Urologist meaning explained with focus on minimally invasive urology procedures that transform care.
Minimally invasive urology procedures have changed the game in urology surgery. They offer a safer and more effective way than old-school open surgery. These new methods let urologists fix specific problems with little harm to the body.
GreenLight laser surgery is a great example. It works well for treating Benign Prostatic Hyperplasia (BPH) and keeps working well over time. By defining urology and knowing what urologists do, patients can see the good in these modern methods.
Key Takeaways
- Minimally invasive urology procedures reduce recovery time and scarring.
- GreenLight laser surgery is effective in treating BPH.
- These procedures offer a safer alternative to traditional surgery.
- Urologists use advanced techniques to minimize disruption.
- Patients benefit from robust long-term outcomes.
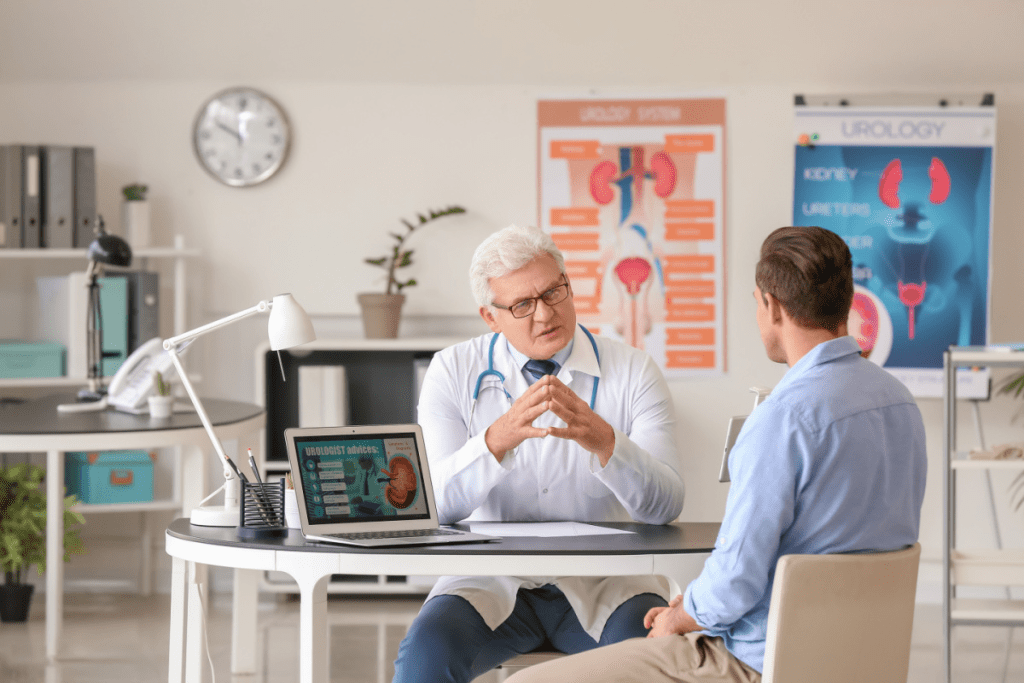
The Meaning of Urology and Urologist in Modern Medicine
Urology is a key part of modern medicine. It deals with the urinary system and male reproductive organs. It helps millions of people worldwide with various health issues.
A urologist is a doctor who focuses on the urinary and male reproductive system. They use both medicine and surgery to treat patients.
Defining the Urologist’s Role and Specialization
Urologists get a lot of training. They handle issues like kidney stones and prostate cancer. They also do urologic surgery when needed.
- They diagnose and treat urinary tract infections and disorders.
- They perform surgery for kidney stones and prostate problems.
- They manage male reproductive health, including infertility and sexual issues.
Common Urological Conditions Requiring Surgical Intervention
Many urological conditions need surgery. These include:
- Kidney stones, which might be removed or broken down with laser lithotripsy.
- Prostate cancer, which could require removing the prostate gland.
- Bladder cancer, which might need the tumor or the whole bladder removed.
