Last Updated on December 2, 2025 by Bilal Hasdemir
For those with complex or long-segment urethral strictures, Stage 1 urethroplasty surgery is a key solution. It involves removing the scarred urethra and lining the defect with graft tissue, usually taken from the mouth. This step is essential for future reconstruction, aiming for the best results.
Medical experts say urethroplasty surgery is the top choice for urethral strictures. Stage 1 urethroplasty is a staged method used for long strictures that require multiple procedures for optimal results.
Key Takeaways
- Stage1 urethroplasty is a critical step in managing complex urethral strictures.
- The procedure involves grafting tissue to create a wide, open urethral plate.
- This staged approach prepares the urethra for possible future reconstruction.
- Urethroplasty is considered the gold standard for treating urethral strictures.
- Multiple procedures may be needed to fix complex strictures.
Understanding Urethral Strictures and Their Treatment
Complex urethral strictures need a detailed treatment plan. This plan must understand the cause and how the condition works. These strictures narrow the urethra, affecting a person’s life quality. They can cause urinary problems and lead to serious issues if not treated.

It’s key to know how urethral strictures work to find good treatments. Complex urethral strictures come from many things like injury, infection, or medical procedures.
Common Causes of Complex Urethral Strictures
There are many reasons for complex urethral strictures. Some common ones are:
- Trauma to the urethra, either from external injury or iatrogenic causes
- Infections, like those from sex or catheters
- Previous surgeries or interventions
- Congenital conditions that affect the urethra
These reasons can make strictures hard to treat. They often need a more detailed plan than simple ones.
When Single-Stage Repairs Are Not Feasible
Not every urethral stricture can be fixed with one surgery. Long or damaged strictures might need a staged treatment. “The initial success/failure-free survival after one-stage urethroplasty is about 77% at 5 years and 58% at 10 years,” showing the need for other plans for complex cases.
We know complex urethral strictures need a custom treatment plan. Knowing the cause and how bad the stricture is helps us choose the best treatment. This could be a staged approach or other advanced methods.
“The complexity of urethral stricture disease demands a tailored approach to treatment, stressing the need for skilled clinicians who can handle urethroplasty’s details.”, healthcare professionals say.
Our method for treating complex urethral strictures includes a full check-up. We look at the patient’s health, the stricture’s details, and the best surgery. This way, we aim for the best results for our patients.
The Fundamentals of Urethroplasty Surgery
Urethroplasty surgery is a complex field. It involves many techniques to fix urethral strictures. The right procedure depends on the stricture’s details, its location, and the patient’s health.
image is to be corrected’
Types of Urethroplasty Procedures
There are several urethroplasty procedures. Each has its own use and benefits. Here are the most common ones:
- Anastomotic Urethroplasty: This method removes the stricture and joins the urethra again.
- Urethroplasty with Buccal Mucosal Graft: It uses a graft from the mouth to make the urethra wider.
- Substitution Urethroplasty: This method replaces the diseased part of the urethra with a graft.
Staged vs. Single-Stage Approaches
Choosing between staged and single-stage urethroplasty depends on the stricture’s complexity and the patient’s health. Single-stage urethroplasty is best for simpler strictures, leading to a quicker recovery. On the other hand, staged urethroplasty is used for more complex cases. It allows for a gradual and controlled repair.
Patient Selection Criteria
Choosing the right patients for urethroplasty is key for success. Several factors are considered:
- The length and location of the urethral stricture.
- The patient’s overall health and surgical risk.
- Previous treatments and their outcomes.
By evaluating these factors carefully, surgeons can customize the urethroplasty procedure. This ensures the best outcome for each patient.
Stage1 Urethroplasty Surgery Steps
Stage 1 urethroplasty is a detailed procedure that needs careful planning and execution. We will explain the key steps from the start to the end of the surgery. This includes the initial check-up, the surgery itself, and how the graft is placed.
Preoperative Evaluation and Planning
Before the surgery, a detailed check-up is done to find out the stricture’s length and where it is. This might involve imaging like retrograde urethrography or cystoscopy. Accurate assessment is key for choosing the right surgery method.
This check-up helps us see how big the urethral stricture is and plan the surgery. We look at the patient’s medical history and any treatments they’ve had before.
