Last Updated on November 26, 2025 by Bilal Hasdemir
Chemotherapy is a challenging treatment that affects millions of people worldwide. It raises big questions about daily life during treatment. One key concern is whether it’s safe to drink alcohol and go out while on chemotherapy. Understanding Alcohol and Social Activities During Chemotherapy helps patients make informed choices and maintain a balanced lifestyle during treatment.
It’s important for patients to know about alcohol consumption during chemotherapy. Some might wonder if it’s okay to drink alcohol while on chemotherapy. Others worry about how treatment affects their social lives.
This article aims to clear up these questions. We’ll look at precautions patients should take and guidelines for getting back to normal activities after treatment.
Key Takeaways
- Understand the risks associated with alcohol consumption during chemotherapy.
- Learn about the precautions to take when going out during treatment.
- Discover guidelines for safely resuming social activities after chemotherapy.
- Explore the impact of chemotherapy on daily life and social interactions.
- Find out when it’s safe to drink alcohol after chemotherapy treatment.
The Impact of Chemotherapy on Your Daily Life

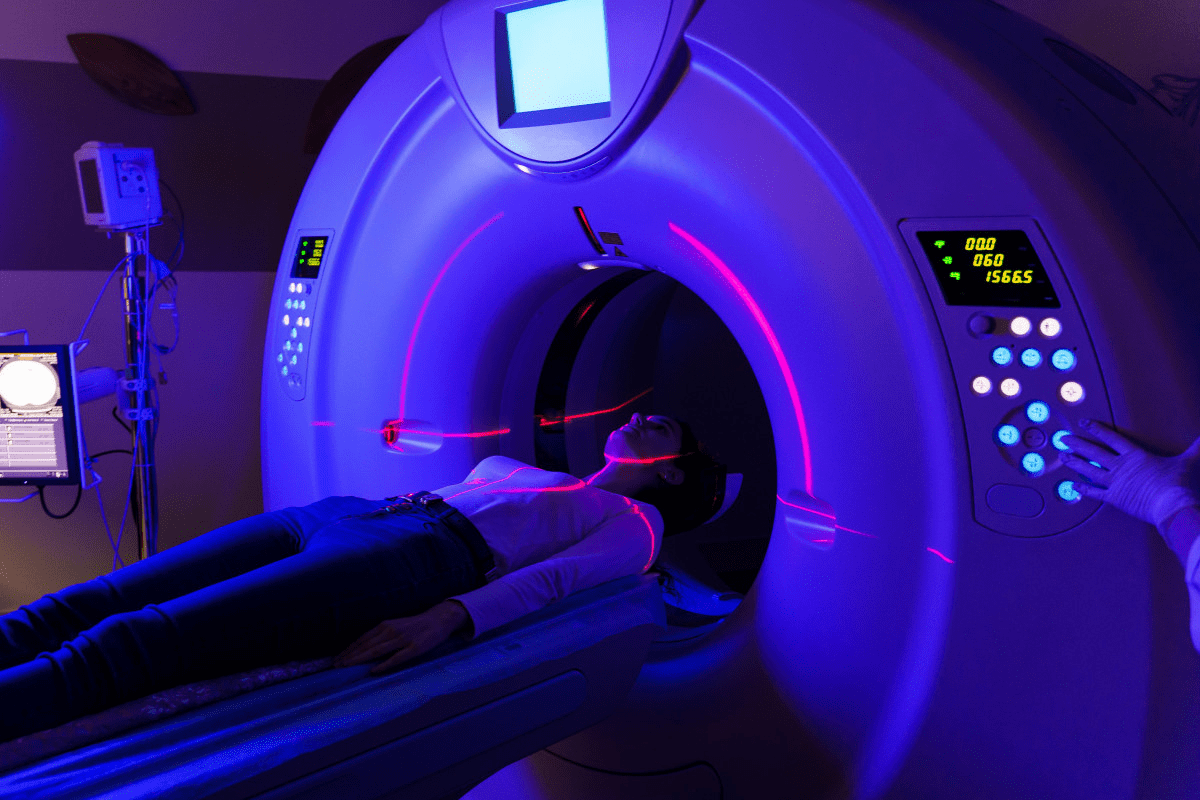
When you’re going through chemotherapy, it changes your daily life a lot. This treatment targets cancer cells but also affects other fast-growing cells in your body. This leads to different side effects.
