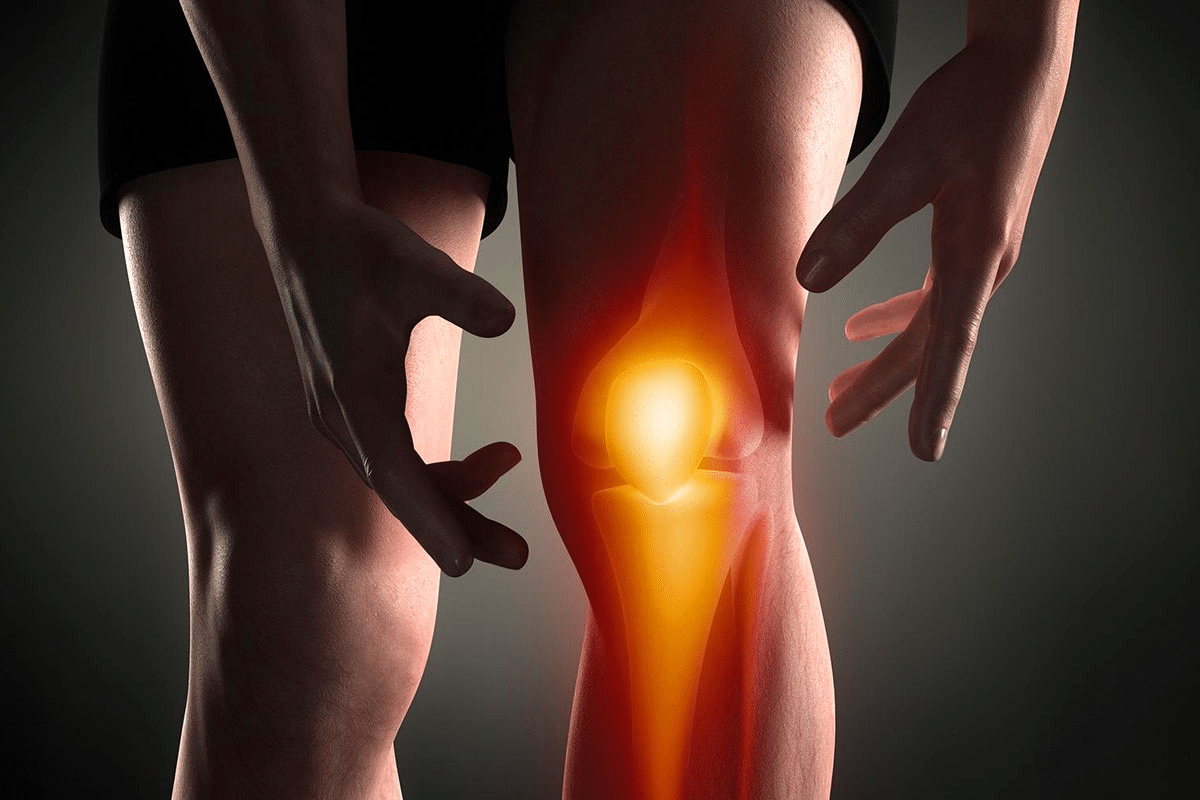
Exploring chondrocalcinosis of the knee, we must understand its causes and effects. This condition happens when calcium pyrophosphate dihydrate (CPPD) crystals build up in the knee cartilage. It causes pain, swelling, and can damage the joint severely.
Definition and Basic Concepts
Chondrocalcinosis of the knee is when CPPD crystals form in the cartilage, mainly in the menisci. It leads to pain, swelling, and makes moving hard. The term “chondrocalcinosis” means “cartilage calcification,” showing what the disorder is about.
This condition is often found by chance on X-rays, showing calcifications in the knee. Knowing about chondrocalcinosis helps in diagnosing and treating it well.
Prevalence and Demographics
Chondrocalcinosis is more common than many think, affecting a lot of people, mainly as they get older. About 1 in 10 people have it, and this number goes up a lot with age.
The Arthritis Foundation says nearly half of people over 85 have chondrocalcinosis. This shows that as we age, our joints can change in ways that lead to this condition.
|
Age Group |
Prevalence of Chondrocalcinosis |
|---|---|
|
Under 60 |
Less than 5% |
|
60-75 |
10-15% |
|
75-85 |
20-30% |
|
85 and older |
Almost 50% |
Historical Background
Our understanding of chondrocalcinosis has grown a lot over time. It was first described in the 1960s as a unique condition different from other arthritis types.
Thanks to better X-rays and finding CPPD crystals in joint fluid, we can diagnose it more accurately. Now, we know it’s a common issue for the elderly, and research is ongoing to understand and manage it better.
The Pathophysiology of Chondrocalcinosis

To understand chondrocalcinosis, we must look at how calcium pyrophosphate dihydrate crystals form and affect the knee. This condition is marked by the buildup of these crystals in the cartilage of joints, mainly in the knee.
