Cancer involves abnormal cells growing uncontrollably, invading nearby tissues, and spreading to other parts of the body through metastasis.
Send us all your questions or requests, and our expert team will assist you.

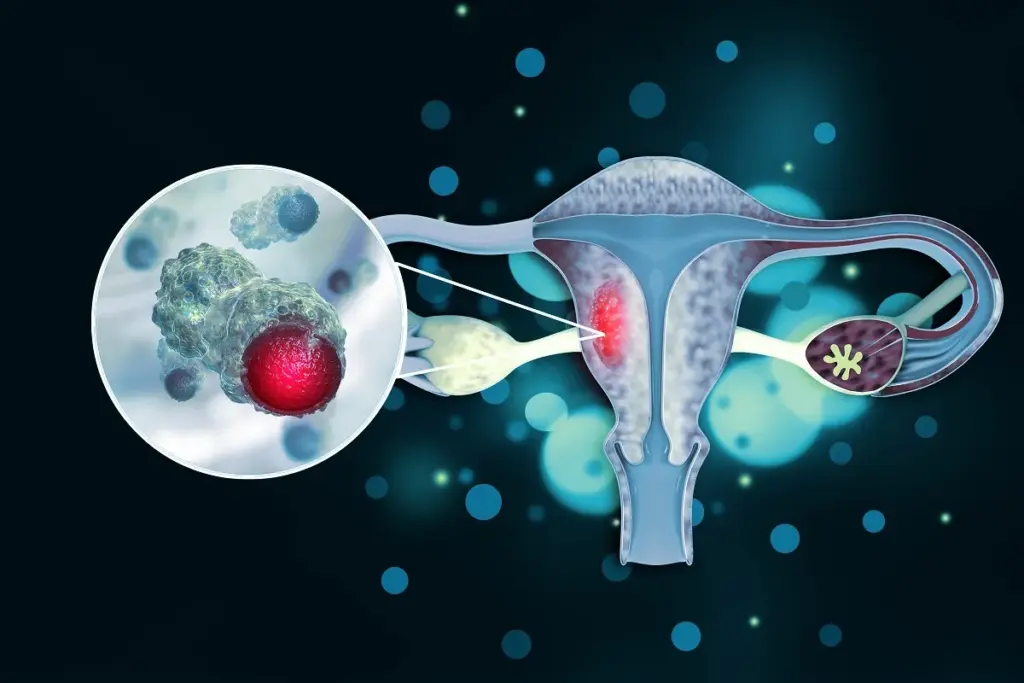
The vulva is the external part of the female genitalia and includes the mons pubis, labia majora, labia minora, clitoris, vaginal vestibule, and glands such as the Bartholin and Skene glands. Vulvar cancer refers to cancer that starts in any of these tissues. Although it is less common than cervical or endometrial cancer, vulvar cancer has its own unique features, often involving chronic skin inflammation, viral infections, and changes in the skin’s protective layer as women age.
Most cases of vulvar cancer are squamous cell carcinoma, which starts in the surface layer of the vulva. Today, doctors recognize two main types: one caused by high-risk human papillomavirus (HPV) infection, and another that develops without HPV, often in women with chronic skin conditions like Lichen Sclerosus. This distinction is important because it affects the cancer’s genetics, the age group it affects, and how it is treated.
Vulvar cancer also includes less common types, such as vulvar melanoma (from pigment cells), extramammary Paget disease (a rare skin cancer likely starting in sweat glands), and Bartholin gland carcinoma (from mucus-producing glands near the vaginal opening). Each type has its own causes and behaviors, so understanding vulvar cancer requires knowledge from several medical fields, including dermatology and gynecology.
The type of cell where vulvar squamous cell carcinoma begins determines how the cancer behaves. There are two main pathways: one linked to HPV infection and one that is not. The HPV-related type is connected to high-grade precancerous changes and involves viral proteins that disrupt normal cell controls, leading to uncontrolled growth. This type usually affects younger women and often has a basaloid or warty appearance under the microscope.