It’s important to know about what urology is and the role of urologists. This helps patients understand their treatment options. Urology procedures range from small surgeries to open surgeries, based on the condition and the patient’s health.
In modern medicine, surgical urology keeps getting better. New technology makes urology procedures more effective and less invasive. This leads to better results and faster recovery times.
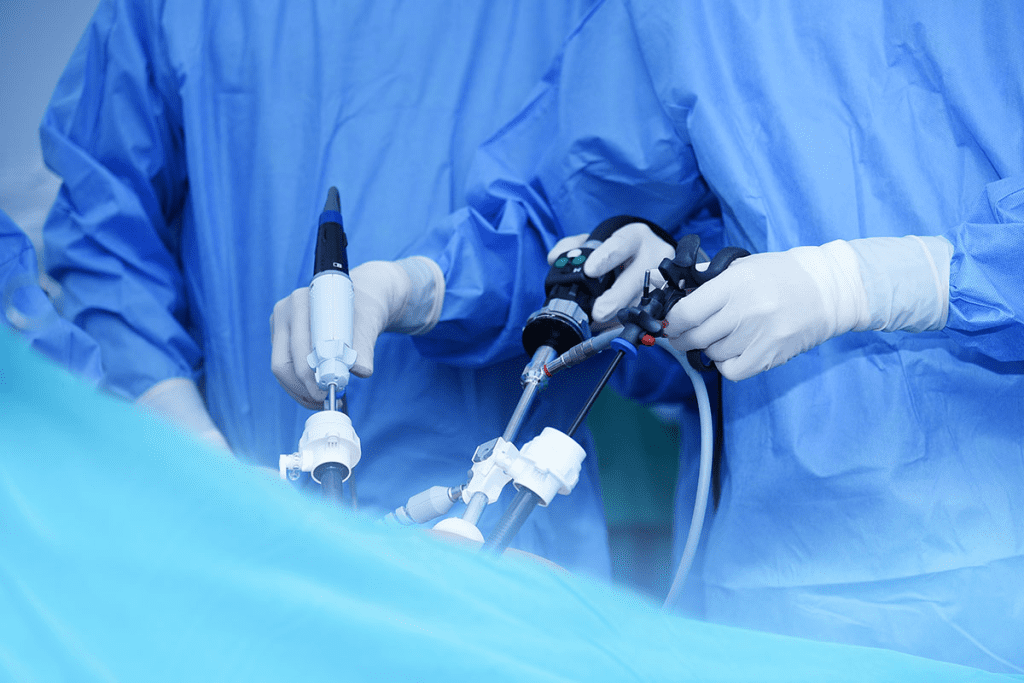
Understanding Minimally Invasive Urologic Surgery
Urologic surgery has changed a lot with new, less invasive methods. These new ways of doing surgery are better for patients. They use small cuts instead of big ones like in old surgeries.
Traditional vs. Minimally Invasive Approaches
Old surgeries need big cuts to get to the problem area. But minimally invasive surgery uses tiny cuts. It lets doctors use tools and a camera to work inside without causing too much damage.
Choosing between old and new surgical methods changes how you feel and recover. People with the new surgery feel less pain and stay in the hospital less. This is because the new way is gentler.
Key Benefits of Minimally Invasive Techniques
There are many good things about the new surgery methods:
- Less time to get better
- Less pain after surgery
- Smaller cuts mean less scarring
- Less chance of problems compared to the old surgery
- Staying in the hospital for less time
These benefits come from better technology and skills. Knowing about these new surgeries helps patients choose the best treatment for them.
GreenLight Laser Surgery for Benign Prostatic Hyperplasia
GreenLight laser surgery is a new way to treat Benign Prostatic Hyperplasia (BPH) in men. It’s a urological surgery that’s less invasive and has fewer side effects. This makes it a big step forward in surgical urology.
The surgery uses a laser to remove extra prostate tissue that blocks urine flow. It’s done through a cystoscope, which goes through the urethra. This means no big cuts are needed.