Calcium Pyrophosphate Dihydrate Crystal Formation
The growth of calcium pyrophosphate dihydrate crystals is key to chondrocalcinosis. These crystals form when there’s an imbalance in inorganic pyrophosphate metabolism. This imbalance leads to their buildup in cartilage. The crystals irritate the area, causing inflammation and joint damage.
This process involves complex biochemical pathways. It’s influenced by age, metabolic conditions, and genetics. As more crystals build up, they can severely harm the joint tissues.
Areas of the Knee Commonly Affected
Meniscal chondrocalcinosis is a common form of calcium crystal buildup in weight-bearing joints. The menisci, being fibrocartilaginous structures, are more prone to crystal deposition. The menisci are vital for knee function, and their involvement can cause a lot of pain.
Hyaline cartilage and other soft tissues around the knee can also be affected. This contributes to the overall condition of chondrocalcinosis. The condition can cause a range of symptoms, from sudden inflammatory attacks to chronic pain and joint degeneration.
Microscopic Changes in Joint Tissues
Looking at affected joints under a microscope shows significant changes. The buildup of calcium pyrophosphate dihydrate crystals causes cartilage damage and degeneration, along with inflammation. The crystals are found in the cartilage and other joint tissues, leading to irritation and inflammation.
The microscopic changes include the presence of crystals, cartilage degeneration, and an inflammatory reaction. Knowing these changes is key to diagnosing and managing chondrocalcinosis effectively.
What is Chondrocalcinosis? Detailed Explanation
Chondrocalcinosis is a joint condition where calcium pyrophosphate dihydrate crystals build up in the cartilage. This can cause a lot of pain and make it hard to move, often in the knee. We’ll look at how it affects the meniscus and cartilage, and what makes it different.
Meniscal Chondrocalcinosis
Meniscal chondrocalcinosis is when these crystals form in the meniscus of the knee. The meniscus is a cartilage that helps cushion and stabilize the knee. When crystals build up, it can lead to pain and stiffness.
The meniscus is prone to this because of its cartilage and the stress it faces. Research shows it’s common in older adults and often goes with other joint problems.
Articular Cartilage Involvement
Articular cartilage is also affected by chondrocalcinosis. This cartilage is smooth and white, covering the bone ends in joints. When crystals deposit here, it can cause the cartilage to break down, leading to pain and joint problems.
This can make it hard to tell it apart from other conditions like osteoarthritis. It’s important to think of chondrocalcinosis when someone has knee pain, and they’re older.
Distinguishing Features of Knee Chondrocalcinosis
There are a few key signs that help diagnose knee chondrocalcinosis. These include:
- Radiographic Evidence: Imaging can show calcification in the cartilage, confirming chondrocalcinosis.
- Joint Fluid Analysis: Testing the joint fluid can find calcium pyrophosphate dihydrate crystals, which is a sign of chondrocalcinosis.
- Clinical Presentation: Symptoms can range from sudden attacks to ongoing pain.
Knowing these signs is key to diagnosing and treating knee chondrocalcinosis. By recognizing these unique features, doctors can create better treatment plans to help patients feel better.
Common Risk Factors for Developing Knee Chondrocalcinosis
Knee chondrocalcinosis is caused by age, metabolic, and genetic factors. Knowing these risks helps in early diagnosis and treatment.
Age-Related Factors
Getting older is a big risk for knee chondrocalcinosis. It’s more common after 60. Wear and tear on joints leads to calcium crystals, causing the condition.
Metabolic Conditions
Some metabolic issues raise the risk of knee chondrocalcinosis. These include hyperparathyroidism, hypothyroidism, hypomagnesemia, and hemochromatosis. It’s key to manage these conditions to lower the risk.
Genetic Predisposition
Genetics also play a part in knee chondrocalcinosis. People with a family history are more at risk. Genetic predisposition affects the chance of crystals forming in joints.
Previous Joint Injuries and Trauma
Joint injuries or trauma can up the risk of knee chondrocalcinosis. Joint damage from injuries changes the joint, making it more prone to crystals. Knowing about past injuries is key to assessing risk.
Healthcare providers can spot high-risk individuals for knee chondrocalcinosis. They can then take steps to prevent and manage it.
Signs and Symptoms of Chondrocalcinosis
Chondrocalcinosis of the knee can show up in different ways. It can range from no symptoms at all to severe pain and swelling. The way it shows up can vary a lot from person to person, from no signs to intense joint inflammation.
Asymptomatic Presentation
Many people with chondrocalcinosis don’t have any symptoms. They might find out about it by chance during tests for something else. This kind of chondrocalcinosis might not really affect their life much.