How Chemotherapy Affects Your Immune System
Chemotherapy can weaken your immune system. It lowers the number of white blood cells, which fight infections. This is called neutropenia and makes you more likely to get sick.
Key precautions include:
- Avoiding crowded places and events where you might be exposed to infections
- Practicing good hygiene, such as frequent handwashing
- Avoiding close contact with people who are sick
- Staying up to date with recommended vaccinations
Common Side Effects That May Limit Social Activities
Chemotherapy can make it hard to do things with friends. Some common side effects are:
- Fatigue: Feeling extremely tired and lacking the energy to participate in activities
- Nausea and vomiting: Experiencing stomach discomfort that can make eating and social dining challenging
- Hair loss: Losing hair, which can affect self-esteem and confidence in social settings
Knowing about these side effects helps you plan better. You can adjust your social plans to keep your quality of life good during treatment.
It’s also important to think about drinking alcohol while on chemotherapy. Alcohol can mix badly with chemotherapy drugs. It might make side effects worse or make treatment less effective. So, it’s best to avoid drinking alcohol during this time.
Social Activities During Chemotherapy: What’s Safe?
It’s important for patients to know what social activities are safe during chemotherapy. This helps them keep their social life going while they’re getting treatment. Chemotherapy not only fights cancer but also affects the patient’s health, so being careful about who they meet is key.
Balancing Social Life and Treatment Requirements
It’s important to balance social life with treatment needs. Patients should rest and recover when needed but also keep in touch with friends and family. This is good for their mental health.
- Plan social activities around treatment schedules to avoid exhaustion.
- Choose low-risk social settings that minimize exposure to infections.
- Communicate with friends and family about your needs and limitations.
Risk Assessment for Different Social Settings
Not all social settings are the same for patients getting chemotherapy. Crowded places like public transportation, shopping malls, or concert venues are high-risk because they increase the chance of getting sick.
- Avoid crowded areas and opt for less crowded times when out.