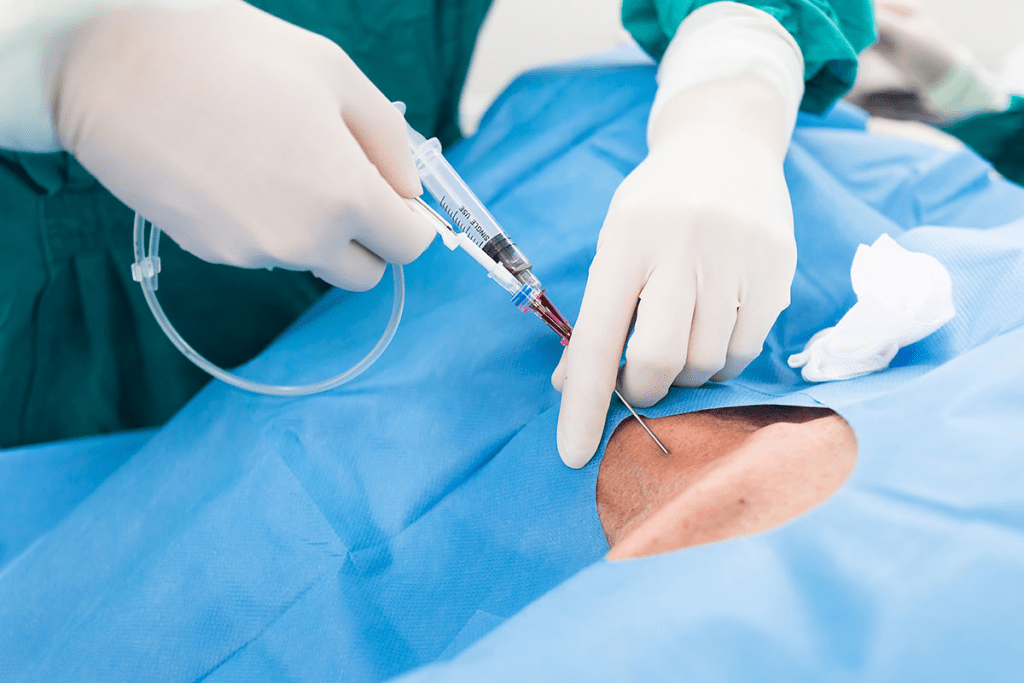
Surgical Technique and Dissection
The surgery for Stage 1 urethroplasty involves carefully cutting through the scarred urethra. The aim is to remove the bad part while keeping as much good tissue as we can. This step is very important for the surgery’s success.
We use special tools to carefully find and remove the stricture. We handle the tissue around it carefully to avoid damage.
image is to be replaced’
Graft Placement and Fixation
After cutting through the urethra, we move on to placing the graft. We use a graft, often from the buccal mucosa, to replace the bad part of the urethra. The graft is carefully fixed in place to help it heal well.
Putting the graft in and fixing it is a precise process. The graft must be the right size and fixed right to help it integrate well and avoid problems.
Urethroplasty with Buccal Mucosal Graft
Urethroplasty with buccal mucosal graft is a top choice for fixing complex urethral strictures. We use it to fix the urethral plate, mainly in staged procedures.
Harvesting the Buccal Mucosa
Getting the buccal mucosa is a key part of urethroplasty. Buccal mucosa is chosen because it’s thick and easy to get. We make sure the process is precise to cut down on risks and help the graft stay healthy.
Advantages of Oral Mucosa in Reconstruction
Oral mucosa, like buccal mucosa, has big benefits for fixing the urethra. It’s well-vascularized and strong, making it perfect for grafts. Using oral mucosa in urethroplasty leads to better results, giving a strong and working urethral plate.
Alternative Graft Materials
Even though buccal mucosal grafts are common, other materials are also used. Options include lingual mucosa and penile skin grafts. The choice depends on the patient’s body and the surgeon’s choice.
We look at each patient’s situation to pick the best graft material for their surgery. Our aim is to get the best results for urethral function and patient happiness.
Recovery and Post-Operative Care
The recovery after Stage 1 urethroplasty is very important. It needs careful management and attention. Good post-operative care helps patients get the best results and prepares them for future treatments.
Immediate Post-Surgical Management
Right after Stage 1 urethroplasty, taking care of the urinary catheter is key. We make sure the catheter is secure and teach patients how to care for it. This helps avoid problems like infections. We also watch for signs of infection, bleeding, or other issues.
Key aspects of immediate post-surgical management include:
- Catheter care and management
- Pain management through medication
- Monitoring for possible complications
A well-known urologist said,
“The success of urethroplasty is not just about the surgery itself but also about the quality of post-operative care. It’s a period that requires vigilance and prompt intervention should any issues arise.”
Long-Term Follow-Up Protocol
After the initial recovery, we start a long-term follow-up plan. This plan helps us check how the healing is going and the health of the urethral plate. We have regular check-ups to see how the graft is doing and the overall health of the urethra.
Regular follow-ups are very important for a few reasons:
- They let us watch the healing process closely.
- They give us a chance to fix any problems early.
- They help us plan for the next stage of the procedure.
Preparing for Stage 2 Procedure
For patients having staged urethroplasty, getting ready for the second stage is key. We check how well the graft has integrated and the urethral plate’s condition. We use advanced tools to check the urethra’s health and decide when to do the next stage.
Getting ready for Stage 2 involves several steps like:
- Checking the graft’s integration and the urethral plate’s health
- Planning the approach for Stage 2
- Telling patients what to expect in the next stage
By managing recovery and post-operative care well, we can greatly improve results for Stage 1 urethroplasty patients. This sets them up for success in future stages of their treatment.
Success Rates and Outcomes
It’s important to know how well Stage1 urethroplasty works. We look at how often it succeeds, what affects its success, and how much experience matters.
Statistical Success Rates Over Time
Research shows that Stage1 urethroplasty works well for most people. Here’s what we’ve found:
- Right after surgery, most people see big improvements.