Acute Symptoms (Pseudogout)
Some people with chondrocalcinosis get sudden joint pain, swelling, and redness. This is called pseudogout. It can start for many reasons, like an injury or surgery. During a pseudogout attack, the joint gets warm, swollen, and very painful, making it hard to move.
Pseudogout attacks can be very bad and need quick medical help to ease the pain and reduce swelling.
Chronic Symptoms
Chondrocalcinosis can also cause ongoing symptoms. People might feel constant joint pain, stiffness, and trouble moving. These symptoms can get worse over time, making everyday tasks harder.
Common chronic symptoms include:
- Joint pain or aching
- Stiffness, mostly after resting
- Swelling or tenderness around the joint
- Warmth or redness around the joint
- Crackling or popping sounds (crepitus)
When to Seek Medical Attention
If you’re experiencing symptoms of chondrocalcinosis, see a doctor if you notice:
- Sudden severe joint pain or swelling
- Increased redness or warmth around the joint
- Fever with joint symptoms
- Big loss of joint function or mobility
Getting diagnosed and treated early can help manage symptoms and slow the disease.
|
Symptom |
Acute (Pseudogout) |
Chronic |
|---|---|---|
|
Joint Pain |
Severe, sudden onset |
Mild to moderate, persistent |
|
Swelling |
Significant, often with redness |
Mild to moderate |
|
Joint Stiffness |
May occur during episodes |
Common, mostly after rest |
|
Warmth/Redness |
Often present |
Less common |
Diagnosing Chondrocalcinosis of the Knee
Chondrocalcinosis of the knee is often found by accident during tests for other issues. It’s hard to spot because its symptoms are similar to other joint problems.
Radiographic Imaging Findings
X-rays are key in finding chondrocalcinosis. They show calcium in the cartilage, a sign of the condition. X-rays are usually the first test used.
Important signs include:
- Linear calcification in the menisci and cartilage
- Calcium pyrophosphate dihydrate (CPPD) crystals
- Joint space narrowing and degenerative changes
Joint Fluid Analysis
Joint fluid aspiration is the best way to diagnose chondrocalcinosis. It checks the fluid for calcium crystals. This test is key to finding CPPD crystals.
|
Characteristics |
Normal Synovial Fluid |
Chondrocalcinosis |
|---|---|---|
|
Crystal Presence |
No crystals |
CPPD crystals present |
|
White Blood Cell Count |
Low |
Variable, can be elevated |
|
Appearance |
Clear |
Can be turbid |
Advanced Imaging Techniques
While X-rays are enough for a first diagnosis, advanced imaging techniques like MRI and CT scans offer more details. They show how far the disease has spread and any damage to the joint.
Laboratory Tests for Associated Conditions
Tests are done to find metabolic conditions linked to chondrocalcinosis, like hyperparathyroidism or hemochromatosis. These include tests for serum calcium, phosphorus, and iron levels.
By using clinical checks, imaging, and lab tests, we can accurately diagnose chondrocalcinosis. Then, we can create a good treatment plan.
Is Chondrocalcinosis Serious? Complications and Prognosis
It’s important to know how serious chondrocalcinosis is. This condition causes calcium crystals to build up in joints, like the knee. It can lead to many problems.
Short-term Complications
Chondrocalcinosis can cause sudden joint pain and swelling. These attacks can be very painful and need quick medical help. We’ll talk more about how to handle these attacks later.
Long-term Joint Damage
Over time, chondrocalcinosis can damage joints. It can make knee osteoarthritis worse, which hurts joint function. The crystals can also speed up joint wear, causing long-term damage.
Impact on Quality of Life
Chondrocalcinosis can really affect your life. It can make everyday tasks hard because of pain and stiffness. It also has a big emotional impact.
Factors Affecting Disease Progression
Many things can make chondrocalcinosis worse. Age, metabolic issues, and genetics are some of them. Knowing these can help doctors find better ways to treat it.
Chondrocalcinosis can cause serious joint damage and affect your quality of life. By understanding the problems it can cause, doctors can help patients better.
Treatment Options for Knee Chondrocalcinosis
Managing knee chondrocalcinosis needs a mix of treatments to ease symptoms and improve joint function. We’ll look at different ways to handle acute attacks, use medicine, try physical therapy, and consider surgery.
Managing Acute Attacks
When you have a sudden knee chondrocalcinosis attack, the main goal is to lessen pain and swelling. Cold or heat application can help; some people find switching between them works best. Use cold packs wrapped in a towel to avoid skin damage.
Resting the joint and avoiding heavy activities can also help. Sometimes, arthrocentesis (joint aspiration) is done to remove extra fluid and ease joint pressure.
Pharmacological Interventions
There are many medicines to help with knee chondrocalcinosis. Nonsteroidal anti-inflammatory drugs (NSAIDs) are often used to reduce pain and swelling. For severe cases, corticosteroid injections can greatly help by cutting down inflammation in the joint.