- Wear a mask in crowded or enclosed spaces to reduce infection risk.
- Practice good hygiene, such as frequent hand washing.
It’s also important to think about who you’re around. Chemotherapy precautions for family members at home include keeping clean and not getting too close when you’re not feeling well.
Having visitors can be nice, but it’s important to talk about health and boundaries. The decision to have visitors depends on your health and theirs.
- Limit visitors when you’re undergoing intense treatment phases.
- Ask visitors to wash their hands and avoid close contact if they’re sick.
- Consider virtual visits as an alternative when in-person visits are not advisable.
How Long After Chemotherapy Can You Drink Alcohol?
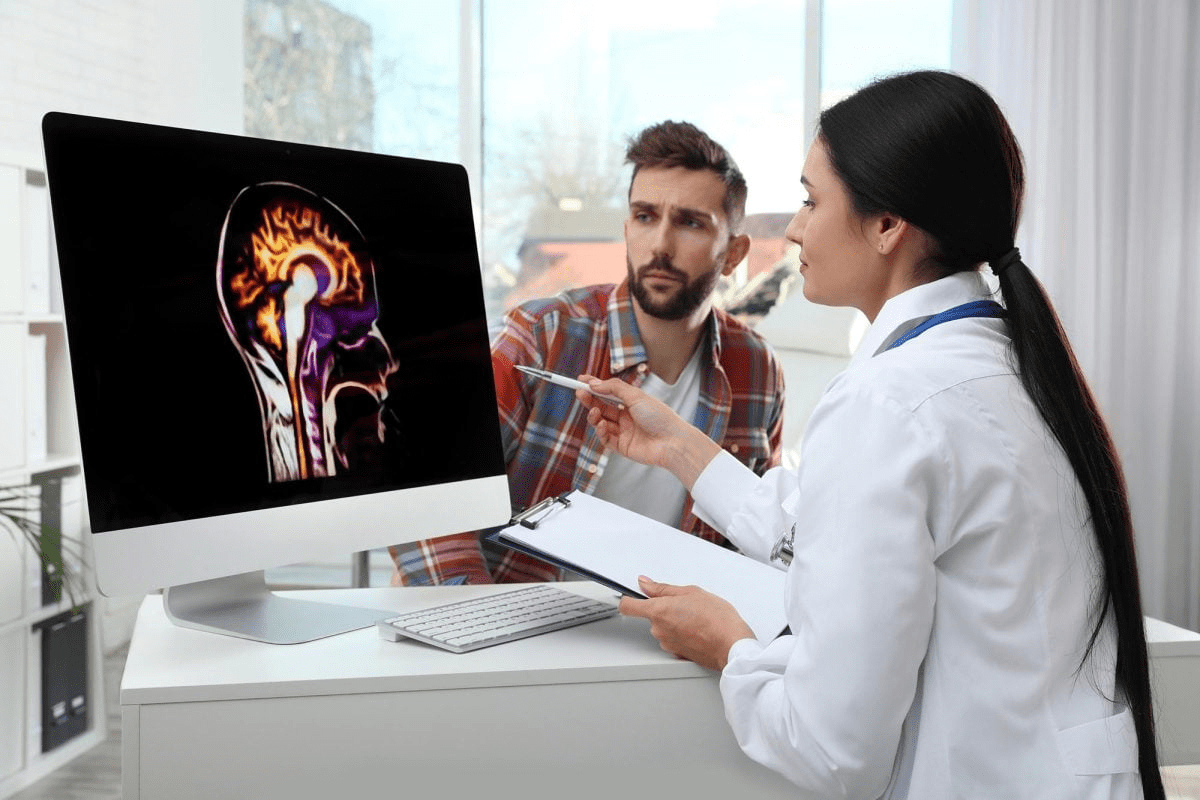
Many cancer patients wonder when they can drink alcohol again after chemotherapy. The answer depends on several things. These include the type of chemotherapy, the patient’s health, and medical guidelines.
Medical Guidelines on Post-Treatment Alcohol Consumption
usually tell patients to avoid alcohol during and right after chemotherapy. The American Cancer Society says patients should talk to their healthcare team about drinking alcohol. There’s no one rule for when it’s safe to drink again. But, most say to wait until you feel better from the treatment’s side effects.
Factors Affecting Safe Alcohol Consumption Timelines
Several things can change when it’s safe to drink alcohol after chemotherapy. These include:
- The type and dosage of chemotherapy drugs used
- The patient’s liver function and overall health
- The presence of any comorbid conditions
- The patient’s age and recovery pace
To understand these factors better, look at the table below:
| Factor | Consideration | Impact on Alcohol Consumption |
| Type of Chemotherapy | Different drugs have varying levels of interaction with alcohol | Some may require longer avoidance of alcohol |
| Liver Function | Liver health affects the body’s ability to process alcohol | Poor liver function may necessitate avoiding alcohol |
| Overall Health | Presence of other health issues can complicate recovery | May require cautious reintroduction of alcohol |
It’s key for patients to talk to their about when it’s safe to drink alcohol again. Each person’s situation is different, and can give personalized advice.