Conversely, the HPV independent pathway is associated with Differentiated Vulvar Intraepithelial Neoplasia. This precursor lesion is frequently subtle and challenging to diagnose but possesses a high potential for malignant transformation. It arises in the context of chronic inflammatory conditions, most notably Lichen Sclerosus. From a regenerative biology perspective, chronic inflammation creates a hostile microenvironment characterized by oxidative stress and continuous cycles of tissue injury and repair. This accelerates the rate of spontaneous mutation, particularly in the TP53 tumor suppressor gene. The resulting carcinomas are typically keratinizing, affect older women, and are often more aggressive and resistant to therapy than their viral counterparts.
Molecular Drivers and Genomic Signatures

The progression of vulvar cancer is not solely determined by the tumor cells but by their interaction with the surrounding stroma. The vulvar microenvironment is rich in immune cells, fibroblasts, and blood vessels. In invasive carcinoma, the basement membrane, the critical barrier separating the epithelium from the deeper tissues, is breached. This invasion is facilitated by the secretion of matrix metalloproteinases, enzymes that degrade the extracellular matrix. The tumor cells undergo an Epithelial to Mesenchymal Transition, losing their adhesive properties and gaining the ability to migrate through the stroma and access lymphatic channels.
Researchers are studying how vulvar cancer interacts with the immune system. The tumor can avoid being attacked by attracting certain immune cells that suppress the body’s defenses and by producing proteins like PD-L1 that block immune responses. This is important for developing new treatments like immunotherapy. In cancers not caused by HPV, especially those linked to Lichen Sclerosus, ongoing inflammation can actually help cancer develop instead of stopping it.
The concept of epithelial plasticity is central to understanding vulvar carcinogenesis. The stratified squamous epithelium of the vulva is constantly regenerating, driven by a population of stem cells in the basal layer. In cancer, these stem cells are corrupted. The chronic inflammatory milieu of Lichen Sclerosus acts as a mutagenic pressure cooker, selecting for stem cell clones that have acquired survival advantages, such as p53 mutations. These cancer stem cells are resistant to standard therapies and are responsible for the high rates of local recurrence seen in vulvar cancer.
Regenerative medicine offers potential avenues for mitigating the damage caused by the disease and its treatment. Research into bioengineered skin grafts and mucosal equivalents aims to improve reconstructive outcomes after vulvectomy. Furthermore, understanding the signaling pathways that maintain the stem cell niche could lead to differentiation therapies that force the cancer cells to mature and stop dividing, rather than simply killing them with cytotoxic drugs. This moves the definition of treatment from destruction to reprogramming.
The interaction between HPV and the host immune system defines a significant portion of vulvar cancer epidemiology. The virus infects basal keratinocytes and uses the cell’s machinery to replicate. In most individuals, the immune system clears the infection. However, in a subset of women, particularly those with compromised immunity or specific genetic susceptibilities, the virus persists. This persistence leads to the integration of the viral genome into the host DNA, a catastrophic event that initiates the oncogenic cascade. The viral oncoproteins E6 and E7 not only drive proliferation but also inhibit the production of interferon, a key antiviral cytokine, effectively blinding the immune system to infected cells. This viral stealth mechanism is a key target for therapeutic vaccines currently under development.
Send us all your questions or requests, and our expert team will assist you.
VIN, or Vulvar Intraepithelial Neoplasia, is a precancerous condition where abnormal cells are found on the surface of the vulva but have not invaded into the deeper tissues. Vulvar cancer occurs when these abnormal cells break through the basement membrane and invade the underlying connective tissue, gaining the potential to spread to lymph nodes and other organs.
Lichen Sclerosus is a chronic inflammatory skin condition that causes thinning, whitening, and itching of the vulvar skin. While it is not cancer, the long-term inflammation and scarring associated with untreated Lichen Sclerosus significantly increase the risk of developing differentiated VIN and subsequently HPV independent squamous cell carcinoma of the vulva.
The Human Papillomavirus can cause both cancers. Women who have a history of cervical cancer or high-grade cervical dysplasia have a higher risk of developing HPV associated vulvar cancer because the same viral risk factor affects the entire lower genital tract, a concept known as the field effect.
The Bartholin glands are two small organs located under the skin near the opening of the vagina that produce mucus to lubricate the area. Although rare, cancer can develop in these glands, which is often mistaken initially for a benign cyst or abscess due to its location and swelling.
While vulvar cancer is traditionally a disease of postmenopausal women, the incidence in younger women is rising due to the increasing prevalence of HPV infection. The HPV-associated type tends to affect younger women, while the HPV independent type associated with chronic skin conditions typically affects older women.