Photoselective Vaporization of the Prostate (GLPVP) Explained
GLPVP uses the GreenLight laser to vaporize prostate tissue. The laser targets the tissue’s hemoglobin, removing it safely. This method helps patients recover quickly and lowers the risk of complications.
Evolution of GreenLight Laser Technology: From Early Models to 180-Watt Systems
GreenLight laser tech has gotten much better over time. The first versions have turned into 180-Watt systems. These newer systems work faster and can handle bigger prostates, making the treatment better.
This progress in surgical urology shows how far we’ve come. It gives urologists better tools to treat BPH. Now, GreenLight laser surgery is a top choice for many.
Success Rates and Long-term Outcomes
Research shows GreenLight laser surgery works well for BPH. Patients see big improvements in their urine flow and feel better overall. The surgery’s minimally invasive nature makes patients very happy with the results.
The benefits of GreenLight laser surgery last a long time. Many patients stay symptom-free for years. The option to do it again if needed makes it a reliable long-term solution for BPH.
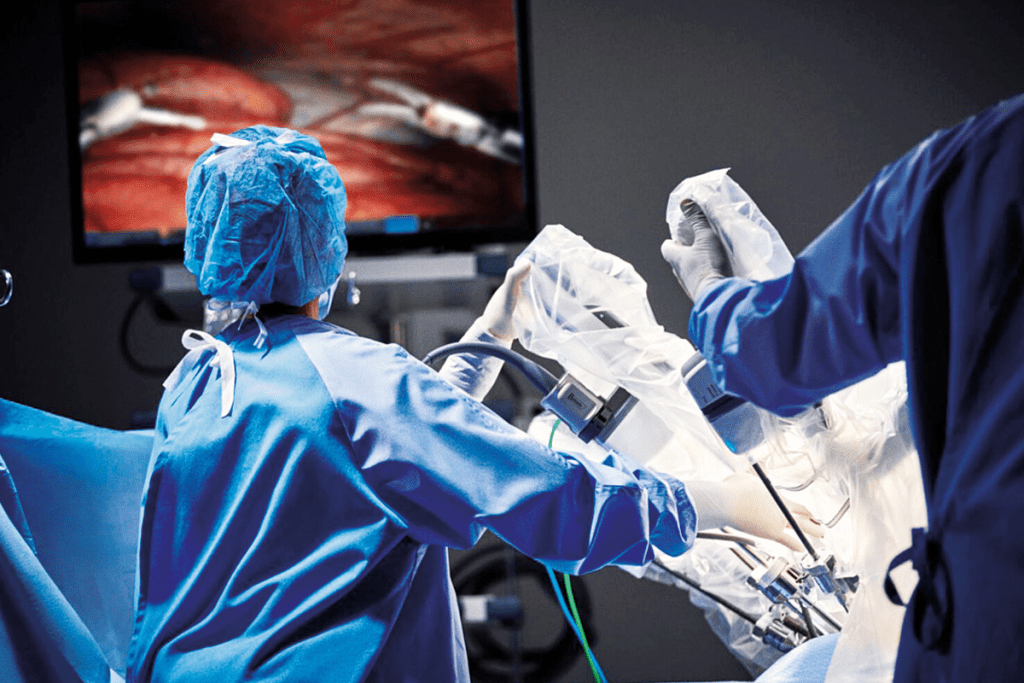
Robotic-Assisted Laparoscopic Procedures in Urology
Robotic-assisted laparoscopic procedures are changing urology. They bring better precision, less blood loss, and quicker recovery than old surgery methods.
Robotic tech in urology, known as “uro-surg,” lets surgeons do complex surgeries better. This tech has greatly helped treat many urological issues.
Robotic Prostatectomy for Prostate Cancer
Robotic prostatectomy is a new way to treat prostate cancer. It removes the prostate gland with a robotic system. This system offers clear 3D views and precise control.
“Robotic-assisted laparoscopy in prostatectomy leads to less pain and quicker recovery,” a top urologist says.
Robotic Partial Nephrectomy for Kidney Conditions
Robotic partial nephrectomy is key in urology. It removes part of the kidney with a tumor or issue, keeping the rest safe.