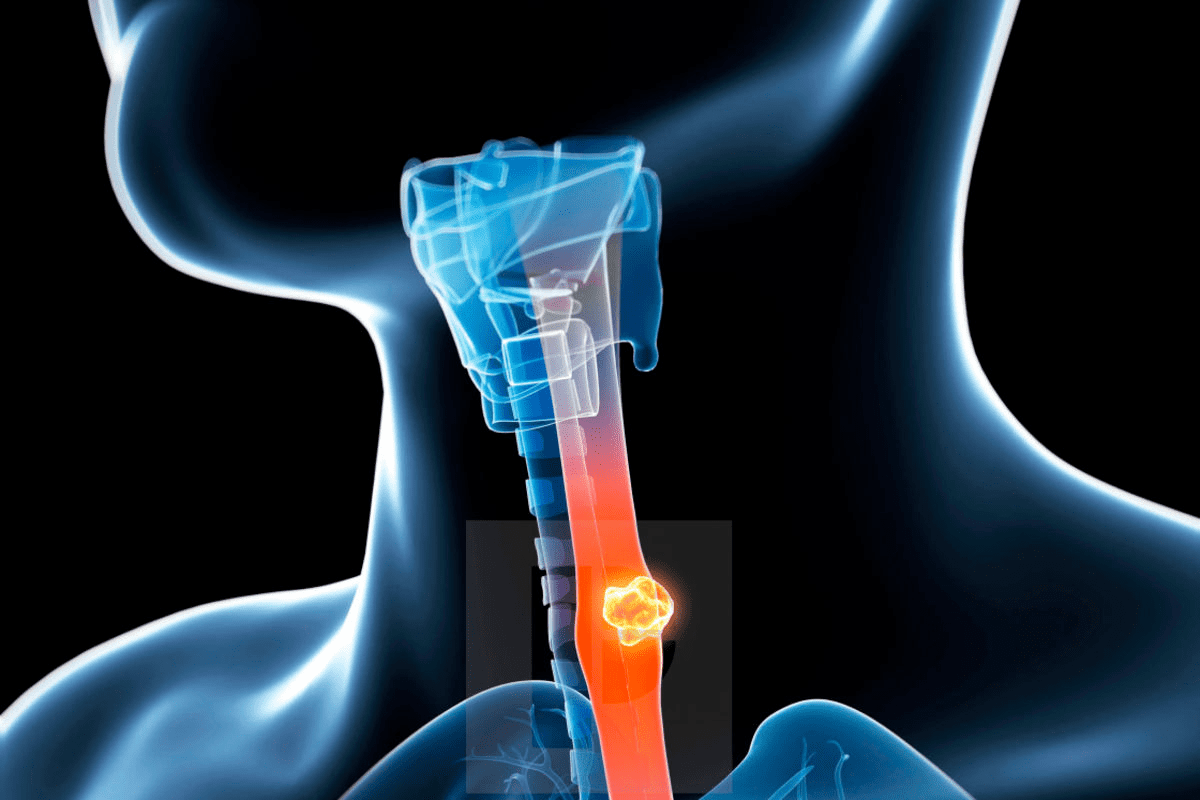
Can You Drink Alcohol While on Chemotherapy?
Patients on chemotherapy need to know if they can drink alcohol. Chemotherapy uses strong drugs to fight cancer. Adding alcohol can make things more complicated.
Potential Interactions Between Alcohol and Chemotherapy Drugs
Alcohol can mix badly with chemotherapy drugs. This can lead to more side effects or less effective treatment. Some chemotherapy drugs might react with alcohol, causing nausea, vomiting, and other issues.
Alcohol can change how chemotherapy drugs work in the body. This can cause unpredictable outcomes. It might make the treatment less effective or more toxic.
What Oncologists Recommend About Alcohol During Active Treatment
Oncologists usually tell patients to stay away from alcohol during chemotherapy. Limiting or completely avoiding alcohol can reduce risks. It helps make sure the treatment works well.
Some oncologists suggest talking about alcohol use with them. They can give advice based on your situation. This helps patients make smart choices about their lifestyle during treatment.
Knowing the risks and listening to can help patients feel safer during chemotherapy. It gives them confidence and safety.
Effects of Alcohol Consumption During Cancer Treatment
Drinking alcohol while on chemotherapy can harm treatment results and health. It’s key to know how alcohol affects chemotherapy drugs and the dangers it poses.
How Alcohol May Intensify Chemotherapy Side Effects
Chemotherapy can cause a lot of side effects, like nausea and tiredness. Drinking alcohol can make these side effects worse, making treatment harder for patients.
- Increased Risk of Nausea and Vomiting: Alcohol can upset the stomach, raising the chance of nausea and vomiting, common with chemotherapy.
- Enhanced Fatigue: Both alcohol and chemotherapy can make you feel very tired. Drinking alcohol while treating cancer can make this feeling worse, affecting your life quality.
- Impact on Liver Function: Chemotherapy already strains the liver. Drinking alcohol can make liver function worse, leading to serious health problems.
Impact on Treatment Efficacy and Recovery
Alcohol can affect how well chemotherapy works and how fast you recover. Studies show alcohol can hinder the body’s recovery from chemotherapy.
| Aspect | Effect of Alcohol | Impact on Chemotherapy |
| Liver Function | Compromised | Reduced ability to process chemotherapy drugs |
| Immune System | Suppressed | Increased risk of infections during treatment |
| Recovery | Slowed | Prolonged recovery times |
In conclusion, knowing how alcohol affects cancer treatment is critical for managing side effects and ensuring chemotherapy works well. Patients should talk to their about drinking alcohol during treatment.