- Looking back over time, success rates might drop a bit. But overall, it’s good.
- Using grafts from the mouth has helped make it even more successful.
Factors Affecting Surgical Outcomes
Many things can change how well Stage1 urethroplasty works. These include:
- How complicated the stricture is.
- The patient’s health problems.
- The surgery method and what graft is used.
We’ve learned that picking the right patient and doing the surgery carefully are key.
Surgeon Experience and Learning Curve
The surgeon’s skill is a big factor in how well Stage1 urethroplasty goes. Here’s what we’ve discovered:
- More experienced surgeons get better results.
- Learning this surgery is hard and takes a lot of practice.
- Getting better at the surgery and caring for patients helps more people succeed.
Knowing these things helps us set the right expectations and improve care for those getting Stage1 urethroplasty.
Conclusion
We’ve looked into the details of urethroplasty surgery, focusing on Stage1. This is key for handling complex urethral strictures. Staged urethroplasty is a valuable method. It prepares for future repairs.
Using buccal mucosal grafts in urethroplasty has shown good results. We’ve talked about its benefits. Knowing about urethroplasty and Stage1 helps both patients and doctors understand treatment options for urethral strictures.
As we move forward in urethroplasty surgery, staged urethroplasty’s role is vital. It’s a key way to tackle tough cases, leading to better results for patients. Understanding these procedures well is key to top-notch healthcare.
FAQ
What is Stage1 urethroplasty, and why is it necessary?
Stage1 urethroplasty is a surgery for complex urethral strictures. It gets the urethra ready for future repairs. It’s needed when a single repair isn’t possible due to the stricture’s complexity or severity.
What are the common causes of complex urethral strictures?
Complex urethral strictures can come from trauma, infection, or past surgeries. Knowing these causes helps find the best treatment.
How is a patient selected for a staged urethroplasty procedure?
Choosing patients for staged urethroplasty looks at the stricture’s complexity and the patient’s health. Other factors also play a role in success.
What is the role of buccal mucosal grafts in urethroplasty?
Buccal mucosal grafts help in urethral reconstruction. They come from the cheek’s lining. They’re easy to get and match well with urethral tissue.
What are the steps involved in Stage1 urethroplasty surgery?
Stage1 urethroplasty starts with a detailed check-up before surgery. Then, it involves dissecting and placing grafts. The exact steps depend on the case.
How is the buccal mucosa harvested for urethroplasty?
Taking buccal mucosa means surgically removing cheek lining. This is done under anesthesia to reduce pain.
What is the recovery process like after Stage1 urethroplasty?
Recovery includes managing pain and wound care right after surgery. Then, there’s a long-term follow-up to check healing and prepare for the second stage.
What are the success rates for Stage1 urethroplasty?
Success rates for Stage1 urethroplasty vary. They depend on the stricture’s complexity, the surgeon’s skill, and the patient’s health.
How does surgeon experience impact the outcome of urethroplasty?
A surgeon’s experience greatly affects urethroplasty outcomes. More experienced surgeons usually have better results.
What are the alternatives to buccal mucosal grafts in urethroplasty?
Other graft materials might be used instead of buccal mucosal grafts. This depends on the patient’s needs and the surgeon’s choice.
References:
Abd El-Gawad, I., Hassan, E., Abdel Hamid, A., & Farid, M. (2019). Outcome of staged buccal mucosal graft for repair of long segment anterior urethral stricture. BMC Urology, 19(1), Article 66.
- In 123 patients who underwent the first stage of a staged buccal mucosal graft urethroplasty, 105 completed the second stage. Overall success (after both stages) was 79.1% with mean follow-up ~34.7 months. Complications included graft contracture, bleeding, oral numbness. BioMed Central
Long, J., Li, J., Zhang, T., Xu, X., & Zhao, W. (2014). Staged urethroplasty: Comparison of early functional results and quality of life in mesh graft and buccal mucosa technique. Journal of Urology, 191(2), 511-516.
- In a series of 19 patients with staged urethroplasty (mesh graft or buccal mucosa graft), the success rate was 84% at ~11 months follow-up. Some functional complaints (urinary dribbling, changes in sensitivity, etc.) but overall high satisfaction. PubMed
Warner, J., et al. (2021). Long-term outcomes for 2-stage urethroplasty: An analysis of risk factors for urethral stricture recurrence. World Journal of Urology. Advance online publication.
- This study reports very high success rates (≈93-94%) for 2-stage buccal mucosa graft urethroplasty in long strictures, especially when only buccal grafts are used (vs skin grafts), with follow-ups around 3 years. Larger strictures and use of skin grafts are associated with higher recurrence. SpringerLink
Donatucci, C. F., et al. (2007). Buccal mucosa graft urethroplasty for anterior urethral stricture repair: Evaluation of the impact of stricture location and lichen sclerosus on surgical outcome. The Journal of Urology, 178(2), 552-557.
- For anterior strictures repaired using buccal mucosal grafts (including multistage repairs for full-thickness disease), success was ~81% at ~52 months follow-up. Presence of lichen sclerosus reduced success in one-stage repairs, more favorable in multistage settings. AUAA Journals