- It’s minimally invasive, causing less damage.
- It lowers the risk of problems.
- Patients recover faster
Advantages Over Traditional Laparoscopy
Robotic-assisted laparoscopy beats traditional laparoscopy in many ways. It offers:
- Better precision and control
- Clearer 3D views for surgeons
- Less strain on surgeons, helping them work longer
Robotic-assisted laparoscopy is changing urology. It gives patients safer, more effective treatments for many conditions.
Endoscopic and Laser Treatments for Urinary Tract Stones
New medical technologies have brought endoscopic and laser treatments for urinary tract stones. These methods are key in urology surgery, helping manage stones well.
Urinary tract stones, or kidney stones, can be very painful. They can also cause serious problems if not treated quickly. Thanks to urology, endoscopic and laser treatments are now major tools. A study on the National Center for Biotechnology Information (NCBI) website shows they work well and are safeurology treatments.
Ureteroscopy with Laser Lithotripsy
Ureteroscopy with laser lithotripsy is a small procedure for ureter or kidney stones. A tiny scope is put through the urethra and bladder into the ureter. Then, a laser breaks the stone into small pieces that can pass out of the body.
This method has many benefits:
- It’s minimally invasive, so recovery time is shorter
- It has a high success rate in removing stones
- It has fewer risks than traditional surgery
Percutaneous Nephrolithotomy
Percutaneous nephrolithotomy (PCNL) is used for larger kidney stones. It makes a small cut in the back and uses a nephroscope to remove or break up the stone.
PCNL is best for:
- Large stones that other methods can’t handle
- Stones causing blockages or infections
- Patients who haven’t responded to other treatments
Extracorporeal Shock Wave Lithotripsy
Extracorporeal shock wave lithotripsy (ESWL) is a non-invasive way to treat kidney stones. It uses shock waves to break stones into smaller pieces that can be passed in urine.
ESWL is good for:
- Small to medium-sized stones
- Stones in the kidney or upper ureter
In summary, endoscopic and laser treatments have greatly improved the treatment of urinary tract stones. They offer effective, less invasive options. Knowing about these treatments is key to understanding urology and its role in today’s medicine.
Minimally Invasive Therapies for Urinary Incontinence and Pelvic Floor Disorders
Minimally invasive therapies have changed how we treat urinary incontinence and pelvic floor disorders. These issues can really affect a person’s life, causing discomfort and embarrassment. New surgical methods are now available, which are less invasive and lead to quicker recovery times.
Sacral Neuromodulation
Sacral neuromodulation is a new way to treat urinary incontinence and pelvic floor disorders. It involves putting a device in the body to help control the bladder. This method works well for those with an overactive bladder and urinary retention.
Benefits of Sacral Neuromodulation:
- Minimally invasive procedure
- Reversible treatment
- Significant improvement in symptoms for many patients
Botox Injections for Overactive Bladder
Botox injections are now used to treat an overactive bladder. Injecting Botox into the bladder muscle helps reduce the need to urinate often. This treatment is done in a clinic and has a quick recovery time.
As noted by a leading urologist, “Botox injections offer a safe and effective solution for patients suffering from overactive bladder, significantly improving their quality of life.”
Minimally Invasive Sling Procedures
Minimally invasive sling procedures help with stress urinary incontinence. They involve placing a supportive sling under the urethra to stop leaks. The sling can be put in using different methods, like the transobturator and retropubic approaches.
The benefits of these sling procedures include:
- Short procedure time
- Minimal discomfort
- Quick recovery
Urologists are key in diagnosing and treating urinary incontinence and pelvic floor disorders. Knowing what urologists do and the treatments they offer helps patients make better choices for their care.
Advancing Patient Care Through Minimally Invasive Urology
Minimally invasive urology has changed how we treat urological issues. It offers patients effective and less invasive options. Knowing what a urologist does and what urology means helps us see these advances.