Types of Alcoholic Beverages During Treatment
When you’re going through chemotherapy, it’s important to think about how alcohol might affect your treatment. Drinking alcohol during chemotherapy can be tricky. Many things can change how safe and effective it is.
Wine, Beer, and Spirits: Comparing Effects During Chemotherapy
Alcoholic drinks have different amounts of alcohol and substances called congeners. These can affect how they work with chemotherapy. Wine might have some health benefits, but its effects during treatment are not fully understood. Beer has a different mix and might seem safer to some. Spirits have more alcohol and could be riskier.
“The type of alcoholic beverage may influence the risk of certain health outcomes, but during chemotherapy, the primary concern is the alcohol content and its interaction with treatment.”
It’s important to compare these drinks to understand their possible effects during chemotherapy.
| Beverage Type | Alcohol Content | Potential Interaction with Chemotherapy |
| Wine | 8-15% | May intensify side effects; interaction with certain chemotherapy drugs |
| Beer | 4-7% | Potential for increased risk of infection; impact on treatment efficacy |
| Spirits | 30-50% | Higher risk of dehydration; severe interaction with chemotherapy medications |
Alcohol Content Considerations for Cancer Patients
The alcohol in drinks is a big deal for cancer patients on chemotherapy. Drinks with more alcohol can cause dehydration and make side effects worse. It’s key to know the alcohol in your drinks and how it might affect your treatment.
If you’re wondering, “can you drink beer while on chemo?” or about other drinks during treatment, it’s all about understanding the risks. Always talk to your healthcare team before making choices.
Dining Out During Chemotherapy: Precautions and Tips
To have a safe dining experience during chemotherapy, knowing about food safety in restaurants is key. Chemotherapy weakens the immune system. This makes patients more likely to get sick from food.
Food Safety Considerations When Eating at Restaurants
When eating out, pick restaurants with good food safety ratings. Stay away from buffets or salad bars where food sits out for too long. Choose cooked foods that are hot, and avoid raw meat, poultry, or seafood.
It’s smart to ask your server about food handling. Find out how often utensils and cutting boards are cleaned. Also, ask if foods are stored and reheated correctly.
Best Restaurant Choices During Cancer Treatment
Picking the right restaurant is important. Go for places known for cleanliness and proper food handling. Steer clear of restaurants with food safety issues.
- Choose restaurants that cook food to order.
- Avoid raw or undercooked foods.
- Select restaurants with a high customer turnover to minimize the risk of food sitting out too long.
By keeping these tips in mind, people going through chemotherapy can enjoy dining out safely. This helps reduce the risk of getting sick from food.
Public Spaces and Chemotherapy: Managing Infection Risks
For those getting chemotherapy, public spaces can be risky. The treatment weakens the immune system. This makes it harder to fight off infections.
Navigating Crowded Venues
Crowded places like buses, malls, and theaters can spread infections. To stay safe, follow these tips:
- Avoid touching your face, like your eyes, nose, and mouth.
- Wear a mask to catch airborne germs.
- Keep a distance of at least 6 feet from others.
Seasonal Considerations for Public Outings
Seasons change, and so do the risks for chemotherapy patients. For example, flu season is a big risk. Knowing these risks helps plan safer outings.
| Season | Infection Risks | Precautions |
| Winter (Flu Season) | Higher risk of flu and other respiratory infections | Get a flu shot, wear a mask, avoid crowded areas |
| Summer | Increased risk of gastrointestinal infections | Practice good hygiene, avoid undercooked foods |
Being aware of these risks and taking steps can help manage infection risks in public spaces.
Chemotherapy Precautions for Family Members at Home
Family members can greatly support their loved ones during chemotherapy by taking precautions at home. It’s important to create a safe and supportive environment. This helps the patient recover and keeps the whole household well.
Household Hygiene Practices During Treatment
Good hygiene is key when living with someone getting chemotherapy. Frequent handwashing is a simple yet effective way to stop infections. Family members should wash their hands with soap and water often. This includes after using the bathroom, before eating, and after coughing or sneezing.