- NSAIDs: Good for pain and swelling.
- Corticosteroid injections: Offer quick relief for severe swelling.
- Colchicine: Used for acute attacks, when NSAIDs can’t be used.
Physical Therapy Approaches
Physical therapy is key in managing knee chondrocalcinosis. It helps improve joint movement and strengthens the muscles around it. A physical therapist can create a custom exercise plan to boost flexibility and reduce stiffness.
Strengthening exercises are vital as they support the joint and enhance function. We also suggest low-impact aerobic exercises like swimming or cycling to keep the heart healthy without stressing the joint too much.
Surgical Considerations
If other treatments don’t work well, surgery might be an option. Arthroscopic surgery can remove calcium pyrophosphate dihydrate crystals and fix damaged tissues.
In some cases, joint replacement surgery might be needed if the joint is badly damaged. Deciding on surgery should be done with an orthopedic specialist, considering your health and how bad your condition is.
Living with Chondrocalcinosis: Lifestyle Modifications and Prevention
Managing chondrocalcinosis well needs lifestyle changes and prevention. The right steps can lessen symptoms and slow the disease’s growth.
Exercise Recommendations
Exercise is key for keeping joints mobile and strong. Low-impact activities like swimming, cycling, and yoga are best. They ease joint stress.
- Swimming: Works out the whole body without harming joints.
- Cycling: Boosts heart health and strengthens knee muscles.
- Yoga: Increases flexibility and balance, lowering fall and injury risks.
Dietary Considerations
Eating right is vital for managing chondrocalcinosis. Staying at a healthy weight lessens joint stress and inflammation.
|
Dietary Component |
Benefit |
|---|---|
|
Omega-3 fatty acids |
Reduces inflammation |
|
Antioxidant-rich foods |
Combats oxidative stress |
|
Calcium and Vitamin D |
Supports bone health |
Joint Protection Strategies
Protecting joints from damage is key. Use assistive devices, take breaks, and avoid heavy lifting.
Preventive Measures for High-Risk Individuals
Preventive steps are vital for those at risk of chondrocalcinosis. Regular health checks, watching for metabolic issues, and avoiding joint overuse are important.
“Early intervention and lifestyle adjustments can significantly impact the management of chondrocalcinosis.”
— Medical Expert, Rheumatologist
By making these lifestyle changes and taking preventive steps, people with chondrocalcinosis can live more active and happy lives.
Conclusion: Navigating Life with Knee Chondrocalcinosis
Understanding and managing chondrocalcinosis is vital for a better life. This condition can lead to serious joint damage if not handled right. Early diagnosis and proper care are key to managing it well.
The NHS says managing chondrocalcinosis involves medical treatment and lifestyle changes. This approach helps people live better with the condition. It’s about finding the right balance between treatment and daily life.
Knowing the risks and symptoms is the first step. Getting medical help early can prevent serious problems. Treatment options like medicine, physical therapy, and sometimes surgery help keep joints healthy.
Living with chondrocalcinosis needs a full plan that includes medical care, lifestyle changes, and prevention. We stress the need for a proactive approach. This way, people can enjoy a better quality of life despite the condition.
FAQ
What is chondrocalcinosis of the knee?
Chondrocalcinosis of the knee is a condition where calcium pyrophosphate dihydrate crystals build up in the cartilage. This leads to symptoms that can mimic arthritis.
What are the common symptoms of chondrocalcinosis?
Symptoms can vary. Some people may not feel anything, while others might experience sudden pain or chronic stiffness.
How is chondrocalcinosis diagnosed?
Doctors use X-rays, joint fluid analysis, and other tests to diagnose it. They also look for signs of other conditions.
Is chondrocalcinosis a serious condition?
Yes, it can cause short-term pain and long-term damage. But, with the right care, people can manage it well.
What are the risk factors for developing knee chondrocalcinosis?
Risk factors include age, metabolic conditions, and family history. Previous injuries also play a role.
How is chondrocalcinosis treated?
Treatment includes managing sudden attacks and long-term care. This can include medication, physical therapy, and sometimes surgery.
Can lifestyle modifications help manage chondrocalcinosis?
Yes, making lifestyle changes can help. This includes exercise, diet, and protecting your joints.
What is meniscal chondrocalcinosis?
It’s when calcium pyrophosphate dihydrate crystals build up in the menisci. This is common in chondrocalcinosis.
How does chondrocalcinosis affect the quality of life?
It can cause chronic pain and limit mobility. But, with the right treatment, these effects can be managed.
Can chondrocalcinosis be prevented?
Some risks can’t be avoided, but high-risk individuals can take steps to lower their chances.
References
National Center for Biotechnology Information. Evidence-Based Medical Guidance. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3078229/