Urologists deal with urinary tract and male reproductive system problems. They diagnose, treat, and manage these issues. This shows how urology is key in today’s medicine.
These new techniques have made treatments better. They cut down recovery times and lower risks. For example, GreenLight Laser Surgery and robotic surgeries help with prostate issues.
By knowing what urologists do, patients can choose better care. This knowledge helps them make informed decisions.
Medical tech keeps getting better, and urology will benefit a lot. Minimally invasive methods have set new care standards. They highlight urology’s role in keeping us healthy.
FAQ
What is urology?
Urology is a branch of medicine. It deals with the diagnosis, treatment, and surgery of disorders related to the urinary tract and male reproductive system.
What do urologists do?
Urologists are medical doctors. They specialize in the diagnosis, treatment, and surgery of disorders related to the urinary tract and male reproductive system. This includes conditions like kidney stones, prostate issues, and urinary incontinence.
What is minimally invasive urology?
Minimally invasive urology uses small incisions and advanced technology. It is used to diagnose and treat urological conditions. This approach results in less trauma to the body and faster recovery times.
What is GreenLight laser surgery?
GreenLight laser surgery is a minimally invasive procedure. It is used to treat Benign Prostatic Hyperplasia (BPH). A laser is used to vaporize excess prostate tissue, relieving symptoms such as urinary obstruction.
What are the benefits of robotic-assisted laparoscopic procedures in urology?
Robotic-assisted laparoscopic procedures offer improved precision and reduced blood loss. They also result in faster recovery times compared to traditional open surgery. This makes them an attractive option for patients undergoing procedures such as prostatectomy or partial nephrectomy.
What is ureteroscopy with laser lithotripsy?
Ureteroscopy with laser lithotripsy is a minimally invasive procedure. It is used to treat urinary tract stones. A small scope is inserted through the urethra to locate the stone. A laser is then used to break it up into smaller fragments that can be easily passed out of the body.
What is sacral neuromodulation?
Sacral neuromodulation is a minimally invasive therapy. It is used to treat urinary incontinence and pelvic floor disorders. A device is implanted to stimulate the sacral nerves, helping to regulate bladder function.
What is the difference between traditional and minimally invasive urologic surgery?
Traditional urologic surgery involves larger incisions and more tissue trauma. This results in longer recovery times and more post-operative pain. Minimally invasive urologic surgery uses smaller incisions and advanced technology. It reduces trauma and promotes faster healing.
What are the advantages of minimally invasive sling procedures?
Minimally invasive sling procedures are used to treat urinary incontinence. They offer advantages such as reduced post-operative pain, shorter recovery times, and improved outcomes compared to traditional sling procedures.
What does invasive surgery mean?
Invasive surgery refers to surgical procedures that involve making incisions or inserting instruments into the body. It is used to diagnose or treat a condition. This often results in tissue trauma and longer recovery times.
What is urologic surgery?
Urologic surgery refers to surgical procedures performed to diagnose and treat disorders related to the urinary tract and male reproductive system. This includes conditions such as kidney stones, prostate issues, and urinary incontinence.
What are urology procedures?
Urology procedures include a range of diagnostic and therapeutic interventions. This includes surgery, endoscopy, and laser treatments. They are used to diagnose and treat disorders related to the urinary tract and male reproductive system.
References
- Porto, B. C., Benedicto, B. C., Constantinou, B. T., Hobaica, N. C., Passerotti, C. C., de Lima, R. D., & Sanderberg, R. A. S. (2025). GreenLight photoselective laser vaporisation versus transurethral resection of the prostate for large prostates: systematic review and meta-analysis. Translational Andrology and Urology.https://pubmed.ncbi.nlm.nih.gov/40529031/
- Annals of The Royal College of Surgeons of England. (2014). Durability and complications of photoselective vaporisation of the prostate with the 120W high performance system GreenLight laser. Annals of The Royal College of Surgeons of England.https://publishing.rcseng.ac.uk/doi/10.1308/003588414X13946184901047


