Cleaning and disinfecting surfaces is also important. Focus on areas like doorknobs, light switches, and countertops. Using a cleaner that fights many viruses and bacteria can help keep everyone safe.
Special Considerations for Children and Pets
Chemotherapy affects children and pets too. Teach kids to wash their hands often and stay away from the patient if they’re sick. Limiting visitors also helps prevent infections.
Pets can offer comfort to patients. But, family members should take turns caring for them. This reduces the patient’s risk of getting sick. Keeping pets clean and up-to-date on shots is also important.
By following these steps and staying open, family members can make a safe and caring space for their loved one.
Can You Have Visitors During Chemotherapy?
Visitors during chemotherapy can offer comfort, but there are risks. Chemotherapy weakens your immune system, making you more likely to get sick. It’s key to find a balance between staying connected and keeping healthy.
Setting Boundaries with Friends and Family
It’s important to set boundaries with friends and family during chemotherapy. Communicate your needs clearly to them. Let them know when you’re ready for visitors and when you need time alone.
Ask them to call before visiting to make sure you’re ready. Also, teach them how to avoid infections. For example, they should wash their hands often and stay away if they’re sick. This way, you can enjoy their company while keeping your health safe.
When to Limit Social Interactions
There are times when it’s best to limit visitors to avoid getting sick. For example, when you have neutropenia (low white blood cell count), your body can’t fight off infections as well. It’s important to stay away from crowded places and people who are sick.
If you’re feeling very tired or have other side effects, it’s okay to limit visitors. Taking care of your health is the most important thing right now. Your loved ones should understand and respect your needs.
Being aware of when to limit visitors and how to set boundaries helps you manage chemotherapy. You can keep meaningful connections with those around you while staying healthy.
Alternative Beverages During Cancer Treatment
Hydration is very important during chemotherapy. Choosing the right drinks is key. Cancer patients need to drink enough to stay healthy and help their treatment work better.
Hydration Importance During Chemotherapy
Drinking enough water is vital during chemotherapy. It helps your body handle the drugs and lowers side effect risks. Adequate hydration also helps with fatigue and dry mouth.
Cancer patients should drink lots of fluids, aiming for eight to ten glasses a day. But, the right amount can vary based on your needs, how active you are, and your treatment plan.
Beneficial Drinks for Cancer Patients
While water is best, there are other good drinks for chemotherapy patients. These include:
- Herbal teas, which are soothing and hydrating without caffeine.
- Clear broths, which help with hydration and give important salts.
- Fruit juices, which have vitamins, but choose ones low in sugar.
- Electrolyte-rich beverages, which keep electrolyte levels balanced in the body.
Coffee and caffeine are also topics of interest. While some caffeine is okay, be careful. It can make dehydration worse and affect some chemotherapy drugs.
Coffee, Caffeine, and Chemotherapy: What to Know
Knowing how caffeine affects you during chemotherapy is key for coffee lovers. Chemotherapy is tough on the body and raises many questions about what to eat or drink. It’s important to understand what’s safe during this time.
Research on Caffeine Consumption During Cancer Treatment
Many studies have looked into caffeine and chemotherapy. Most say moderate caffeine is okay for most people. But, how much you can handle can differ a lot. Always talk to your for advice tailored to you.
Caffeine can change how some chemotherapy drugs work. It might make them less effective or increase side effects. For example, it can make your liver process drugs differently, leading to more toxicity.
Moderation Guidelines for Coffee Lovers
If you’re having chemotherapy and want to keep drinking coffee, be careful. The American Cancer Society says up to 3-4 cups a day is usually okay. But, it depends on how your body reacts and your treatment plan.
Watch how your body reacts to caffeine. If you feel jittery, anxious, or your heart beats faster, you might need to drink less. It’s all about listening to your body.
Remember, coffee has antioxidants that are good for you. But, always follow your advice on what to eat and drink while you’re being treated.
Engaging Activities That Support Recovery
Doing activities that help with recovery can make chemotherapy better. These activities give emotional comfort and keep you feeling connected to the world.
