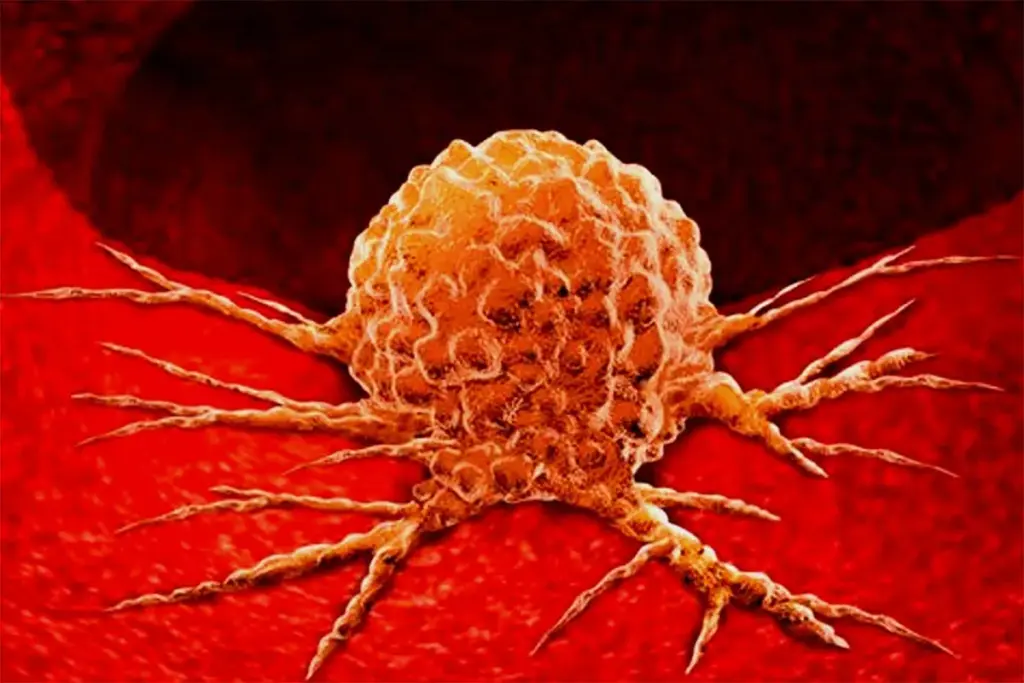
Cancer involves abnormal cells growing uncontrollably, invading nearby tissues, and spreading to other parts of the body through metastasis.
Send us all your questions or requests, and our expert team will assist you.
Targeted therapy is a major advance in cancer treatment, shifting from broad cell destruction to precise molecular targeting. It uses drugs or substances to find and attack specific cancer cells while sparing most normal cells. Unlike traditional chemotherapy, which affects all fast-growing cells, targeted therapies focus on certain molecules involved in cancer growth and spread. This approach is central to precision medicine, which sees cancer as a problem of genes and cell signals rather than just affected organs.
Targeted therapy is based on the idea of oncogene addiction. This means that even though cancer cells have many mutations, they often depend on one main signaling pathway to survive and grow. Blocking this key pathway can stop the cancer. The main drivers are usually proteins that help cells communicate and control their activities. When these proteins are abnormal, they tell the cell to keep dividing or avoid cell death. Targeted drugs are designed to block these signals and stop cancer growth at its source.
Targeted therapy has an advantage over older treatments because it spares the body’s normal, fast-growing cells, like those in the bone marrow and gut. This helps the body keep its ability to repair itself and reduces stress on the patient. There are two main types of targeted therapy: small-molecule inhibitors, which can enter cells and block certain enzymes, and monoclonal antibodies, which are larger proteins that attach to targets on the outside of cancer cells.
The efficacy of targeted therapy is predicated on the precise interruption of intracellular signaling cascades. The most common targets are Tyrosine Kinases, enzymes that function as biological on-off switches. When a growth factor binds to a receptor on the cell surface, tyrosine kinases phosphorylate specific proteins, triggering a cascade of downstream effects that eventually reach the nucleus and initiate cell division. In many cancers, the gene encoding the receptor or the kinase is mutated, keeping the switch in the on position.
Small-molecule tyrosine kinase inhibitors work by blocking the part of the enzyme that uses energy, which turns off the signal for cell growth. Monoclonal antibodies work differently. They can attach to the outside of the receptor to stop growth factors from binding, or they can bind to the growth factor itself and block it in the bloodstream. Some antibodies also help the immune system recognize and destroy cancer cells.
Researchers around the world are working to find more targets for new cancer drugs. Early progress was made with targets like EGFR and HER2, but now scientists are trying to tackle harder targets like KRAS. Using computer modeling, they can design drugs that fit the shapes of mutated proteins. This planned approach is very different from the older, trial-and-error way of finding drugs.
Targeted therapy also changes how we think about the tumor’s surroundings. Some targeted drugs, called angiogenesis inhibitors, block the blood supply to the tumor instead of attacking the cancer cells directly. By stopping new blood vessels from forming, these drugs cut off the tumor’s oxygen and nutrients. This can also help other treatments reach the tumor better and lower the pressure inside the tumor.
Key Physiological Mechanisms Utilized

Send us all your questions or requests, and our expert team will assist you.
Small-molecule inhibitors are tiny chemical compounds that can enter cells to block proteins and enzymes that signal cancer growth. Monoclonal antibodies are large, laboratory-made proteins that cannot enter cells but instead bind to specific targets on the outer surface of cancer cells to block growth signals or alert the immune system.
While targeted therapy is designed to spare healthy cells, it does not always do so. The targets found on cancer cells, such as growth factor receptors, are also present on some healthy cells, though usually in lower numbers. Therefore, targeted drugs can affect healthy cells, causing side effects, but generally with less severity and different patterns than those of chemotherapy.
Oncogene addiction is a theory explaining why targeted therapies work. It suggests that even though a cancer cell has many genetic mutations, it becomes dependent on just one or a few specific abnormal genes (oncogenes) for its survival. If a drug blocks that particular gene or protein, the cancer cell cannot survive and dies.
Targeted therapy only works if the patient’s tumor has the specific genetic mutation or protein target that the drug was designed to attack. If the cancer does not have the target, the drug will have nothing to latch onto and will be ineffective. This is why biomarker testing is essential before starting treatment.
No, they are different. Targeted therapy uses drugs to block specific proteins or genes that drive cancer growth. Gene therapy involves replacing, inactivating, or introducing genes into cells to treat a disease. Targeted therapy acts on gene products (proteins), while gene therapy acts on the genes themselves.


Many people can live with stage 4 cancer for months without obvious signs. Advanced cancers often cause vague symptoms. These symptoms are often mistaken for
Breast cancer diagnosis has changed a lot with new genetic tests. Now, we can give treatments that fit each patient’s genes. The signature test for

Breast cancer diagnosis and treatment rely on specific tumor markers. At Liv Hospital, we focus on three key markers: estrogen receptor (ER), progesterone receptor (PR),
Explore ivermectin cancer clinical trials. Get amazing news on scary treatments and find powerful, vital hope for new rectal therapies. We are seeing a big

When chemotherapy stops working for multiple myeloma, patients face a tough challenge. The disease starts to grow again because it has become resistant. This can

Neuroendocrine tumors (NETs) have long been tough to treat. But, new hope has arrived with the FDA’s approval of cabozantinib, a targeted therapy. This is

Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Leave your phone number and our medical team will call you back to discuss your healthcare needs and answer all your questions.
Your Comparison List (you must select at least 2 packages)