Low-Risk Social Activities Recommended During Chemotherapy
It’s key to keep social life balanced with health during chemo. Low-risk social activities are safe and don’t tire you out. Here are some:
- Having a video call with friends or family
- Enjoying a quiet dinner at home with loved ones
- Participating in online communities or forums for cancer patients
Creative Ways to Stay Connected While Protecting Your Health
Staying in touch with others is important for your mood during chemo. Creative activities keep you engaged and safe. Try these:
- Writing letters or emails to friends and family
- Creating art or crafting at home
- Watching movies or TV shows and discussing them online
These activities help you stay connected while you’re getting treatment. They support your mental and emotional health.
When to Resume Normal Activities After Completing Chemotherapy
Finishing chemotherapy is a big step in fighting cancer. But, the healing doesn’t stop there. Knowing when to start doing normal things again is key to getting back to life safely.
Timeline for Returning to Regular Social Life
How long it takes to get back to social life varies. It depends on the cancer type, how strong the chemotherapy was, and the patient’s health. Most people are told to slowly get back to doing things over weeks or months.
A study in the Journal of Oncology found most people can get back to normal in 3 to 6 months after chemotherapy. But, everyone heals at their own pace.
| Activity Level | Typical Recovery Time | Guidelines |
| Light Activities (e.g., short walks) | 1-3 weeks | Start with short sessions and gradually increase duration |
| Moderate Activities (e.g., household chores) | 3-6 weeks | Listen to your body and rest when needed |
| Strenuous Activities (e.g., intense exercise) | 6-12 weeks or more | Consult with your healthcare provider before resuming strenuous activities |
Monitoring Your Body’s Signals During Recovery
It’s important to listen to your body while recovering. Watch for signs of tiredness, pain, or other symptoms that mean you’re doing too much. Change what you’re doing to keep safe.
Key indicators to watch for:
- Unusual fatigue or weakness
- Increased pain or discomfort
- Shortness of breath or dizziness
- Fever or signs of infection
If you notice these signs, talk to your . They can help you figure out how to manage them and adjust your recovery plan.
Conclusion: Balancing Quality of Life and Safety During Cancer Treatment
When you’re going through cancer treatment, like chemotherapy, you need to think about your daily life. It’s important to keep a balance between enjoying life and staying safe. Chemotherapy weakens your immune system, making you more likely to get sick.
It’s also key to be careful about social activities and drinking alcohol while on chemotherapy. Following advice is vital to avoid risks. Drinking alcohol can make treatment side effects worse and interact badly with your drugs.
To stay safe, try to avoid crowded places and keep your home clean. Be careful with what you eat and drink. Choosing safer drinks and activities can help you recover well and enjoy life.
Finding a balance is the main goal in cancer treatment. It’s about staying connected with friends and family while keeping your health safe. By knowing what precautions to take, you can make choices that keep you safe and happy.
FAQ
Can you drink alcohol while on chemotherapy?
No, it’s not a good idea to drink alcohol during chemotherapy. It can make side effects worse and affect how well the treatment works.
Can you have visitors during chemotherapy?
Yes, you can have visitors, but set limits when you’re not feeling well. Tell them to avoid getting you sick. It’s important to keep your immune system strong.
What are the precautions for family members at home during chemotherapy?
Family members should keep the house clean and stay healthy. Avoid close contact when sick. This is important, even more so with kids and pets around.
Can you drink beer while on chemotherapy?
No, it’s not safe to drink beer or any alcohol during chemotherapy. It can react with your treatment and make side effects worse. The type of drink doesn’t matter.
How long should you stay away from people after chemotherapy?
How long to stay away from people varies. It depends on your health and how your treatment affects your immune system. Try to avoid crowded places and sick people until you’re better.
Can cancer patients drink coffee during chemotherapy?
You can have coffee in small amounts during chemotherapy. But, talk to your oncologist first. Too much caffeine can be bad.
What are some beneficial drinks for cancer patients during chemotherapy?
Drinking plenty of water is key during chemotherapy. Also, clear broths and drinks with electrolytes are good. But, avoid too much sugar and caffeine.
Can you drink alcohol during radiation therapy?
It’s best to avoid alcohol during radiation therapy. It can increase side effects and affect treatment success.
What are some low-risk social activities during chemotherapy?
You can stay connected with loved ones through phone calls, video chats, or online groups. Also, enjoy hobbies that don’t risk getting you sick.